Chapter: Medical Surgical Nursing: Terrorism, Mass Casualty, and Disaster Nursing
Weapons of Terror: Nuclear Radiation Exposure
Nuclear Radiation Exposure
The threat of nuclear warfare or radiation exposure
is very real with the availability of nuclear material and easily concealed
sim-ple devices, such as the so-called dirty bomb, for dispersal. A dirty bomb
is a conventional explosive (eg, dynamite) that is packaged with radioactive
material that scatters when the bomb is deto-nated. It disperses radioactive
material and may be called a radi-ologic weapon, but is not a nuclear weapon,
which is a complex nuclear fission reaction that is thousands of times more
devastat-ing than the dirty bomb.
Sources of radioactive
material include not only nuclear weapons but reactors and simple radioactive
samples, such as weapons-grade plutonium or uranium, freshly spent nuclear
fuel, or medical supplies (eg, radium, certain cesium isotopes) used in cancer
treatments and radiography machines. Exposure of a large number of people can
be accomplished by placing a radioactive sample in a public place. Thousands
may be exposed this way; some may be immediately affected, and others may
require health monitoring for many years to assess long-term effects.
History has demonstrated
the effectiveness of these weapons in the devastating results of the bombings
of Hiroshima and Nagasaki in World War II. The effects of radiation exposure
also were felt by the inhabitants of a small town in Brazil, who in 1987 found
and opened a small canister of cesium 137 and rubbed the blue powder on
themselves; 249 people were sickened, and 4 died
Jagminas & Suner,
2001). In 1983, a hospital sample was stolen in Mexico, resulting in the
release of radioactive material among some scrap metal. A year later, the radiation
contamination was de-tected when the scrap metal was inadvertently transported
into the Los Alamos National Laboratory and triggered a Geiger counter.
On a larger scale,
nuclear reactor incidents have occurred in the Chernobyl (1986) and Three Mile
Island (1979) nuclear fa-cilities. There were 31 official deaths on the day of
the Chernobyl incident, which involved a core meltdown and explosion,
releas-ing radiation throughout the community. The long-term effects of this
incident, including increased incidence of thyroid cancers and leukemia,
continue to be evaluated. Reactors, however, fol-low very strict security
measures and protocols for prevention of core meltdown. These measures decrease
the possibility of a ra-diation incident from a reactor.
TYPES OF RADIATION
Atoms consist of protons, neutrons, and electrons. The
protons and neutrons are in balance in the nucleus. The protons repel each
other, because they are all positively charged. The number of protons is
specific for each element in the periodic table. There is a specific ratio of
protons and neutrons for each different atom, and the result is element
stability. When an element is radio-active, there is an imbalance in the
nucleus resulting from an excess of neutrons.
To achieve stability, a radioactive nuclide can eject
particles until the most stable number (an even number) of protons and neutrons
exists. A proton can become a neutron by ejecting a positron; conversely, a
neutron can become a proton by ejecting a negative electron. An alpha particle
is released when two pro-tons and two electrons are ejected.
Alpha particles cannot penetrate the skin. A thin layer
of paper or clothing is all that is necessary to protect the skin from
alpha-radiation. However, this low-level radiation can enter the body through
inhalation, ingestion, or injection (open wound).
Only localized damage will occur.
Beta particles have the ability to moderately penetrate
the skin to the layer in which skin cells are being produced. This high-energy
radiation can cause skin damage if the skin is exposed for a prolonged period
and can cause injury if beta particles become internal by penetrating the skin.
Gamma-radiation is a short-wavelength electromagnetic
en-ergy that is emitted when there is excess core nucleus energy. Gamma
particles are penetrating. It is difficult to shield against gamma-radiation.
X-rays are an example of gamma-radiation. Gamma-radiation often accompanies
both alpha- and beta-particle emission.
MEASUREMENT AND DETECTION
Radiation is measured in
several different units. The rad is
the basic unit of measurement. A rad is equivalent to 0.01 joule of energy per
kilogram of tissue. To determine the damaging effect of the rad, a conversion
to the rem (Roentgen equivalent man)
is necessary. The rem reflects the type of radiation absorbed and the potential
for damage. For example, 200,000 mrem will result in mild radiation sickness (1
rem = 1000 millirem) ( Jagminas& Suner, 2001).
Typical natural yearly exposure for an individual is 360 mrem. Another
important concept is half-life. The
half-life of a radioactive product is the time it takes to lose one half of its
radioactivity.
Radiation is invisible.
The only means of detection is through a device that determines the exposure
per minute. There are var-ious devices for this purpose. The Geiger counter (or
Geiger-Mueller survey meter) can measure background radiation quickly through
detection of gamma- and some beta-radiation. With high-level radiation, the
Geiger counter may underestimate exposure. Other devices include the ionization
chamber survey meter, alpha monitors, and dose-rate meters. Personal dosimeters
are simple tools to identify radiation exposure and are worn by radiology
personnel.
