Chapter: Obstetrics and Gynecology: Infertility
Treatment of Infertility
TREATMENT
A couple’s infertility may be
related to one or several abnormalities in one or both partners. Numerous medical,surgical, and assisted reproductive technology (ART)
ther-apies are available for treating the infertile couple. For coupleswith
unexplained infertility, empiric treatment may over-come the negative effects
of one or more mild abnormal-ities. These couples, as well as the majority of
infertile couples, tend to proceed through fertility treatment in a stepwise
fashion, starting with conservative and then with more aggressive ovarian
stimulation, inseminations, and eventually proceeding to IVF (explained below).
Surgical procedures are indicated
in certain circum-stances. If a woman presents with pelvic pain and
infertility, laparoscopy may be used to identify and treat the cause of her
pelvic pain as well as evaluate pelvic anatomy from a fer-tility standpoint. If
an obstructed fallopian tube is identified with HSG, it may be possible to
correct the obstruction sur-gically. For these operations to be successful, the
endo-salpinx must be healthy. If the tubal damage is significant enough to
impair gamete transport, then an ART such as IVF may be necessary. When
indicated, abnormalities of the uterine cavity such as submucosal leiomyomas,
endometrial polyps, intrauterine adhesions, and a septum can be surgically
corrected with a hysteroscopic procedure.
Ovarian Stimulation
Ovulation
induction is indicated in women with anovula-tion or
oligo-ovulation. However, any identified
condition asso-ciated with ovulatory disorders should be treated before initiating
ovulation-induction therapy. Such conditions include thyroid dis-orders,
hyperprolactinemia, PCOS, and high levels of stress (including psychologic
stress, intense exercise, or eating disorders).
The most
commonly used medication for ovulation induction is clomiphene citrate.Clomiphene is a selective
estrogenreceptor modulator (SERM) that competitively inhibits estrogen binding
to the estrogen receptors at the hypothal-amus and pituitary. The anti-estrogen
effects of clomiphene induce gonadotropin release from the pituitary, which
stim-ulates follicle development in the ovaries. Clomiphene is administered
daily for 5 days in the follicular phase of the menstrual cycle, starting
between cycle days 3 to 5. If ovula-tion does not occur, the dose is increased
for the subse-quent month. Women with ovulatory disorders associated with
oligomenorrhea may not have regular menses and may require a
progesterone-induced menses to start their clomiphene cycle. When used in women
who are already ovulatory, clomiphene may stimulate development of sev-eral
mature follicles.
With clomiphene, ovulation can
occur between 5 to 12 days after the last pill, and it can be monitored in
several ways. Urine LH kits can be used each day starting on cycle day 10; when
ovulation occurs, exposure to sperm through intercourse or intrauterine insemination (IUI) should occur. Transvaginal
ultrasound performed on cycle day 11 or 12 may identify a developing follicle.
When ultrasound is used and a mature follicle is identified (average diameter
>18 mm), ovulation can be triggered by administering a sub-cutaneous
injection of hCG. The exogenous hCG effec-tively simulates the LH surge and
ovulation occurs; this practice enables the proper timing of intercourse or
insem-ination. Some couples prefer to not monitor ovulation, and have regular
midcycle intercourse. In this situation, a serum progesterone level on cycle
day 21 can identify if ovulation has occurred. The use of clomiphene is associated with a 10% riskof multiple
gestations, the majority of which are twin gestations, and a small risk of
ovarian hyperstimulation and cyst formation.
Alternatively, exogenous gonadotropins can be given to stimulate follicular development. The use of gonado-tropins is commonly referred to as controlled ovarianhyperstimulation (COH). This therapy aims to achievemonofollicular ovulation in anovulatory women (particu-larly those who do not respond to clomiphene), and ovula-tion of several mature follicles in other infertile women. Available preparations include purified human menopausal gonadotropins (FSH and LH are extracted from the urine of postmenopausal women), and recombinant human FSH. The dose of medication is tailored to a woman’s age, body weight, infertility diagnosis, and response to previous fer-tility treatments. These medications are more potent than clomiphene and require frequent monitoring of follicle growth that usually includes transvaginal ultrasonography and serum estradiol measurements. When at least one mature follicle is identified (average follicle diameter of 18 mm and serum estradiol concentration >200 pg/mL), hCG is administered to trigger ovulation. Timed insemina-tions are commonly performed within 12 to 36 hours from hCG administration. The risks of this therapy include ovarian hyperstimulation syndrome (OHSS), which can require intensive therapy; a 25% incidence of multiple gestations; and an increased risk of ectopic pregnancy.
