Chapter: Clinical Cases in Anesthesia : Transurethral Resection of the Prostate
What other complications can occur during a TURP?
What other complications can occur during a TURP?
Approximately 7% of all patients undergoing a
TURP suffer a major complication. The 30-day mortality rate has been estimated
to be 0.1–0.8%. This is a marked improve-ment over earlier studies that showed
a mortality rate of approximately 2.5% during the 1960s. Patients undergoing a
TURP are often advanced in age, and have coexisting cardiopulmonary disorders
making them more likely to experience complications. Since many patients are on
chronic diuretics, they are often dehydrated with electrolyte abnormalities
preoperatively.
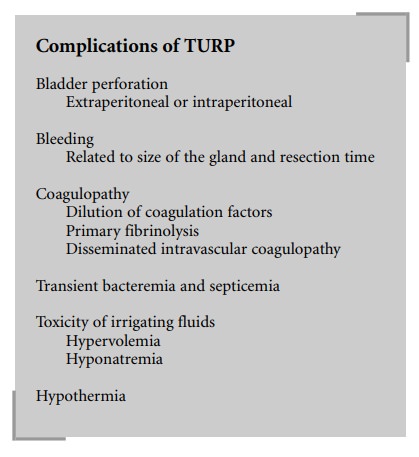
Other complications associated with this
procedure are as follows:
Bladder Perforation
Bladder perforation occurs in approximately 1%
of all TURP procedures. It may be caused by overdistention of the bladder with
irrigating fluid, or as a result of surgical instrumentation. An early sign of
bladder perforation is a decrease in return of irrigating fluid from the
bladder. The abdomen will become distended and often rigid. If the procedure is
being performed under a regional anesthetic, the patient may complain of pain
and/or experience nausea and vomiting. Hypotension followed by hypertension is
common.
Most perforations are extraperitoneal and
benign in nature. This type of perforation causes pain in the periumbilical
region. However, pain in the upper abdomen or referred pain to the shoulder may
be a sign of an intraperitoneal perforation, a potentially fatal compli-cation.
Diagnosis should quickly be confirmed by cysto-urethrography and treated with a
suprapubic cystostomy.
Bleeding
The prostate is a highly vascular organ. Since
a large amount of irrigation is used, it is difficult to determine the actual
blood loss. Intraoperative blood loss corresponds to the size of the gland as
well as to the resection time. It has been estimated that the blood loss is
approximately 2–5 ml/min of resection time and 20–50 ml/g of prostate tissue.
Blood loss is linearly related to prostate size up to 35 grams, at which point
blood loss tends to exceed the linear correlation. Patients with resection
times of greater than 90 minutes or a prostate size of more than 60 grams have
been found to have a significant increase in morbidity associated with
bleeding.
Coagulopathy
Subclinical coagulopathy occurs in
approximately 6% of patients undergoing a TURP, while clinical coagulopathy
occurs approximately 1% of the time. This condition seems to correlate with the
mass of the resected prostatic tissue. It is more likely to occur if the
resected tissue is greater than 35 grams. Coagulopathy may be due to a dilution
of coagulation factors and platelets.
Primary fibrinolysis has also been implicated
as a cause of coagulopathy. Plasminogen activator, which is responsi-ble for
converting plasminogen into plasmin, is released during these procedures. The
treatment of choice for primary fibrinolysis is ε-aminocaproic acid.
Secondary fibrinolysis may occur as a result of
dissemi-nated intravascular coagulopathy (DIC). DIC is caused by the systemic
absorption of prostate tissue, which is rich in thromboplastin. Proof of this
theory lies in the fact that these patients often have a low level of
plasminogen activa-tor, platelets, and fibrinogen – common findings in DIC. If
DIC is suspected, the treatment is symptomatic. Fluid and blood products are
administered as needed. Heparin administration may be beneficial.
Transient Bacteremia and Septicemia
The prostate, rich in bacteria, may cause a
postoperative bacteremia via the prostatic venous sinusoids. An indwelling
urinary catheter will enhance the risk. Approximately 6–7% of patients will go
on to develop sepsis. Treatment consists of antibiotics and supportive care.
Toxicity of Irrigating Fluids
The major toxicity of the irrigation fluids
used today is secondary to massive absorption causing fluid overload,
hyponatremia, and hypo-osmolality. The incidence of hypo-osmolality and its
associated neurologic sequelae has decreased since the use of nonelectrolyte
iso-osmotic irri-gating fluids. However, fluid overload and hyponatremia still
remain a problem. As much as 8 liters of irrigating fluid may be absorbed
during a TURP, causing an average weight gain of about 2 kg. Twenty to thirty
percent of this fluid is absorbed directly into the vascular space. The
remainder is absorbed into the periprostatic and the peri-toneal space
(interstitial space). Several factors contribute to the rate of absorption of
irrigating fluid by the patient. These include the prostate size, integrity of
the prostatic capsule, and the height of the irrigating fluid container.
Greater amounts of irrigating fluid are absorbed when the prostate is large
because of its richer blood supply, and if the prostate capsule is violated.
There are maneuvers that may be carried out to
limit the amount of irrigating fluid absorbed. The first is to restrict the
height of the fluid container above the surgical field. This will decrease the
hydrostatic pressure driving the fluid into the sinuses. When the height of the
bag is greater than 60 cm, absorption is greatly enhanced. The sec-ond is to
limit the length of the resection time to less than 150 minutes, as some
investigators have found that 10–30 cc of irrigation fluid is absorbed per
minute of resection time.
Sorbitol and mannitol, both sugar alcohols,
have been associated with the development of lactic acidosis and
hyper-glycemia. Specific effects of glycine will be discussed later.
Hypothermia
Patients may develop hypothermia under either
general or neuraxial anesthesia. This can be exacerbated by using irrigating
fluids at room temperature. Using warmed
It is a theoretical concern that warming the irrigating fluids would
cause vasodilation, thereby increasing blood loss. However, this has not been
shown to be a clinical concern. In fact, since hypothermia may cause shivering,
which increases venous pressure, there may be an increased blood loss if the
irrigating fluids are not warmed.
Related Topics