EXPOSURE
Exposure is affected by
time, distance, and shielding. The longer a person is within the radiation
area, the higher the exposure. Also, the larger the amount of radioactive
material in the area, the greater the exposure. The farther away the person is
from the ra-diation source, the lower the exposure. Shielding from the
radia-tion source also decreases exposure. One should never touch radioactive
materials directly.
Three types of radiation-induced
injury can occur: external ir-radiation, contamination with radioactive
materials, and incor-poration of radioactive material into body cells, tissues,
or organs.
External irradiation exposure
occurs when all or part of thebody is exposed to radiation that penetrates or
passes completely through the body. In this type of exposure, the patient is
not radioactive and does not require special isolation or decontami-nation
measures. Irradiation does not necessarily constitute a medical emergency.
Contamination occurs when the body is exposed to radioactivegases,
liquids, or solids either externally or internally. If internal, the
contaminant can be deposited within the body. Contamination requires immediate
medical management to prevent incorporation.
Incorporation is the actual uptake of radioactive material intothe
cells, tissues, and susceptible organs. The organs involved are usually the
kidneys, bone, liver, and thyroid.
Sequelae of
contamination and incorporation can occur days to years later. The thyroid
gland can be largely protected from radiation exposure by administration of
stable iodine (potassium iodide, or KI) before or promptly after the intake of
radioactive iodine (WHO, 1999).
Priorities in the
treatment of any type of radiation exposure are always treatment of
life-threatening injuries and illnesses first, followed by measures to limit
exposure, contamination control, and finally decontamination.
DECONTAMINATION
Hospital and countywide
disaster plans should be in effect when managing a radiation disaster. Access
restriction is essential to prevent contamination of other areas of the
hospital. Triage out-side the hospital is the most effective means of
preventing conta-mination of the facility itself. Floors are covered to prevent
tracking of contaminants throughout the treatment areas. Strict isolation
precautions should be in effect. Waste is controlled through double-bagging and
the use of plastic-lined containers outside of the facility.
Staff are required to wear protective clothing, such as
water-resistant gowns, two pairs of gloves, masks, caps, goggles, and booties.
Dosimetry devices should be worn by all staff members participating in patient
care. The radiation safety officer in the hospital should be notified
immediately to assist with surveys (using a radiation survey meter) of the
incoming patients and to provide dosimeters to all staff personnel involved
with patient care of exposed victims. There is minimal risk to staff if the
pa-tients are properly surveyed and decontaminated. The majority of patients
can be safely decontaminated with soap and water.
Each patient arriving at
the hospital should be first surveyed with the radiation survey meter for
external contamination and then directed toward the decontamination area as
needed. De-contamination occurs outside of the ED with a shower, collec-tion
pool, tarp, and collection containers for patient belongings, as well as soap,
towels, and disposable paper gowns for patients. Water runoff needs to be
contained. Patients who are uninjured can perform self-decontamination with the
use of handheld showers. After the patient has showered, a resurvey should be
conducted to determine whether the radioactive contaminants have been removed.
Additional washings should occur until the patient is free of contamination. It
is important to ensure during showers that previously clean areas are not
contaminated with runoff from the washed contaminated areas (eg, hair should be
washed in the bent-over position to protect the body from contamination).
Biologic samples should be taken through nasal and throat
swabs, and a complete blood count with differential should be obtained. Wounds
should be irrigated and then covered with a water-resistant dressing prior to
total body decontamination.
Internal contamination or incorporation requires
decontami-nation through catharsis and/or gastric lavage with chelating agents
(agents that bind with radioactive substances and are then excreted). Samples
of urine, feces, and vomitus are surveyed to determine internal contamination
levels.
ACUTE RADIATION SYNDROME
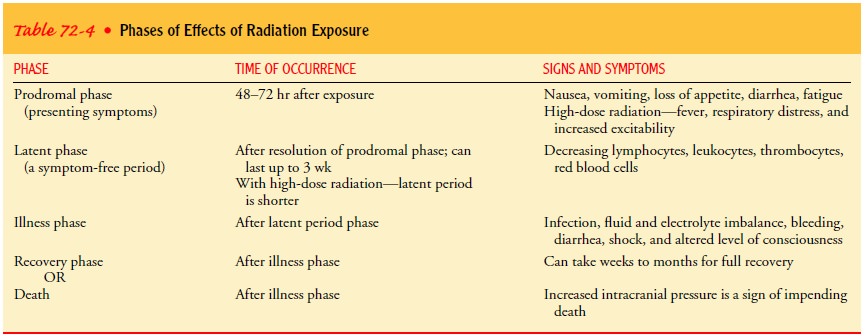
Acute radiation syndrome
(ARS) can occur after exposure to ra-diation. It is the dose rather than the
source that determines whether ARS develops. Factors that determine whether the
pa-tient’s response to exposure will result in ARS include a high dose (minimum
100 rad) and rate of radiation with total body expo-sure and penetrating-type
radiation. Age, medical history, and genetics also affect the outcome after
exposure. The effects follow a predictable course. Table 72-4 identifies the
phases of ARS.
