Chapter: Medical Surgical Nursing: Assessment and Management of Problems Related to Male Reproductive Processes
The Patient Undergoing Prostate Surgery
THE
PATIENT UNDERGOING PROSTATE SURGERY
Prostate
surgery may be indicated for the patient with BPH or prostate cancer. The
objectives before prostate surgery are to as-sess the patient’s general health
status and to establish optimal renal function. Prostate surgery should be
performed before acute urinary retention develops and damages the upper urinary
tract and collecting system or, in the case of prostate cancer, before cancer
progresses.
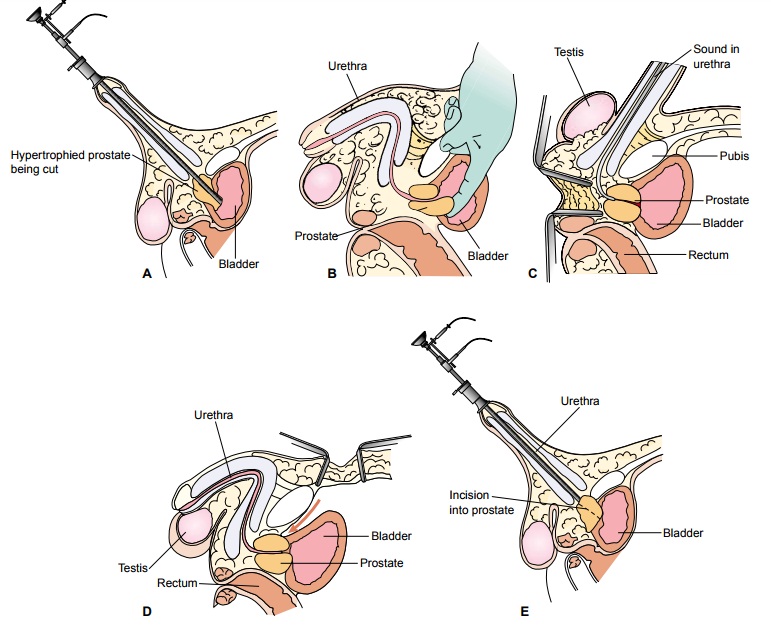
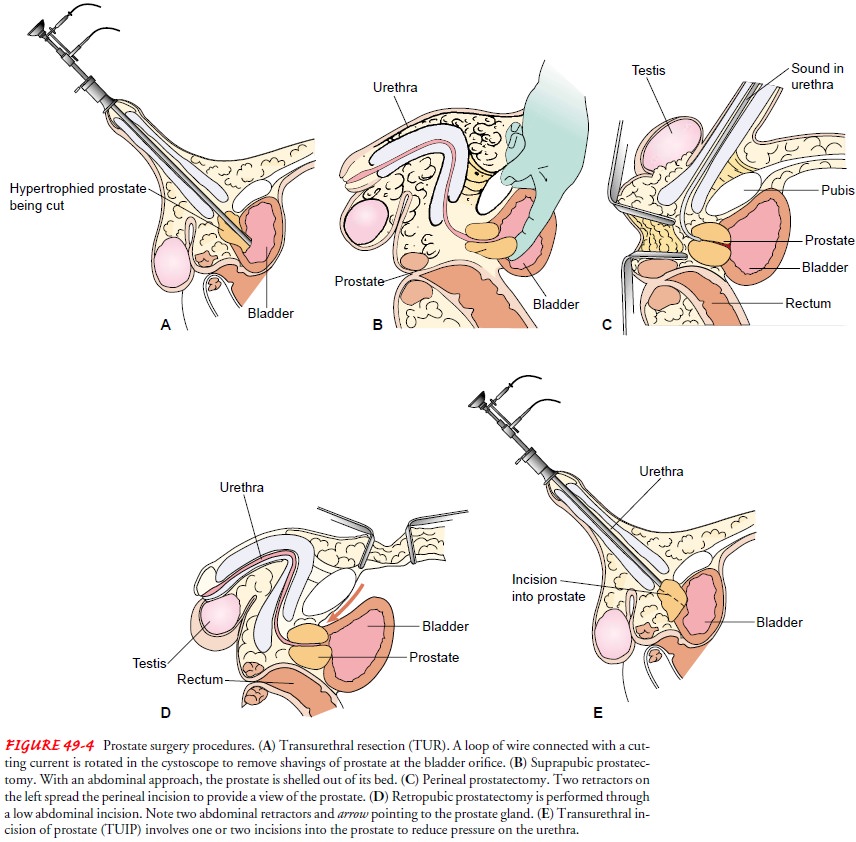
Surgical Procedures
Several
approaches can be used to remove the hypertrophied por-tion of the prostate
gland: transurethral resection of the prostate (TURP), suprapubic
prostatectomy, perineal prostatectomy, retropubic prostatectomy, and
transurethral incision of the prostate (TUIP) (Table 49-3). In these
approaches, the surgeon removes all hyperplastic tissue, leaving behind only
the capsule of the prostate. The transurethral approaches (TURP, TUIP) are
closed procedures; the other three are open procedures (ie, a sur-gical
incision is required). The procedure chosen depends on the underlying disorder,
the patient’s age and physical status, and pa-tient preference.
