Chapter: Biology of Disease: Disorders of the Gastrointestinal Tract, Pancreas, Liver and Gall Bladder
Disorders of the Liver, Gall Bladder and Bile Duct
DISORDERS OF THE LIVER, GALL BLADDER AND BILE DUCT
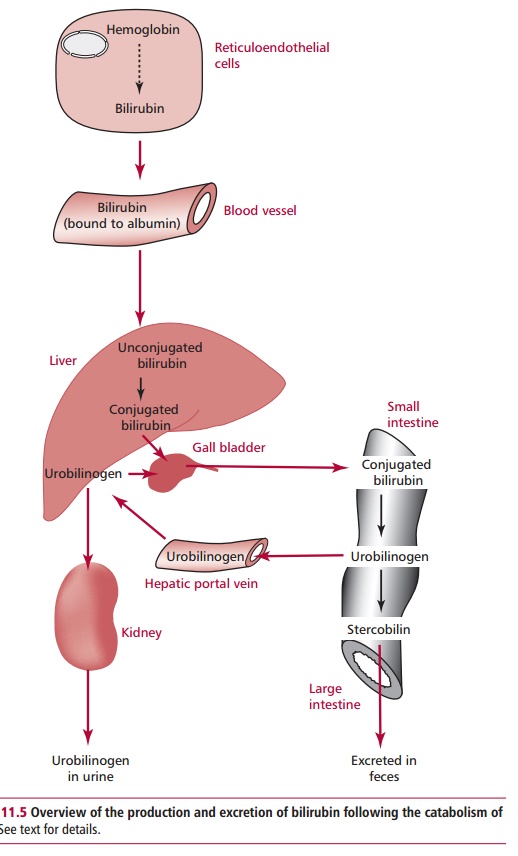
Jaundice is the yellow discoloration of tissues due to an
accumulation of bilirubin (Figure 11.5).
Many disorders of the liver give rise to jaundice, although clinical jaundice
may not be seen until the concentration of bilirubin in the serum is greater
than 50 µmol dm–3. The causes of jaundice can be pre-hepatic,
hepatic or posthepatic.
The causes of prehepatic jaundice include hemolysis, where there
is an increased breakdown of hemoglobin producing large amounts of bilirubin
that overloads the conjugating mechanism. Such bilirubin is mostly uncon- jugated
and commonly occurs in newborn babies. If the concentration of serum bilirubin
approaches 200 µmol dm–3, then phototherapy is used to degrade it, otherwise its high
concentra-tion may cause damage to the brain called kernicterus. Other causes of pre-hepatic hyperbilirubinemia include
hemolytic disease of the newborn due to Rhesus incompatibility and ineffective
erythropoiesis, which occurs in pernicious anemia . The commonest causes of
hepatic hyperbilirubinemia are viral hepatitis and paracetamol (acetaminophen)
poisoning . There is also physiological jaundice of the newborn, a mild
unconjugated hyperbilirubinemia that develops because of low activ-ity of
UDP-glucuronyltransferase, following birth. Activity increases within two weeks
and the jaundice disappears. Other causes include Gilbert’s and Criggler-Najjar
syndromes. In Gilbert’s syndrome, the affected individuals have an inherited
partial deficiency of hepatic UDP-glucuronyltransferase. Patients present with
a mild jaundice and occasionally suffer from abdomi-nal discomfort but
otherwise the condition is harmless. Fasting, infection, stress and excessive
alcohol intake may aggravate the symptoms. Treatment of Gilbert’s syndrome is
by administration of phenobarbitone to stimulate glucuronyltransferase
activity. Criggler-Najjar syndrome is a rare hereditary disorder characterized
by a complete absence of glucuronyltransferase activ-ity from birth. Patients
suffer from severe unconjugated hyperbilirubinemia. Treatment using
phototherapy in affected newborns may temporarily reduce the unconjugated hyperbilirubinemia
but infants generally die within one year of birth.
