Chapter: Psychiatric Mental Health Nursing : Schizophrenia
Treatment - Schizophrenia
TREATMENT
Psychopharmacology
The primary medical treatment for schizophrenia is
psychopharmacology. In the past, electroconvulsive therapy, insulin shock
therapy, and psychosurgery were used, but since the creation of chlorpromazine
(Thorazine) in 1952, other treatment modalities have become all but obsolete.
Antipsychotic medications, also known as neuroleptics,
are prescribed primarily for their efficacy in decreasing psy-chotic symptoms.
They do not cure schizophrenia; rather, they are used to manage the symptoms of
the disease.
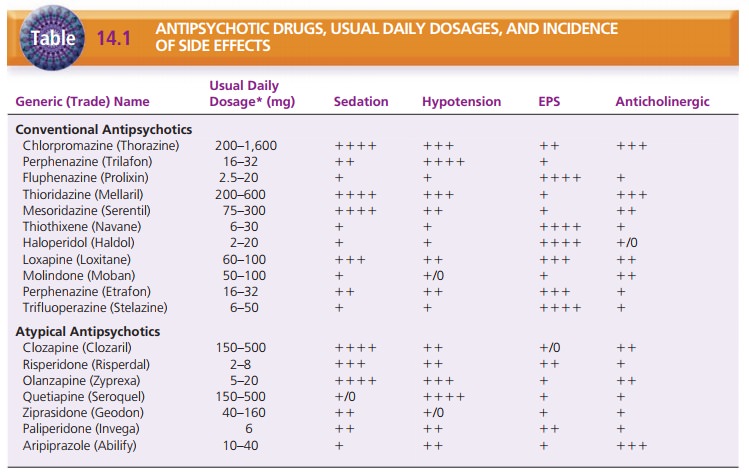
The older, or conventional, antipsychotic medications are dopamine
antagonists. The newer, or atypical, antipsy-chotic medications are both
dopamine and serotonin antag-onists . These medications, usual daily dos-ages,
and their common side effects are listed in Table 14.1. The conventional
antipsychotics target the positive signs of schizophrenia, such as delusions,
hallucinations, disturbed thinking, and other psychotic symptoms, but have no
observable effect on the negative signs. The atypical antip-sychotics not only
diminish positive symptoms but also, for many clients, lessen the negative
signs of lack of voli-tion and motivation, social withdrawal, and anhedonia.
Maintenance Therapy
Two antipsychotics are available in depot injection forms for
maintenance therapy: fluphenazine (Prolixin) in decanoate and enanthate
preparations and haloperidol (Haldol) in decanoate. The vehicle for depot
injections is sesame oil; therefore, the medications are absorbed slowly over
time into the client’s system. The effects of the medi-cations last 2 to 4 weeks,
eliminating the need for daily oral antipsychotic medication . The dura-tion of
action is 7 to 28 days for fluphenazine and 4 weeks for haloperidol. It may
take several weeks of oral therapy with these medications to reach a stable
dosing level before the transition to depot injections can be made. Therefore,
these preparations are not suitable for the management of acute episodes of
psychosis. They are, however, very use-ful for clients requiring supervised
medication compliance over an extended period.
