Chapter: Medical Surgical Nursing: Emergency Nursing
Violence, Abuse, and Neglect - Emergency Nursing
Violence,
Abuse, and Neglect
FAMILY VIOLENCE, ABUSE, AND NEGLECT
EDs are often the first
place where victims of family violence, abuse, or neglect go to seek help. Each
year in the United States 3 to 4 million women experience domestic violence,
and up to one third of all women will be in a domestic violence situation in
their lifetime. One million women are severely beaten each year. Approximately
2 to 3 million children are seriously abused, an additional 5 million children
are maltreated, and 1 to 2 million elders are abused or neglected (Guth,
Pachter, 2000). Among women who are pregnant, 4% to 14% will suffer physical
vio-lence from their intimate partner, with 10% to 24% of this pop-ulation
having been abused during the year before they became pregnant. These
statistics are startlingly higher for teenagers, of whom 20% are assaulted
while pregnant. The severity of the abuse increases and is associated with
battering during pregnancy. Domestic violence is the leading cause of death for
young African American women (Campbell, 1999; Harrell et al., 2002). On the
average, between 6% and 28% of women seen in the ED have suffered abuse, with
up to 6% of these patients seeking treatment for a complaint related to a
recent event. Between 20% and 35% of all ED visits relate to continuous abuse.
Young women are most likely to suffer nonlethal violent acts that result in
visits to the ED (Moskowitz, Griffith, DiScala, & Sege, 2001). ED nurses
must be aware that men and persons with disabilities are also victims of
domestic violence and should include questions to that effect in their
evaluations. Elder abuse takes many forms, including physical and psychological
abuse, neglect, violation of personal rights, and financial abuse.
Clinical Manifestations
When victims of abuse seek treatment, they may present
with physical injuries or with health problems, such as anxiety, in-somnia, or
gastrointestinal symptoms, that are related to stress. They usually do not
identify their abuser.
The possibility of abuse should be investigated whenever
a person presents with multiple injuries that are in various stages of healing,
when injuries are unexplained, and when the expla-nation does not fit the
physical picture (Chart 71-13). The pos-sibility of neglect should be
investigated whenever a dependent person with adequate resources and a
designated care provider shows evidence of inattention to hygiene, to
nutrition, or to known medical needs (eg, unfilled medication prescriptions,
missed appointments with health care providers). In the ED, the most common
physical injuries seen are unexplained bruises, lacerations, abrasions, head
injuries, or fractures. The most com-mon clinical manifestations of neglect are
malnutrition and de-hydration.
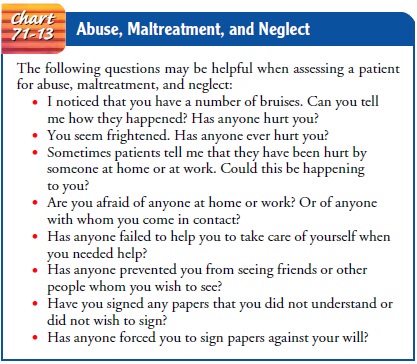
Assessment and Diagnostic Findings
Nurses in EDs are in an ideal position to provide early
detection and interventions for victims of domestic violence. This requires an
acute awareness of the signs of possible abuse, maltreatment, and neglect.
Nurses must be skilled in interviewing techniques that are likely to elicit
accurate information. A careful history is crucial in the screening process.
Asking questions in private— away from others—may be helpful in eliciting
information about abuse, maltreatment, and neglect.
Whenever evidence leads one to suspect abuse or neglect,
an evaluation with careful documentation of descriptions of events and drawings
or photos of injuries is important, because the med-ical record may be used as
part of a legal document. Assessment of the patient’s general appearance and
interactions with signifi-cant others, an examination of the entire surface
area of the body, and a mental status examination are crucial.