TRANSURETHRAL RESECTION OF THE PROSTATE
TURP, the most common procedure used, can be
carried out through endoscopy. The surgical and optical instrument is
intro-duced directly through the urethra to the prostate, which can then be
viewed directly. The gland is removed in small chips with an electrical cutting
loop (Fig. 49-4A). This procedure,
which re-quires no incision, may be used for glands of varying size and is
ideal for patients who have small glands and those who are con-sidered poor
surgical risks.
This
approach usually requires an overnight hospital stay. Strictures are more
frequent, and repeated procedures may be necessary because the residual
prostatic tissue can grow back. TURP rarely causes erectile dysfunction, but it
may cause retro-grade ejaculation because removing the prostatic tissue at the
bladder neck can cause the seminal fluid to flow backward into the bladder
rather than forward through the urethra during ejaculation.
SUPRAPUBIC PROSTATECTOMY
Suprapubic prostatectomy is one method of
removing the gland through an abdominal incision. An incision is made into the
bladder, and the prostate gland is removed from above (see Fig. 49-4B). Such an approach can be used for a
gland of any size, and few complications occur, although blood loss may be
greater than with the other methods. Another disadvantage is the need for an
abdominal incision, with the concomitant hazards of any major abdominal
surgical procedure.
PERINEAL PROSTATECTOMY
Perineal prostatectomy involves removing the
gland through an incision in the perineum (see Fig. 49-4C ). This approach is prac-tical when other approaches are not
possible and is useful for an open biopsy. Postoperatively, the wound may easily
become con-taminated because the incision is near the rectum. Incontinence,
impotence, and rectal injury are more likely with this approach.
RETROPUBIC PROSTATECTOMY
Retropubic prostatectomy, another technique,
is more common than the suprapubic approach. The surgeon makes a low ab-dominal
incision and approaches the prostate gland between the pubic arch and the
bladder without entering the bladder (see Fig. 49-4D). This procedure is suitable for large glands located high in the
pelvis. Although blood loss can be better controlled and the surgical site is
easier to visualize, infections can readily start in the retropubic space.
TRANSURETHRAL INCISION OF THE PROSTATE
Transurethral
incision of the prostate (TUIP) is another proce-dure used in treating BPH. An
instrument is passed through the urethra (see Fig. 49-4E ). One or two incisions are made in the prostate and prostate
capsule to reduce the prostate’s pressure on the urethra and to reduce urethral
constriction. TUIP is indicated when the prostate gland is small (30 g or less)
and is an effective treatment for many cases of BPH. TUIP can be performed on
an outpatient basis and has a lower complication rate than other in-vasive
prostate procedures (Mebust, 1998).
LAPAROSCOPIC RADICAL PROSTATECTOMY
Laparoscopic
radical prostatectomy is a method recently devel-oped in France. Although not
yet widespread in the United States, it is anticipated that this procedure will
be widely used in place of more extensive surgery for patients with localized
prostate cancer. The laparoscopic approach provides better visu-alization of
the surgical site and surrounding areas. Preliminary data suggest that patients
who undergo this procedure have less bleeding and reduced need for blood
transfusion, a shorter hos-pital stay, less postoperative pain, and more rapid
return to nor-mal activity compared to open radical prostatectomy (Rassweiler,
Sentker, Seemann et al., 2001). Further research is needed to as-sess long-term
outcomes.
Complications
Complications depend on the type of
prostatectomy performed and may include hemorrhage, clot formation, catheter
obstruc-tion, and sexual dysfunction. All prostatectomies carry a risk of
impotence because of potential damage to the pudendal nerves. In most
instances, sexual activity may be resumed in 6 to 8 weeks, the time required
for the prostatic fossa to heal. During ejacula-tion, the seminal fluid goes
into the bladder and is excreted with the urine. (The anatomic changes in the
posterior urethra lead to retrograde ejaculation.) A vasectomy may be performed
during surgery to prevent infection from spreading from the prostatic urethra
through the vas and into the epididymis.
After total prostatectomy (usually for
cancer), impotence al-most always results. For the patient who does not want to
give up sexual activity, options are available to produce erections suffi-cient
for sexual intercourse: prosthetic penile implants, negative-pressure (vacuum)
devices, and pharmacologic interventions.
Related Topics