Chapter: Medicine and surgery: Cardiovascular system
Wolff-Parkinson-White syndrome - Junctional arrhythmias
Wolff-Parkinson-White syndrome
Definition
Congenital predisposition to recurrent supraventricular tachycardia due to the presence of an extra accessory pathway between the atria and the ventricles.
Aetiology
Abnormal connection between atrium and ventricle (e.g. bundle of Kent) that allows quick conduction from the atria to the ventricles bypassing the AV node. Half of patients have a tachycardia either due to reentry or atrial fibrillation.
Pathophysiology
Normally the fast conduction through the bundle of Kent allows the adjacent area of ventricle to be rapidly depolarised (preexcitation), whilst the remainder of the ventricle is depolarised by the normal route. However, the two pathways may form a re-entry circuit with the fast accessory pathway causing a retrograde stimulation of the atria and hence the AV node. The result is a form of paroxysmal supraventricular tachycardia.
Clinical features
In sinus rhythm WolffŌĆōParkinsonŌĆōWhite syndrome is asymptomatic. Patients may experience paroxysms of
Investigations
During sinus rhythm the rapid conduction through the accessory pathway causes a short PR interval (<0.12 seconds) and a wide QRS complex beginning with a slurred part known as a ╬┤ wave (see Fig. 2.8).
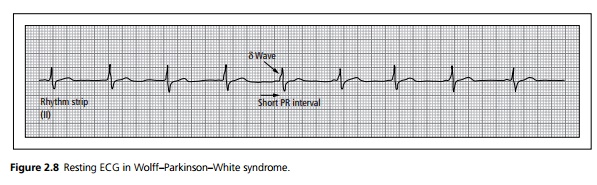
During a tachycardic episode, the conduction enters the ventricle through the AV node thus the PR interval and QRS morphology return to normal. Retrograde excitation of the atria causes abnormal P waves following the QRS complex.
Complications
Sudden cardiac death may rarely occur if atrial fibrillation occurs. This leads to ventricular fibrillation because the accessory pathway can conduct rapid impulses without the usual blocking effect of the AV node, leading to sudden death.
Management
Re-entrant tachycardias are treated with drugs that block retrograde conduction through the accessory pathway, e.g. disopyramide, propanolol or amiodarone. Verapamil and digoxin are contraindicated as they accelerate anterograde conduction through the accessory pathway.
Symptomatic patients should be offered a specialist evaluation for radioablation of the accessory pathway.
Prognosis
With age the pathway may fibrose and so some patients ŌĆśgrow out of ŌĆÖ the condition.
Related Topics