Management
Whenever abuse, maltreatment, or neglect is suspected,
the health care worker’s primary concern should be the safety and welfare of
the patient. Treatment focuses on the consequences of the abuse, violence, or
neglect and on prevention of further injury. Protocols of most EDs require that
a multidisciplinary ap-proach be used. Nurses, physicians, social workers, and
commu-nity agencies work collaboratively to develop and implement a plan for
meeting the patient’s needs.
If in immediate danger, the patient should be separated
from the abusing or neglecting person whenever possible. On the basis of this
danger, or on the basis of injuries or neglected medical conditions, hospitalization
is justified until alternative plans are made. However, it must be remembered
that third-party payers may not approve hospitalization that is based solely on
abuse or neglect.
When abuse or neglect is considered to be the result of
stress experienced by a caregiver who is no longer able to cope with the burden
of caring for an elderly person or a person with chronic disease or a
disability, respite services may be necessary. Support groups may be helpful to
these caregivers. When mental illness of the abuser or neglecter is responsible
for the situation, alternative living arrangements may be required.Nurses must
be mindful that competent adults are free to ac-cept or refuse the help that is
offered to them. Some patients will insist on remaining in the home environment
where the abuse or neglect is occurring. The wishes of patients who are
competent and not cognitively impaired should be respected. However, all
possible alternatives and available resources should be explored with the
patient.
Mandatory reporting laws in most states require health
care workers to report suspected
abuse to an official agency, usually Adult (or Child) Protective Services. All
that is required for re-porting is the suspicion of abuse. The health care
worker is not required to prove anything. Likewise, health care workers who
re-port suspected abuse are immune to civil or criminal liability if the report
is made in good faith. Subsequent home visits result-ing from the report of
suspected abuse are a part of gathering information about the patient in the
home environment. In addition, many states have resource hotlines for use by
health care workers and by patients who seek answers to questions about abuse
and neglect.
SEXUAL ASSAULT
The definition of rape is forced sexual acts, especially
vaginal or anal penetration. Perpetrators and victims may be either male or
female. The feminist movement has focused on the rights and care of rape
victims, and law enforcement agencies are becoming increasingly sensitive and
aggressive in managing these crimes. Rape crisis centers offer support, educate
victims, and help them through the subsequent courtroom experience.
The manner in which the patient is received and treated
in the ED is important to his or her future psychological well-being. Crisis
intervention should begin when the patient enters the health care facility. The
patient should be seen immediately. Most hospitals have a written protocol that
reflects consideration for the victim’s physical and emotional needs as well as
forensic evidence collection that is required.
The Sexual Assault Nurse Examiner
In many states, there is
the opportunity for emergency nurses to become trained sexual assault nurse
examiners (SANEs). The role allows for specific training in forensic evidence
collection, history taking, documentation, and ways to approach the patient and
family. Specialized training also includes proper photography and the use of
colposcopy. Colposcopy increases assessment by examination for microtrauma
through magnification. Evidence is collected through photography, videography,
and analysis of specimens. Another tool useful to SANEs is the light-staining
microscope, which enables the examiner to identify motile and nonmotile sperm
and infection. This tool saves time and also enhances assessment. SANEs
complement the ED staff and can spend more time with both the patient and
police officers inves-tigating the incident.
Assessment and Diagnostic Findings
The patient’s reaction to rape has been termed rape trauma syn-drome and is seen as an
acute stress reaction to a life-threateningsituation. The nurse performing the
assessment is aware that the patient may go through several phases of
psychological reactions (Dole, 1996; Ritchie, 1998):
·
An acute disorganization
phase, which may manifest as an expressed state in which shock, disbelief,
fear, guilt, humiliation, anger, and other such emotions are encountered or as
a controlled state in which feelings are masked or hidden and the victim
appears composed
·
A phase of denial and
unwillingness to talk about the inci-dent, followed by a phase of heightened
anxiety, fear, flash-backs, sleep disturbances, hyperalertness, and
psychosomatic reactions
·
A phase of reorganization, in
which the incident is put into perspective. Some victims never fully recover
and go on to develop chronic stress disorders and phobias.