Side Effects
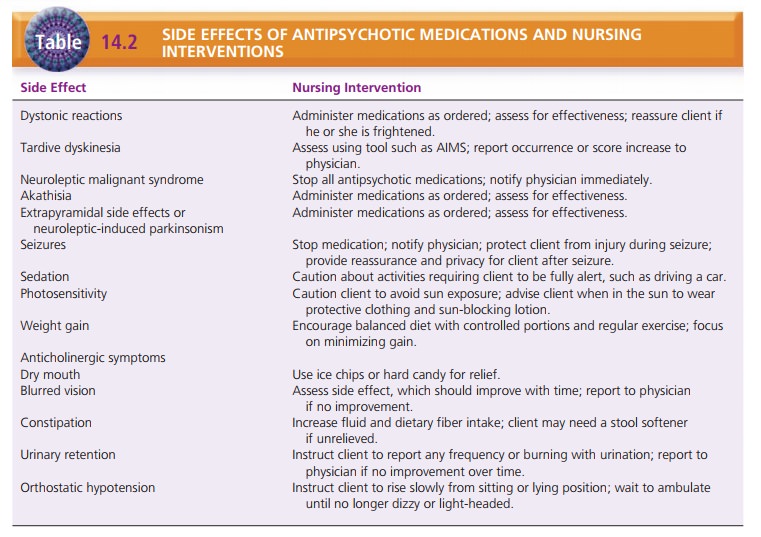
The side effects of antipsychotic medications are significant and
can range from mild discomfort to permanent move-ment disorders (Kane &
Marder, 2005). Because many of these side effects are frightening and upsetting
to clients, they are frequently cited as the primary reason that clients
discontinue or reduce the dosage of their medications. Seri-ous neurologic side
effects include extrapyramidal side effects (EPS) (acute dystonic
reactions, akathisia, and par-kinsonism), tardive dyskinesia, seizures, and
neuroleptic malignant syndrome (NMS; discussion to follow). Nonneu-rologic side
effects include weight gain, sedation, photosen-sitivity, and anticholinergic
symptoms such as dry mouth, blurred vision, constipation, urinary retention, and
orthos-tatic hypotension. Table 14.2 lists the side effects of antipsy-chotic
medications and appropriate nursing intervention.
Extrapyramidal Side Effects. EPS are reversible movement disorders induced by
neuroleptic medication. They in-clude dystonic reactions, parkinsonism, and
akathisia.
Dystonic reactions to antipsychotic medications
appearearly in the course of treatment and are characterized by spasms in
discrete muscle groups such as the neck muscles (torticollis) or eye muscles
(oculogyric crisis). These spasms also may be accompanied by protrusion of the
tongue, dys-phagia, and laryngeal and pharyngeal spasms that can com-promise
the client’s airway, causing a medical emergency. Dystonic reactions are
extremely frightening and painful for the client. Acute treatment consists of
diphenhydramine (Benadryl) given either intramuscularly or intravenously, or
benztropine (Cogentin) given intramuscularly.
Pseudoparkinsonism, or neuroleptic-induced
parkin-sonism, includes a shuffling gait, mask-like facies, muscle stiffness
(continuous) or cogwheeling rigidity (ratchet-like movements of joints),
drooling, and akinesia (slowness and difficulty initiating movement). These
symptoms usually appear in the first few days after starting or increasing the
dosage of an antipsychotic medication. Treatment of pseu-doparkinsonism and
prevention of further dystonic reac-tions are achieved with the medications
listed in Table 14.3.
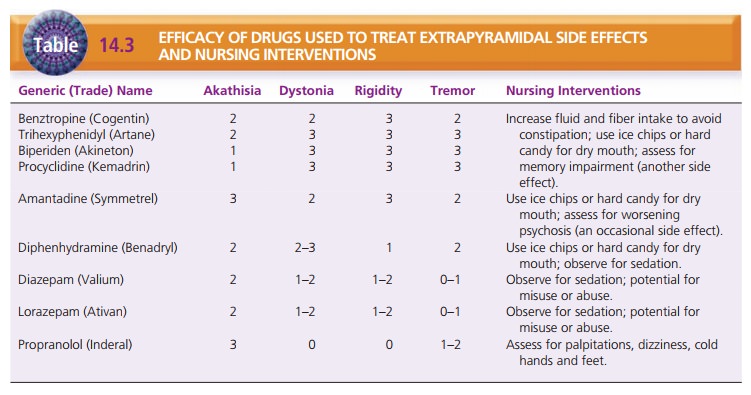
Akathisia is characterized by restless
movement, pac-ing, inability to remain still, and the client’s report of inner
restlessness. Akathisia usually develops when the antipsy-chotic is started or
when the dose is increased. Clients are very uncomfortable with these sensations
and may stop taking the antipsychotic medication to avoid these sideeffects.
