Chapter: Medical Surgical Nursing: Terrorism, Mass Casualty, and Disaster Nursing
Weapons of Terror: Biological Weapons
WEAPONS OF TERROR
Biological Weapons
Biological weapons are
weapons that spread disease among the general population or the military. Use
of biological weapons dates far back into history, but improved production
techniques and genetic engineering have expanded the potential for wide-spread
casualties as a result of biological weaponry.
EFFECTS OF BIOLOGICAL WEAPONS
Biological warfare is a covert method of severely affecting thetarget.
Overall, biological weapons are easily obtained and easily disseminated, and
they result in significant mortality and mor-bidity. The potential use of
biological agents calls for continuous increased surveillance by health
departments and an increased index of suspicion by clinicians. Many biological
weapons re-sult in signs and symptoms similar to those of common disease
processes.
Biological agents are
delivered in either a liquid or dry state, applied to foods or water, or
vaporized for inhalation or direct contact. Vaporization may be accomplished
through spray or ex-plosives loaded with the agent. With increased travel, an
agent could be released in one city and affect people in other cities
thou-sands of miles away. The vector can be an insect, animal, or per-son, or
there may be direct contact with the agent itself.
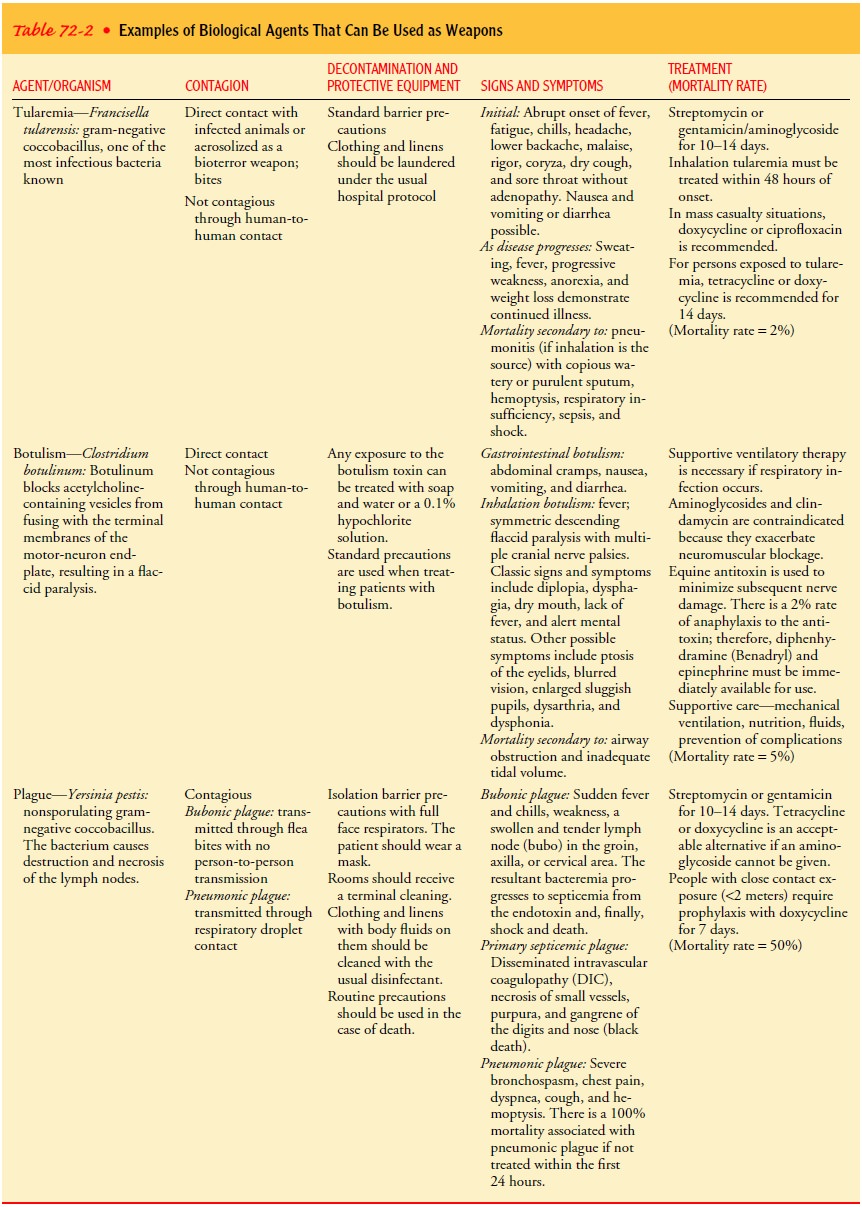
The following is a
discussion of two of the agents most likely to be used or weaponized. Table
72-2 describes other easily weap-onized biological agents.
ANTHRAX
Bacillus anthracis is a naturally occurring gram-positive, encapsu-lated rod
that lives in the soil in the spore state throughout the world. The bacterium
sporulates (is liberated) when exposed to air and is infective only in the
spore form. Contact with infected animal products (raw meat) or inhalation of
the spores results in infection. Cattle and other herbivores are vaccinated
against an-thrax to prevent transmission through contaminated meat.
It is believed that approximately 8000 to 50,000 spores
must be inhaled to put a person at risk. As an aerosol, anthrax is odor-less
and invisible and can travel a great distance before dissemi-nating; hence, the
site of release and the site of infection can be miles apart.
Anthrax is recognized as
the most likely weaponized biological agent available. Anthrax has been known
as a highly debilitating agent for centuries. It is believed that the plague in
1500 BC
Egypt was caused by anthrax (Spencer, Whitman & Morton, 2001). In 1979,
Sverdlosk, Russia, experienced the intentional release of anthrax, with
widespread mortality and morbidity. Anthrax was released with the sarin gas
attack in Tokyo, Japan, in 1995; how-ever, the method of release chosen was
poorly designed for effect.