Management
The goals of management are to give sympathetic support,
to re-duce the emotional trauma of the patient, and to gather available
evidence for possible legal proceedings. All of the interventions have the
ultimate goal of having the patient regain control over his or her life.
Throughout the patient’s
stay in the ED, the patient’s privacy and sensitivity must be respected. The
patient may exhibit a wide range of emotional reactions, such as hysteria,
stoicism, or feel-ings of being overwhelmed. Support and caring are crucial.
The patient should be reassured that anxiety is natural and asked whether a
support person may be called. Appropriate support is available from
professional and community resources. The Rape Victim Companion Program, if
available in the community, can be contacted, and services of a volunteer can
be requested. The patient should never be left alone.
PHYSICAL EXAMINATION
A written, witnessed
informed consent must be obtained from the patient (or parent or guardian if
the patient is a minor) for ex-amination, for taking of photographs, and for
release of findings to police. A history is obtained only if the patient has
not already talked to a police officer, social worker, or crisis intervention
worker. The patient should not be asked to repeat the history. Any history of
the event that is obtained should be recorded in the patient’s own words. The
patient is asked whether he or she has bathed, douched, brushed teeth, changed
clothes, urinated, or defecated since the attack, because these actions may
alter in-terpretation of subsequent findings. The time of admission, time of
examination, date and time of the alleged rape, and the patient’s emotional
state and general appearance (including any evidence of trauma, such as
discoloration, bruises, lacerations, secretions, or torn and bloody clothing)
are documented.
For the physical examination, the patient is helped to
undress and is draped properly. Each item of clothing is placed in a sepa-rate
paper bag. Plastic bags are not used because they retain mois-ture; moisture
may promote mold and mildew formation, which can destroy evidence. The bags are
labeled and given to appro-priate law enforcement authorities.
The patient is examined (from head to toe) for injuries,
espe-cially injuries to the head, neck, breast, thighs, back, and but-tocks.
Body diagrams and photographs aid in documenting the evidence of trauma. The
physical examination focuses on the following:
·
External evidence of trauma
(bruises, contusions, lacerations, stab wounds)
·
Dried semen stains (appearing
as crusted, flaking areas) on the patient’s body or clothes
·
Broken fingernails and body
tissue and foreign materials under nails (if found, samples are taken)
·
Oral examination, including a
specimen of saliva and pre-scribed cultures of gum and tooth areas
Pelvic and rectal
examinations are also performed. The per-ineum and other areas are examined
with a Wood lamp or other filtered ultraviolet light. Areas that appear
fluorescent may indi-cate semen stains. The color and consistency of any
discharge pres-ent is noted. A water-moistened rather than a lubricated vaginal
speculum is used for the examination. Lubricant contains chemi-cals that may
interfere with later forensic testing of specimens and acid phosphatase
determinations. The rectum is examined for signs of trauma, blood, and semen.
During the examination, the patient should be advised of the nature and
necessity of each pro-cedure and given the rationale for each question asked.
SPECIMEN COLLECTION
During the physical
examination, numerous laboratory speci-mens may be collected, including the
following:
·
Vaginal aspirate, examined for
presence or absence of motile and nonmotile sperm
·
Secretions (obtained with a
sterile swab) from the vaginal pool for acid phosphatase, blood group antigen
of semen, and precipitin test against human sperm and blood
·
Separate smears from the oral,
vaginal, and anal areas
·
Culture of body orifices for
gonorrhea
·
Blood serum for syphilis and
HIV testing; a sample of serum for syphilis may be frozen and saved for future
testing
·
Pregnancy test if there is a
possibility that the patient may be pregnant
·
Any foreign material (leaves,
grass, dirt), which is placed in a clean envelope
·
Pubic hair samples obtained by
combing or trimming. Sev-eral pubic hairs with follicles are placed in separate
contain-ers and identified as the patient’s hairs.