Beta-blockers such as propranolol have been most effective in treating
akathisia, whereas benzodiazepines have provided some success as well.
The early detection and successful treatment of EPS is very
important in promoting the client’s compliance with medication. The nurse is
most often the person who observes these symptoms or the person to whom the
client reports symptoms. To provide consistency in assessment among nurses working
with the client, a standardized rating scale for extrapyramidal symptoms is
useful. The Simpson–Angus scale for EPS is one tool that can be used.
Tardive Dyskinesia. Tardive dyskinesia, a late-appearing side effect of antipsychotic
medications, is characterized by abnormal, involuntary movements such as lip
smack-ing, tongue protrusion, chewing, blinking, grimacing, and choreiform
movements of the limbs and feet. These invol-untary movements are embarrassing
for clients and may cause them to become more socially isolated. Tardive
dyskinesia is irreversible once it appears, but decreasing or discontinuing the
medication can arrest the progression. Clozapine (Clozaril), an atypical
antipsychotic drug, has not been found to cause this side effect, so it often
is rec-ommended for clients who have experienced tardive dys-kinesia while
taking conventional antipsychotic drugs.
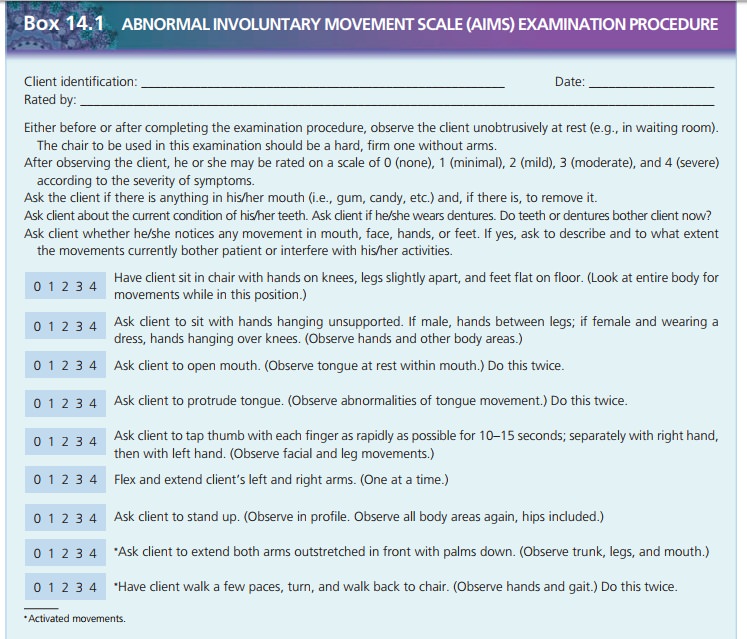
Screening clients for late-appearing movement disor-ders such as
tardive dyskinesia is important. The Abnor-mal
Involuntary Movement Scale (AIMS) is used to screen for symptoms of movement disorders. The client is observed in
several positions, and the severity of symp-toms is rated from 0 to 4. The AIMS
can be administered every 3 to 6 months. If the nurse detects an increased
score on the AIMS, indicating increased symptoms of tardive dyskinesia, he or
she should notify the physician so that the client’s dosage or drug can be
changed to prevent advancement of tardive dyskinesia.
Seizures. Seizures are an infrequent side effect
associ-ated with antipsychotic medications. The incidence is 1% of people
taking antipsychotics. The notable exception is clozapine, which has an
incidence of 5%. Seizures may be associated with high doses of the medication.
Treatment is a lowered dosage or a different antipsychotic medication.