One of the causes of posthepatic hyperbilirubinemia is cholestasis where there is failure of
bile to reach the small intestine. Cholesterol is virtually insoluble in water
and is maintained in an aqueous environment in vesicles combined with
phospholipids and bile salts. In normal conditions, the vesicles maintain the
concentration of cholesterol in bile near its saturation point. Cholesterol
monohydrate crystals form when the ratio of cholesterol, phospholipids and bile
salts exceeds the normal range and results in the formation of gallstones in a
process termed cholelithiasis.
Eighty per cent of gallstones are composed largely of cholesterol; the
remaining 20% consist of calcium and bilirubin. They vary in size from that of
a grain of sand to the diameter of a golf ball. In many cases, the smaller
stones can be excreted in the bile duct without caus-ing harm. Larger
gallstones usually cause abdominal pain and are so large that they obstruct the
flow of bile into the small intestine. However, in some cases gallstones may
exist for years without causing any symptoms. When there is a complete
blockage, there is little or no urobilinogen in the feces, which are pale
colored due to absence of stercobilinogens. When the block-age is removed,
urobilinogen becomes detectable in the urine and the feces regain their normal
color. Occasionally intrahepatic obstruction arises where a blockage affects
the bile canaliculi in liver cirrhosis or cancer . This type of blockage causes
an increase in the concentration of conjugated bilirubin in the serum.
It is essential to determine whether the cause of the increased
amounts of conjugated bilirubin is intra- or extrahepatic because it is of
diagnostic signif-icance and determines the subsequent treatment. The degree of
obstruction to the flow of bile is usually greater in extrahepatic cholestasis.
Extrahepatic cholestasis may benefit from surgery to remove the gall bladder or
to remove the gallstone. Nonsurgical treatments are preferred because surgery
can be hazardous. Oral dissolution therapy with ursodiol and chenodiol, which
are derived from bile salts, is effective in treating small, predominantly
choles-terol gallstones. Treatment may be required for months to years before
the gallstones are dissolved but is preferred in patients who cannot undergo
sur-gery. In some cases, gallstones may be broken down using ultrasound waves
to smaller particles that can easily be excreted.
Acute hepatitis is caused by infection and subsequent
inflammation of the liver, where liver cells are destroyed and the liver
becomes necrotic. The com-monest cause is viral infections, for example with
hepatitis A, B, C, D and E viruses, although drugs, toxins and autoimmune
reactions can also lead to acute hepatitis. The initial symptoms of acute viral
hepatitis include malaise, anorexia, fever, rashes, abdominal pain, dark urine
and jaundice.
Hepatitis A virus causes a mild hepatitis where patients recover
usually with no complications. The virus is transmitted by contaminated food or
drink, especially where sanitation is poor. Following an incubation period of
15 to 40 days, the patient develops fever, sickness and, shortly afterwards,
jaun-dice. Hepatitis B virus is more serious with a mortality rate of 5–20%
although most patients gradually recover. Hepatitis B virus spreads from one
person to another via body fluids, such as blood, saliva, semen, vaginal
fluids, tears, breast milk and urine. Transmission may occur during sexual
activity with an infected person and vertically from an infected mother to the
baby. It is commonly present in drug addicts. The symptoms develop suddenly
after an incubation period of one to six months and include fever, chills,
weakness and jaundice. In contrast to other types of hepatitis, more than 80%
of hepa-titis C virus (HCV) infections cause chronic liver disease.
Approximately 170 million people worldwide may be infected with HCV. This
infection is mild in the early stages and is often only diagnosed when it has
already caused severe liver damage. For this reason, infection with HCV has
been referred to as the ‘silent epidemic’. Blood transfusions were the commonest
means of transmission prior to the testing of blood products for HCV.
Infections with hepatitis B and C viruses are associated with liver cancer .
The hepatitis D virus occurs only with or after infection with hepatitis B
virus and its mode of transmission is identical to that of the B virus.
Hepatitis E was ini-tially grouped as a type C virus. It occurs in people who
have been to parts of the world where this virus is endemic, such as India. It
is transmitted by water contaminated with fecal material.
A clinical history of recent blood transfusions or intravenous
drug use may all suggest acute hepatitis. Blood tests based on antigen–antibody
reactions are conducted to establish the type of virus causing the hepatitis.