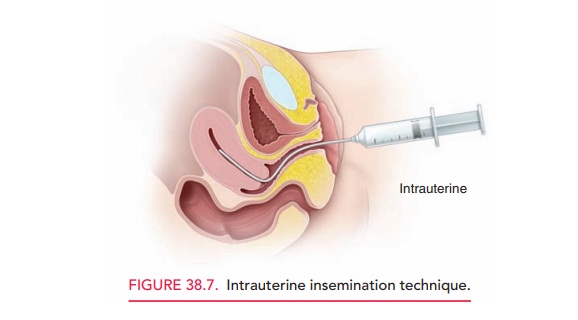
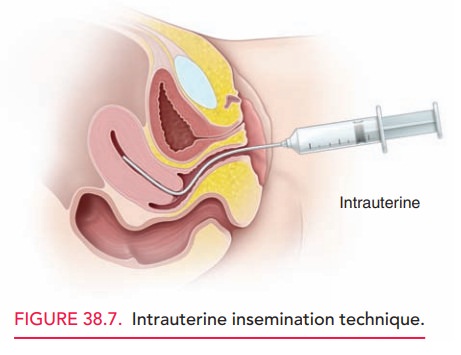
Intrauterine Insemination
Before performing IUI, an
ejaculated semen specimen is washed to remove prostaglandins, bacteria, and
proteins. The sperm is then suspended in a small amount of medium To perform
IUI, a speculum is inserted into the vagina, the specimen is placed in a thin
flexible catheter, and the catheter is advanced through the cervix into the
uterine cavity where the specimen is deposited (Fig. 38.7). A total motile
sperm count (concentration multiplied by motility) of at least one million must
be present, as pregnancy is rarely achieved with lower counts. In couples with infertility,and particularly
in those with mild male infertility, pregnancy rates are increased with IUI. However,
more severe maleinfertility may necessitate the use of ART to achieve
preg-nancy. If the male partner is azoospermic and no sperm are identified
during testicular biopsy, or if a woman does not have a male partner, IUI with
anonymous donor sperm is an available alternative.
Assisted Reproductive Technologies
All fertility procedures that
involve manipulation of gametes, zygotes, or embryos to achieve conception
com-prise the assisted reproductive technologies (ART). In the United States,
IVF accounts for more than 99% of all ART procedures. The process of IVF involves ovarian stimulation toproduce multiple
follicles, retrieval of the oocytes from the ovaries, oocyte fertilization in
vitro in the laboratory, embryo incuba-tion in the laboratory, and transfer of
embryos into a woman’s uterus through the cervix. The required medications
for IVFinclude gonadotropins to stimulate follicle development, a gonadotropin-releasing
hormone analogue (agonist or antagonist) to prevent premature ovulation during
folli-cle development, and hCG to initiate the final matura-tion of oocytes
prior to their retrieval. As with COH, the IVF process necessitates careful
monitoring of ovarian response with transvaginal ultrasonography and serum
estradiol measurements.
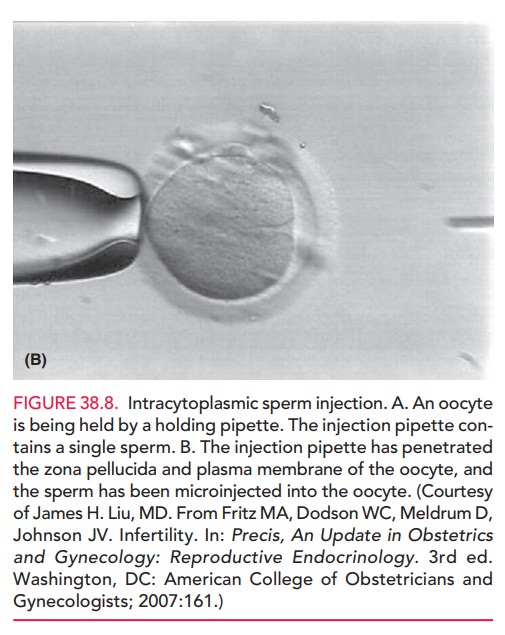
Depending on the etiology of infertility, fertilization can be achieved “naturally” by placing tens of thousands of sperm together with a single oocyte, or with intracyto-plasmic sperm injection (ICSI) by which a single spermis injected directly into the oocyte (Fig. 38.8).

Therefore, IVF provides the tools necessary
to bypass the normal mechanisms of gamete transport, fertilization, and embryo
transport. After oocyte retrieval, daily
progesterone supplemen-tation is necessary to insure the appropriate secretory
changes in the endometrium and to support the potential pregnancy; if
con-ception occurs, supplementation is continued until at least 10 weeks of
gestation.
Indications for IVF include the
following: absent or blocked fallopian tubes, tubal sterilization, failed
surgery to achieve tubal patency, severe pelvic adhesions, severe
endometriosis, poor ovarian response to stimulation, oligo-ovulation, severe
male factor infertility, unexplained infertility, or failed treatment with less
aggressive therapies. Success rates with
IVF depend on the etiology of infertility and the age of the female partner. The
chance of conception withone IVF cycle depends on the number and quality of
embryos transferred, and can be as high as 40% to 50%, with a 30% rate of
multiple gestations and at least a 15% rate of spontaneous abortion.
Related Topics