Neuroleptic Malignant Syndrome. Neuroleptic malignant syndrome (NMS) is a serious and frequently fatal condi-tion seen in those being
treated with antipsychotic medi-cations. It is characterized by muscle
rigidity, high fever, increased muscle enzymes (particularly creatine
phospho-kinase), and leukocytosis (increased leukocytes). It is esti-mated that
0.1% to 1% of all clients taking antipsychotics develop NMS. Any of the
antipsychotic medications can cause NMS, which is treated by stopping the
medication. The client’s ability to tolerate other antipsychotic medica-tions
after NMS varies, but use of another antipsychotic appears possible in most
instances.
Agranulocytosis. Clozapine has the potentially
fatal side effect of agranulocytosis (failure of the bone
marrow to produce adequate white blood cells). Agranulocytosis develops
suddenly and is characterized by fever, malaise, ulcerative sore throat, and
leukopenia. This side effect may not be manifested immediately but can occur as
long as 18 to 24 weeks after the initiation of therapy. The drug must be
discontinued immediately. Clients taking this an-tipsychotic must have weekly
white blood cell counts for the first 6 months of clozapine therapy and every 2
weeks thereafter. Clozapine is dispensed every 7 or 14 days only, and evidence
of a white cell count above 3,500 cells/mm3 is required before a
refill is furnished.
Psychosocial Treatment
In addition to pharmacologic treatment, many other modes of
treatment can help the person with schizophrenia. Indi-vidual and group
therapies, family therapy, family educa-tion, and social skills training can be
instituted for clients in both inpatient and community settings.
Individual and group therapy sessions are often sup-portive in
nature, giving the client an opportunity for social contact and meaningful
relationships with other people. Groups that focus on topics of concern such as
medication management, use of community supports, and family concerns also have
been beneficial to clients with schizophrenia (Pfammatter, Junghan, &
Brenner, 2006).
Clients with schizophrenia can improve their social com-petence
with social skill training, which translates into more effective functioning in
the community. Basic social skill training involves breaking complex social
behavior into simpler steps, practicing through role-playing, and applying the
concepts in the community or real-world setting. Cognitive adaptation training
using environmental supports is designed to improve adaptive functioning in the
home setting. Individually tailored environmental supports such as signs,
calendars, hygiene supplies, and pill containers cue the client to perform
associated tasks (Velligan et al., 2006).
Moriana, Alarcon, and Herruzo (2006) found that psycho-social skill
training was more effective when carried out during in-home visits in the
client’s own environment rather than in an outpatient setting.
A new therapy, cognitive enhancement therapy (CET), combines
computer-based cognitive training with group sessions that allow clients to
practice and develop social skills. This approach is designed to remediate or
improve the clients’ social and neurocognitive deficits, such as attention,
memory, and information processing. The expe-riential exercises help the client
to take the perspective of another person, rather than focus entirely on self.
Positive results of CET include increased mental stamina, active rather than
passive information processing, and spontane-ous and appropriate negotiation of
unrehearsed social challenges (Hogarty, Greenwald, & Eack, 2006).
Family education and therapy are known to diminish the negative
effects of schizophrenia and reduce the relapse rate (Penn, Waldheter, Perkins,
Mueser, & Lieberman, 2005). Although inclusion of the family is a factor
that improves outcomes for the client, family involvement often is neglected by
health-care professionals. Families often have a difficult time coping with the
complexities and ramifications of the client’s illness. This creates stress
among family members that is not beneficial for the client or family members.
Family education helps to make fam-ily members part of the treatment team.
In addition, family members can benefit from a support-ive
environment that helps them cope with the many diffi-culties presented when a
loved one has schizophrenia. These concerns include continuing as a caregiver
for the child who is now an adult; worrying about who will care for the client
when the parents are gone; dealing with the social stigma of mental illness;
and possibly facing financial problems, marital discord, and social isolation.
Such sup-port is available through the National Alliance for the Men-tally Ill
and local support groups. The client’s health-care provider can make referrals
to meet specific family needs.
Related Topics