To preserve the chain of evidence, each specimen is
labeled with the name of the patient, the date and time of collection, the body
area from which the specimen was obtained, and the names of personnel
collecting specimens. Then the specimens are given to a designated person (eg,
crime laboratory technician), and an itemized receipt is obtained.
TREATING POTENTIAL CONSEQUENCES OF RAPE
After the initial physical examination is completed and
specimens have been obtained, any associated injuries are treated as
indi-cated. The patient is given the option of prophylaxis against sex-ually
transmitted disease. Ceftriaxone (Rocephin), administered intramuscularly with
1% lidocaine (Xylocaine), may be pre-scribed as prophylaxis for gonorrhea.
Doxycycline (Vibramycin) taken for 10 days may be prescribed as prophylaxis for
syphilis and chlamydia.
Antipregnancy measures
may be considered if the patient is of childbearing age, is not using
contraceptives, and is at high risk in her menstrual cycle. A postcoital
contraceptive medication, such as Ovral, which contains estrogen ethinyl
estradiol and pro-gestin norgestrel, may be prescribed after a pregnancy test.
To promote effectiveness, Ovral should be administered within 12 to 24 hours
and no later than 72 hours after intercourse. The 21-day package rather than
the 28-day package is prescribed, so that the patient does not take the inert
tablets by mistake. An antiemetic may be administered as prescribed to decrease
discomfort from side effects. A cleansing douche, mouthwash, and fresh clothing
are usually offered.
FOLLOW-UP CARE
The patient is informed of counseling services to prevent
long-term psychological effects. Counseling services should be made available
to both the patient and the family. A referral is made to the Rape Victim
Companion Program, if available. Appointments for follow-up surveillance for
pregnancy, sexually transmitted disease, and HIV testing also are made.
The patient is encouraged to return to his or her
previous level of functioning as soon as possible. When leaving the health care
facility, the patient should be accompanied by a family member or friend.
VIOLENCE IN THE EMERGENCY DEPARTMENT
Not only do ED staff
members encounter patients who are vio-lent from substance abuse, injury, or
other emergencies, but they may also encounter violent situations in the rest
of the environ-ment. Patients and families waiting for assistance are
increasingly volatile. Often, waiting rooms are the site for dissatisfaction,
fear, and anger to be acted out in violence. Some EDs assign security officers
to the area and have installed metal detectors to identify weapons and protect
patients, families, and staff. It is not unusual for a patient to come to the
ED armed. Nurses and other per-sonnel must be prepared to deal with such
circumstances.
Management
Safety is the first priority. Protecting the ED on a
daily basis will prevent any untoward events from occurring. Protection of the
department provides protection for the patients, families, and staff. It is
essential that all nurses be aware of the environment in which they are
working.
Metal detectors, silent alarm systems, and secured entry
into the department assist in maintaining safety. Members of gangs and feuding
families need to be separated in the ED, in the wait-ing room, and later in the
inpatient nursing unit to avoid angry confrontations. Security officers should
be ready to assist at all times. The department should be able to be locked
against entry if security is at all in question.
Patients from prison and those who are under guard need
to be shackled to the bed with appropriate assessment. The same as-sessment and
care that are provided to patients with hand or ankle restraints are provided
to patients with handcuffs. In addi-tion, the following precautions are taken:
·
Never release the hand or
ankle restraint (handcuff).
·
Always have a guard present in
the room.
·
Place the patient face down on
the stretcher to avoid injury from head-butting, spitting, or biting.
·
Use restraints on any violent
patient as needed.
·
Administer medication if
necessary to control violent be-havior until definitive treatment can be
obtained.
In the case of gunfire
in the ED, self-protection is a priority. There is no advantage to protecting
others if the caregivers are also injured. Security officers and police must
gain control of the situation first; then care is provided to the injured.
Related Topics