Each body system is
affected differently in ARS. Systems with cells that rapidly reproduce are the
most affected. The effects on the hematopoietic system include decreased
numbers of lympho-cytes, granulocytes, thrombocytes, and reticulocytes. It is
the first system affected and serves as an indicator of the severity of
radi-ation exposure ( Jarrett, 2001; Jagminas & Suner, 2001). A marker of
outcome is the absolute lymphocyte count at 48 hours after ex-posure. A
significant exposure would be indicated by lymphocyte counts of 300 to 1200 per
cubic millimeter of blood (the normal lymphocyte count is 1500 to 3000/mm3).
Barrier precautions should be implemented to protect the patient from
infection. Neutrophils decrease within 1 week, platelets decrease within 2
weeks, and red blood cells decrease within 3 weeks. Hemor-rhagic complications,
fever, and sepsis are common.
The gastrointestinal
system, with its rapidly producing cells, is also readily affected by
radiation. Doses of radiation required to produce symptoms are approximately
600 rad or higherJagminas & Suner, 2001). The gastrointestinal symptoms
usu-ally occur at the same time as the changes in the hematopoietic system.
Nausea and vomiting occur within 2 hours after expo-sure. Sepsis, fluid and
electrolyte imbalance, and opportunistic infections can occur as complications.
An ominous sign is the presence of high fever and bloody diarrhea; these
typically appear on day 10 after exposure.
The central nervous
system is affected with doses greater than 1000 rad ( Jagminas& Suner,
2001). The symptoms occur when damage to the blood vessels of the brain results
in fluid leakage. Signs and symptoms include cerebral edema, nausea, vomiting,
headache, and increased intracranial pressure. Increased intra-cranial pressure
heralds a poor outcome and imminent death. Central nervous system injury with
this amount of exposure is ir-reversible and occurs before hematopoietic or
gastrointestinal sys-tem symptoms appear. Cardiovascular collapse is usually
seen in conjunction with these injuries.
Depending on the dose,
skin effects can also occur. With ex-posure of 600 to 1000 rad, erythema
occurs; it can disappear within hours, and then reappear. The exposed patient
must be evaluated hourly for the presence of erythema. With exposures greater
than 1000 rad, desquamation (radiation dermatitis) of the skin occurs. Necrosis
becomes evident within a few days to months at doses greater than 5000 rad.
Skin signs are an indication of the dose of radiation exposure.
Secondary injury can
occur when the radiation exposure oc-curs during a traumatic event such as a
blast or burn. Trauma in addition to radiation exposure increases patient
mortality. Atten-tion must first be directed toward the primary assessment for
trauma. Airway, breathing, circulation, and fracture reduction re-quire
immediate attention. All definitive treatments must occur within the first 48
hours. Thereafter, all surgical procedures should be delayed for 2 to 3 months
because of the potential for delayed wound healing and the possible development
of oppor-tunistic infections several weeks after exposure.
SURVIVAL
There are three categories of predicted survival after
radiation ex-posure: probable, possible, and improbable. Triage of victims at
the scene, after decontamination, is conducted with the routine system for
disaster triage. Presenting signs and symptoms deter-mine the potential for
survival and therefore the category of pre-dicted survival during triage.
Probable survival
victims have either no initial symptoms or only minimal symptoms (eg, nausea
and vomiting), or these symptoms resolve within a few hours. These patients
should re-ceive a complete blood count and may be discharged with in-structions
to return if any symptoms recur.
Possible survivors are
those who present with nausea and vom-iting that persists for 24 to 48 hours.
They will experience a latent period, during which leukopenia,
thrombocytopenia, and lym-phocytopenia occur. Barrier precautions and
protective isolation are implemented if the patient’s lymphocyte count is less
than 1200/mm3. Supportive treatment includes administration of
blood products, prevention of infection, and provision of enhanced nutrition.
The improbable survival
group is composed of those who have received more than 800 rad of total body
penetrating irradiation. Acutely, people in this group demonstrate vomiting,
diarrhea, and shock. Any neurologic symptoms suggest a lethal dose of
ra-diation (Jarrett, 2001). These patients still require decontamina-tion, to
prevent contamination of the area. Personal protection is essential, because it
is virtually impossible to fully decontaminate these patients since all of
their internal organs have been irradi-ated. The survival time is variable;
however, death usually ensues swiftly due to shock. If there are no neurologic
symptoms, the patient may be alert and oriented, similar to a patient with
extensive burns. In a mass casualty situation, the nurse should expect to
triage these patients into the black category, where they will receive comfort
measures and emotional support. If it is not a mass casualty situation,
aggressive fluid and electrolyte therapy are essential.
Although radiation,
biological, and chemical events are not everyday events, when they do occur
every facility and every nurse will need to know the basics of caring for affected
patients.
Any terrorist-sponsored
or unintentional radiation release can be sizeable and may require the entire
hospital and prehospital staff to be prepared, recognize signs and symptoms of
exposure, and rapidly treat victims without contamination of personnel,
visitors, patients, or the facility itself.
Related Topics