Chapter: Medical Physiology: Insulin, Glucagon, and Diabetes Mellitus
Type I Diabetes-Lack of Insulin Production by Beta Cells of the Pancreas
Type I Diabetes-Lack of Insulin Production by Beta Cells of the Pancreas
Injury to the beta cells of the pancreas or diseases that impair insulin production can lead to type I diabetes.
Viral infections or autoimmune disorders may beinvolved in the destruction of beta cells in many patients with type I diabetes, although heredity also plays a major role in determining the susceptibility of the beta cells to destruction by these insults. In some instances, there may be a hereditary tendency for beta cell degen-eration even without viral infections or autoimmune disorders.
The usual onset of type I diabetes occurs at about 14 years of age in the United States, and for this reason it is often called juvenile diabetes mellitus. Type I diabetes may develop very abruptly, over a period of a few days or weeks, with three principal sequelae: (1) increased blood glucose, (2) increased utilization of fats for energy and for formation of cholesterol by the liver, and (3) depletion of the body’s proteins.
Blood Glucose Concentration Rises to Very High Levels in Diabetes Mellitus. The lack of insulin decreases the efficiencyof peripheral glucose utilization and augments glucose production, raising plasma glucose to 300 to 1200 mg/100 ml. The increased plasma glucose then has multiple effects throughout the body.
Increased Blood Glucose Causes Loss of Glucose in the Urine
The high blood glucose causes more glucose to filter into the renal tubules than can be reabsorbed, and the excess glucose spills into the urine. This normally occurs when the blood glucose concentration rises above 180 mg/100 ml, a level that is called the blood “thresh-old” for the appearance of glucose in the urine. When the blood glucose level rises to 300 to 500 mg/100 ml— common values in people with severe untreated dia-betes—100 or more grams of glucose can be lost into the urine each day.
Increased Blood Glucose Causes Dehydration The very highlevels of blood glucose (sometimes as high as 8 to 10 times normal in severe untreated diabetes) can cause severe cell dehydration throughout the body. This occurs partly because glucose does not diffuse easily through the pores of the cell membrane, and the increased osmotic pressure in the extracellular fluids causes osmotic transfer of water out of the cells.
In addition to the direct cellular dehydrating effect of excessive glucose, the loss of glucose in the urine causes osmotic diuresis. That is, the osmotic effect of glucose inthe renal tubules greatly decreases tubular reabsorption of fluid. The overall effect is massive loss of fluid in the urine, causing dehydration of the extracellular fluid, which in turn causes compensatory dehydration of the intracellular fluid. Thus, polyuria (excessive urine excretion), intracellularand extracellular dehydration, and increased thirst areclassic symptoms of diabetes.
Chronic High Glucose Concentration Causes Tissue Injury Whenblood glucose is poorly controlled over long periods in diabetes mellitus, blood vessels in multiple tissues throughout the body begin to function abnormally and undergo structural changes that result in inadequate blood supply to the tissues. This in turn leads to increased risk for heart attack, stroke, end-stage kidney disease, retinopathy and blindness, and ischemia and gangrene of the limbs.
Chronic high glucose concentration also causes damage to many other tissues. For example, peripheralneuropathy, which is abnormal function of peripheralnerves, and autonomic nervous system dysfunction are frequent complications of chronic, uncontrolled dia-betes mellitus. These abnormalities can result in impaired cardiovascular reflexes, impaired bladder control, decreased sensation in the extremities, and other symptoms of peripheral nerve damage.
The precise mechanisms that cause tissue injury in diabetes are not well understood but probably involve multiple effects of high glucose concentrations and other metabolic abnormalities on proteins of endothe-lial and vascular smooth muscle cells, as well as other tissues. In addition,hypertension, secondary to renal injury, and atherosclerosis, secondary to abnormal lipid metabolism, often develop in patients with diabetes and amplify the tissue damage caused by the elevatedglucose.
Diabetes Mellitus Causes Increased Utilization of Fats and Meta bolic Acidosis. The shift from carbohydrate to fat metab-olism in diabetes increases the release of keto acids, such as acetoacetic acid and b-hydroxybutyric acid, into the plasma more rapidly than they can be taken up and oxidized by the tissue cells. As a result, the patient develops severe metabolic acidosis from the excess keto acids, which, in association with dehydration due to the excessive urine formation, can cause severe acidosis. This leads rapidly to diabetic coma and death unless the condition is treated immediately with large amounts of insulin.
All the usual physiologic compensations that occur in metabolic acidosis take place in diabetic acidosis. They include rapid and deep breathing, which causes increased expiration of carbon dioxide; this buffers the acidosis but also depletes extracellular fluid bicarbonate stores. The kidneys compensate by decreas-ing bicarbonate excretion and generating new bicar-bonate that is added back to the extracellular fluid.
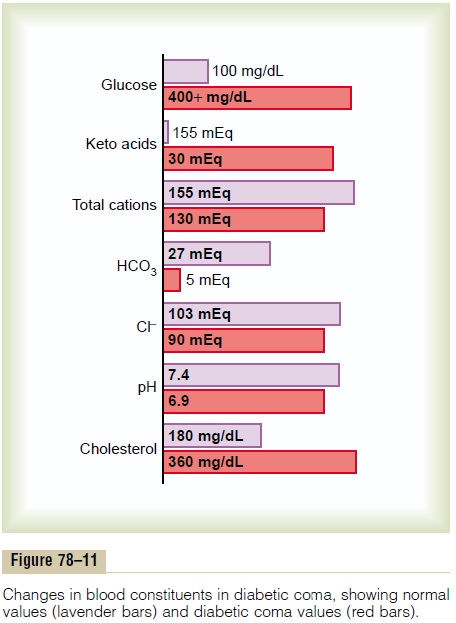
Although extreme acidosis occurs only in the most severe instances of uncontrolled diabetes, when the pH of the blood falls below about 7.0, acidotic coma and death can occur within hours. The overall changes in the electrolytes of the blood as a result of severe diabetic acidosis are shown in Figure 78–11.
Excess fat utilization in the liver occurring over a long time causes large amounts of cholesterol in the circu-lating blood and increased deposition of cholesterol in
Diabetes Causes Depletion of the Body’s Proteins. Failure touse glucose for energy leads to increased utilization and decreased storage of proteins as well as fat. Therefore, a person with severe untreated diabetes mellitus suffers rapid weight loss and asthenia (lack of energy) despite eating large amounts of food (polyphagia). Without treatment, these metabolic abnormalities can cause severe wasting of the body tissues and death within a few weeks.
Related Topics