Anthrax is caused by
replicating bacteria that release toxin re-sulting in hemorrhage, edema, and
necrosis. The incubation period is from 1 to 6 days. There are three primary
methods of infection: skin contact, inhalation, and gastrointestinal ingestion.
Skin lesions (the most common infection) cause edema with pruritis and macule
or papule formation resulting in ulceration with 1- to 3-mm vesicles. A
painless eschar develops, which falls off in 1 to 2 weeks.
Ingestion of anthrax results in fever, nausea and
vomiting, abdominal pain, bloody diarrhea, and occasionally ascites. If
mas-sive diarrhea develops, decreased intravascular volume becomes the primary
treatment concern. The bacterium affects the terminal ileum and cecum. Sepsis
can occur. Treatment is fluoroquinolones or tetracycline.
The inhalation form of
anthrax is the most severe. Its symp-toms mimic those of the flu, and usually
treatment is sought only when the second stage of severe respiratory distress
occurs. At this point, even antibiotic therapy will not halt the progress of
the dis-ease. The inhalation form can have an incubation period of up to 60
days, making it difficult to identify the source of the bacterium. Initial
signs and symptoms include cough, headache, fever, vom-iting, chills, weakness,
mild chest discomfort, dyspnea, and syn-cope, without rhinorrhea or nasal
congestion.
Most patients have a
brief recovery period followed by the sec-ond stage within 1 to 3 days,
characterized by fever, severe respira-tory distress, stridor, hypoxia,
cyanosis, diaphoresis, hypotension, and shock. These patients require
optimization of oxygenation, correction of electrolyte imbalances, and
ventilatory and hemody-namic support. More than 50% of these patients have
hemorrhagic mediastinitis on chest x-ray (a hallmark sign) (Spencer, Whitman,
Morton 2001; Altman,
2002; Inglesby et al., 1999). The disease can also progress to include
meningitis with subarachnoid hemor-rhage. Death results in approximately 24 to
36 hours after the onset of severe respiratory distress. The mortality rate
nears 100%.
Treatment.
Presently anthrax is penicillin sensitive;
however,the Russian government has been involved in the production of
penicillin-resistant anthrax. Recommended treatment includes penicillin,
erythromycin, chloramphenicol, gentamicin, or doxy-cycline. If antibiotic
treatment begins within 24 hours after ex-posure, death can be prevented (Franz
& Zajtchuk, 2000). In a mass casualty situation, ciprofloxacin or
doxycycline is recommended. Treatment is continued for 60 days. For patients
who have been directly exposed to anthrax but have no signs and symptoms of
disease, ciprofloxacin or doxycycline is used for prophylaxis fordays.
When caring for a
patient infected with anthrax, standard pre-cautions are all that are
necessary. The patient is not contagious, and the disease cannot be spread from
person to person. Equip-ment should be cleaned using standard hospital
disinfectant. After death, cremation is recommended because the spores can
survive for decades and represent a threat to morticians and foren-sic medicine
personnel.
SMALLPOX
Variola is classified as
a DNA virus. It has an incubation period of approximately 12 days. It is
extremely contagious and is spread by direct contact, contact with clothing or
linens, or by droplets from person to person only after the fever has decreased
and the rash phase has begun (Inglesby et al., 1999). There is an associ-ated
30% case-fatality rate. Aerosolization of the virus would re-sult in widespread
dissemination. The World Health Organization (WHO) declared smallpox eradicated
in 1977 and stopped world-wide vaccination in 1980. In the United States, the
last child was vaccinated in 1972. Therefore, a large portion of the current
pop-ulation has no immunity to the virus. Recently, plans have been instituted
in the U.S. for smallpox vaccination, with health care personnel being the
first to receive the vaccine.
Smallpox was used as
biowarfare during the French and Indian War in 1754–1767, when blankets from
smallpox patients were sent into the Indian camps, resulting in greater than
50% fatality rates (Inglesby et al., 1999). Smallpox virus survives for up to
24 hours in cool temperatures and low humidity.
Signs and symptoms include high fever, malaise, headache, backache, and prostration. After 1 to 2 days, a maculopapular rash appears, evolving at the same rate and beginning on the face, mouth and pharynx, and forearms (Fig 72-1). Only then does the rash pro-gress to the trunk and also become vesicular to pustular (Inglesby et al., 1999; Hagstad, 2000; Franz & Zajtchuk, 2000). There is a large amount of the virus in the saliva and pustules. Smallpox (variola) is contagious only after the appearance of the rash. Vari-ola major has a 30% case fatality rate. Hemorrhagic smallpox in-cludes all of the above signs and symptoms with the addition of a dusky erythema and petechiae to frank hemorrhage of the skin and mucous membranes, resulting in death by day 5 or 6. Variola minor produces fewer constitutional symptoms and a sparse rash.
Treatment.
Treatment includes supportive care with
antibioticsfor any additional infection. The patient must be isolated with the
use of transmission precautions. Laundry and biological wastes should be
autoclaved before being washed with hot water and bleach. Standard
decontamination of the room is effective. All persons who have household or
face-to-face contact with the patient after the fever begins should be
vaccinated within 4 days to prevent infection and death (Franz & Zajtchuk,
2000; Inglesby et al., 1999). A patient with a temperature of 38°C (101°F) or higher within 17
days after exposure requires isola-tion. Postvaccination encephalitis occurs in
approximately 1 of every 300,000 patients and has a 25% fatality rate.
Cremation is preferred for all deaths, because the virus can survive in scabs
for up to 13 years.
Related Topics