Chapter: Clinical Cases in Anesthesia : Shock
What are the treatment options for each of the discussed dysrhythmias? What would you do for this patient?
What are
the treatment options for each of the discussed dysrhythmias? What would you do
for this patient?
Complete discussion of all the treatment
options for every dysrhythmia is beyond the scope of this discussion.
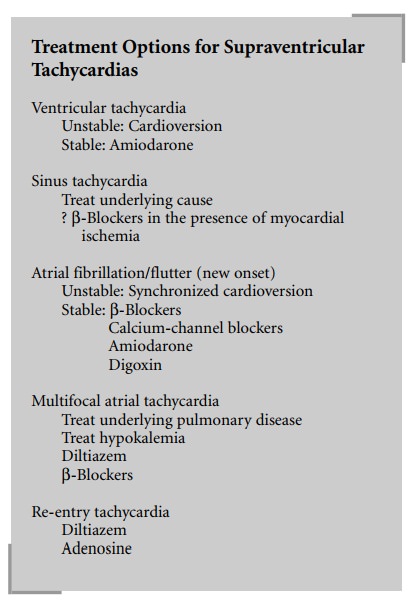
Sinus tachycardia should be treated by
identification and correction of the underlying cause (e.g., hypovolemia,
hypoxemia, anemia, pain, side-effect of medication). In the absence of a
treatable cause in a patient at risk for developing ischemia from the
tachycardia, a trial of β-blocker administration may be warranted. A
short-acting agent such as esmolol should be used so that the therapy may be
rapidly stopped if side-effects, such as hypotension, supervene.
In patients who develop new-onset atrial
fibrillation or flutter complicated by significant hypotension, congestive
heart failure, or ischemia, synchronized
cardioversion start-ing at 100 joules (J) (50 for flutter) is the therapy of
choice.
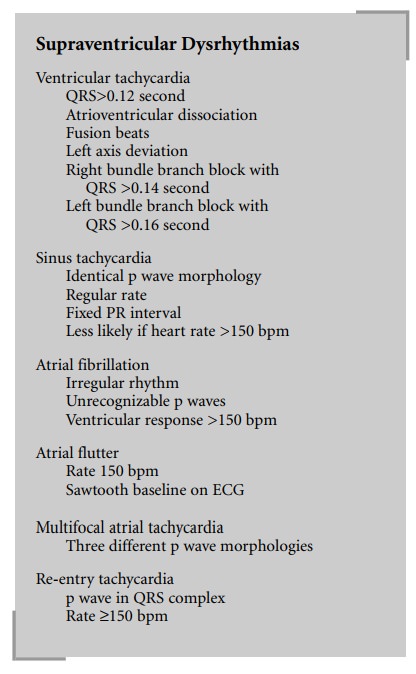
In the absence of such life-threatening
side-effects, chemi-cal conversion to sinus rhythm may be accomplished with:
· β-Blockers: Metoprolol 5 mg intravenously (IV), repeat q5 min up to 25 mg.
· Calcium-channel
blockers: Diltiazem, 5–10 mg IV q5 min up to 30 mg, is usually preferred over
verapamil, 5 mg IV, because it is less of a negative inotrope.
· Amiodarone:
load with 150 mg IV over 10 minutes, then 1 mg/min IV for 6 hours followed by 0.5
mg/min for 18 hours.
· Digoxin:
0.5 mg IV, then 0.25 mg IV q6h × 2; additional 0.25 mg doses can be given if the rate is not controlled. It is
effective in controlling the rate, but equivalent to placebo for conversion to
sinus rhythm. Digoxin will generally require a minimum of 30 minutes to have an
effect but it is hemodynamically well tolerated. The other agents will act
within minutes of administration but may cause hypotension.
Re-entry (“paroxysmal supraventricular”)
tachycardia is treated like atrial flutter but will more often convert to sinus
rhythm when treated with intravenous diltiazem. Intravenous adenosine (6 mg IV
push, then 12 mg up to 2 times) may also be used, but because of its very short
half-life, the rhythm may quickly revert to the re-entry tachycardia.
Multifocal atrial tachycardia usually results
from a primary respiratory problem such as decompensated chronic obstructive
pulmonary disease. Treatment should be aimed at the underlying cause, most
often hypoxemia and/or hypokalemia, although rate control can sometimes be
achieved by administration of intravenous diltiazem or β-blockers.
Unstable patients with ventricular tachycardia
should immediately be cardioverted (start with 100 Joules), whereas stable
patients should be given intravenous amiodarone (150 mg IV infusion over 10
minutes). Wide complex dysrhythmias that cannot be clearly identified as
aberrantly conducted supraventricular dysrhythmias should not be treated with
calcium-channel blockers because these can lead to intractable cardiac arrest
if given to patients with ventricular tachycardia. In this context, adenosine
given for diagnostic purposes is no longer recommended. Untreated ventricular
tachycardia will usually deteriorate into ven-tricular fibrillation, which
should be immediately treated with DC defibrillation starting with 200 Joules.
If a defib-rillator is not immediately available, a precordial thump can be
used in an attempt to restore sinus rhythm. If this fails, cardiopulmonary
resuscitation (CPR) should be initi-ated until defibrillation is possible.
In this patient’s case, the main diagnoses are
ventricular tachycardia, aberrantly conducted atrial fibrillation with rapid
ventricular response, or paroxysmal supraventricular tachycardia. Since the
dysrhythmia is poorly tolerated, immediate synchronized
cardioversion should be attempted, starting with 100 J and increasing to 200,
300, then 360 J if needed. Amiodarone is probably the drug of choice to prevent
recurrence, since it will be effective both on ven-tricular tachycardia and on
supraventricular dysrhythmias.
Most defibrillators automatically revert to the
nonsyn-chronized mode after a synchronized shock is delivered, in order to
permit immediate defibrillation should ventricular fibrillation result. One
should not forget to select the syn-chronized mode again if the original
dysrhythmia persists or recurs, in order to prevent “R on T” phenomenon leading
to ventricular fibrillation.
Remember to avoid calcium-channel blockers (as
well as adenosine) in patients with pre-excitation syndromes such as
Wolff-Parkinson-White syndrome who develop atrial fibrillation, because of the
risk of increased conduc-tion through the accessory pathway causing ventricular
fibrillation.
Related Topics