Chapter: Clinical Cases in Anesthesia : Congenital Heart Disease
What are the common right-to-left shunting lesions with reduced pulmonary blood flow?
What are
the common right-to-left shunting lesions with reduced pulmonary blood flow?
Tetralogy of Fallot (TOF)
The combination of VSD, pulmonary valvular
and/or right ventricular infundibular stenosis, right ventricular hypertrophy,
and a large overriding aorta is known as TOF. It is the most common cyanotic
defect seen after the first year of life, contributing to 10% of all congenital
cardiac lesions. The degree of right ventricular outflow and/or pul-monic
obstruction determines the onset and severity of cyanosis. With severe
obstruction, cyanosis appears with closure of the ductus arteriosus in the
neonatal period. Prostaglandin E1 may be used to clinically
stabilize the patient prior to surgical intervention. Many infants do not
develop symptoms until 3–6 months of age and even then may not appear cyanotic
at rest. However, episodes of severe cyanosis with hyperventilation and
acidosis, known as hypercyanotic spells (or “tet” spells), may occur. These are
caused by severe infundibular spasm, probably induced by changes in venous
return and SVR. Reduction in SVR leads to decreased pulmonary blood flow, since
blood tends to be shunted to the systemic circulation. Decreased venous return
further decreases pulmonary blood flow. In older children, the squatting
posture may improve symptoms through an increase in venous return from the
lower extremities and by increasing SVR. The treatment of hypercyanotic spells
is based on the goals of decreasing infundibular spasm by decreasing
contractility and heart rate, and by increasing preload. Another goal
(especially in fixed right ventricular outflow obstruction) is to increase SVR
to decrease right-to-left shunting across the ventricular septal defect.
In TOF, both ventricles work at systemic
pressure but volume overload does not occur and congestive heart fail-ure is
rare.
These patients should arrive in the operating
room well sedated. Preoperative fluid restriction should be mini-mized and/or
maintenance fluid given intravenously to prevent hemoconcentration and
hypovolemia. A smooth induction is important to prevent increases in oxygen
demand or hypercyanotic spells. The agents used should have minimal peripheral
vasodilating effects. Thus, halothane is theoretically preferable to isoflurane
or sevoflurane for this purpose. Mild myocardial depression may relieve
infundibular obstruction and is, therefore, desirable. If intravenous agents
are used, they should be carefully titrated to prevent relative overdose.
Intravenous barbiturate requirements may be halved. Ketamine can be safely
used, particularly in very sick patients, since it main-tains SVR and does not
cause “tet” spells.
Arterial oxygen saturation generally increases
upon induction of anesthesia in cyanotic patients. The reasons for this are
probably related to the reduction in oxygen consumption during anesthesia and
the subsequent increase in venous saturation. Monitoring blood pressure may
become problematic in patients with previous shunting procedures using the
subclavian arteries. The contralateral arm should be used for invasive or
non-invasive monitoring. For major surgery, intra-arterial and/or central
venous pressures should be measured directly. This will also allow blood
sampling for blood gas and acid–base measurements. Because the major
myocar-dial stress rests on the right ventricle in these patients, central
venous pressures can be used to assess cardiac performance.
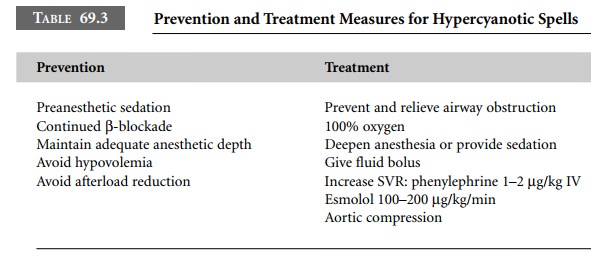
Hypercyanotic spells may develop
perioperatively because of the dynamic nature of the muscular infundibu-lar
obstruction present in TOF. Strategies to prevent and treat these complications
are outlined in Table 69.3.
These patients require endocarditis prophylaxis
for life.
Transposition of the Great Arteries (TGA) and Complex Lesions
These patients will have undergone repair or
palliation prior to any elective noncardiac surgery and will be dis-cussed
below.
Related Topics