Many patients present with proteinuria and bilirubinuria and show increased
levels of serum alkaline phosphatase (ALP) activity. A liver biopsy will
confirm the initial diag-nosis. The HCV is treated with @-interferon , otherwise patients are advised to take
plenty of bed rest with adequate food and fluid intakes. A serious complication
of many cases of acute hepatitis is the development of chronic hepatitis.
Chronic hepatitis is an inflammation of the liver that persists
for more than six months without improvement. Its causes include autoimmune
liver dam-age, chronic infection with hepatitis B virus and excessive drug and
alcohol use. Chronic hepatitis can be divided into two histological types,
namely, chronic persistent hepatitis, which has a good prognosis, and chronic
active hepatitis that may respond to immunosuppressive or antiviral agents but often
progresses to cirrhosis, leading to death within five years as a result of
liver failure.
Cirrhosis is a condition where the liver responds to injury or
death of some of its cells by producing strands of fibrous tissue between which
are nodules of regenerating cells. Patients with cirrhosis may be asymptomatic
for a long period of time before vague symptoms such as nausea, vomiting,
anorexia, weakness, weight loss and edema of the legs become apparent. Its
clinical complications include jaundice, ascites,
which is an abnormal accumulation of fluid in the abdomen, GIT bleeding and
hepatic encephalopathy. Cirrhosis may interfere with intrahepatic circula-tion
causing gradual failure of liver function. Cirrhosis can be divided into three
types, namely, alcoholic, postnecrotic and biliary cirrhosis. Alcoholic
cirrhosis is discussed.
Postnecrotic cirrhosis accounts for about 25% of all cases of
cirrhosis and is associated with viral infections, the use of certain drugs and
poisons. About 25% of postnecrotic cirrhosis cases have a prior history of
viral hepatitis. Unfortunately 75% of all patients with postnecrotic cirrhosis
die within one to five years. Biliary cirrhosis accounts for approximately 15%
of all cases of cir-rhosis and is characterized by the death of liver cells
surrounding bile ducts. It is most commonly caused by an obstruction of the bile
duct leading to an accumulation of bile within the liver.
Diagnosis of cirrhosis will involve palpation and X-ray of the
abdomen, which often reveal an enlarged liver. A liver biopsy is required to
confirm the diag-nosis. Other laboratory tests may reveal anemia or
hyperbilirubinemia and liver function tests (LFTs) determine increases in the
activities of a number of enzymes (see
below). There are no drugs that can arrest or reverse the fibrotic process
in cirrhosis and treatment is aimed at dealing with the underlying cause, for
example alcohol abuse or biliary obstruction and by treating any complications.
A number of plasma enzyme activities are used to assess liver
function, including those of aspartate transaminase (AST), alanine transaminase
(ALT), alkaline phosphatase (ALP) and F-glutamyltranspeptidase (GGT). Alanine transaminase is present
in both the cytosol and mitochondria of hepatocytes whereas ALT is found only
in the cytosol. Liver cell damage releases these enzymes increasing their
levels in the plasma. Alanine transaminase is specific for the liver whereas
AST is also found in pancreatic and skeletal and cardiac muscle tissues. In
hepatocellular damage, levels of AST and ALT may increase tenfold but in
obstructions of the bile duct or cholestasis, the increases may be relatively
slight, usually no more than two to three times their normal levels. Alanine
transaminase and AST measurements are useful in monitoring the progress of
hepatocellular damage where falling levels suggest an improve-ment in the
disease. Alkaline phosphatase is found on the surface of hepato-cytes and in
the microvilli of bile ducts but is not specific for liver. Its activity is
increased in cholestasis. In hepatocellular disease, ALP levels may be normal
or slightly raised. Falling plasma levels of ALP suggest a correction of
cholestasis and may be useful for monitoring this defect. Plasma GGT levels are
raised in both hepatocellular disease and cholestasis. Although the test for
this enzyme is sensitive, it is not specific for liver disease as its activity
is increased by some drug therapies and by alcohol. The blood protein albumin
is synthesized in the liver and its concentration in plasma reflects the
functional capacity of the liver. Plasma albumin concentration is low
in chronic liver disease but tends to be normal in the early stages of acute
hepatitis.
Related Topics