Chapter: The Massage Connection ANATOMY AND PHYSIOLOGY : Integumentary System
Structure of the Skin
Structure of the Skin
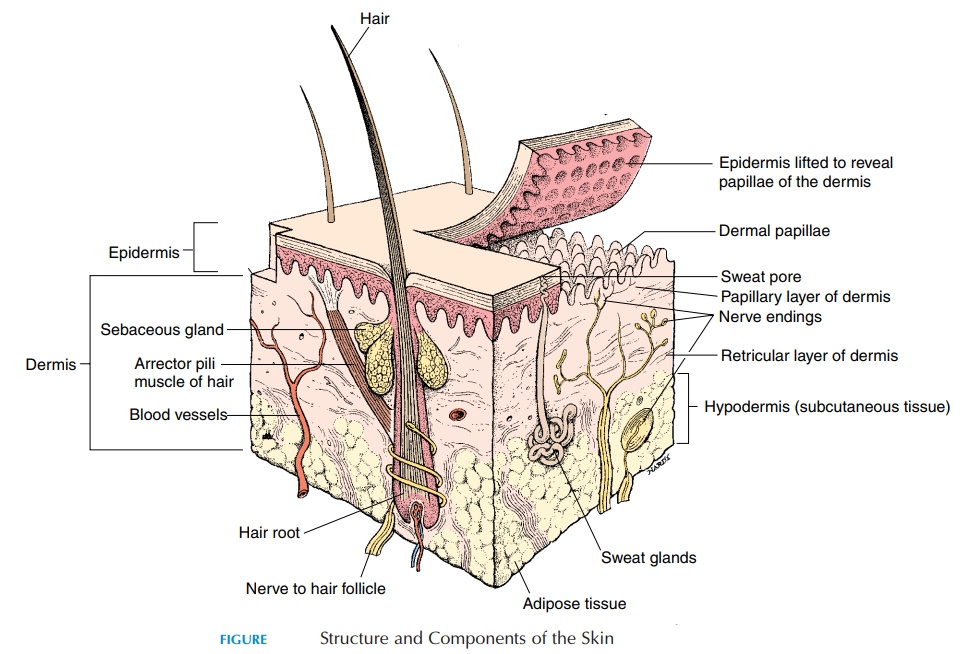
The integument consists of the cutaneous membrane, or skin, and the accessory structures, such as hair, nails, glands, muscles, and nerves (see Figure 2.1). The skin covers an area of approximately 1.5–2 m2 (59–78.7 sq in) and is responsible for about 16% of body weight. The superficial part of the skin is the epithelium, or epidermis. Deep to the epithelium is a layer of con-nective tissue, the dermis, in which the glands, hair, and nails are located. Deep to the dermis is the subcu-taneous layer, orhypodermis, which consists of looseconnective tissue and adipose tissue. This layer sepa-rates the skin from the underlying muscle, bone, and other structures.
THE EPIDERMIS
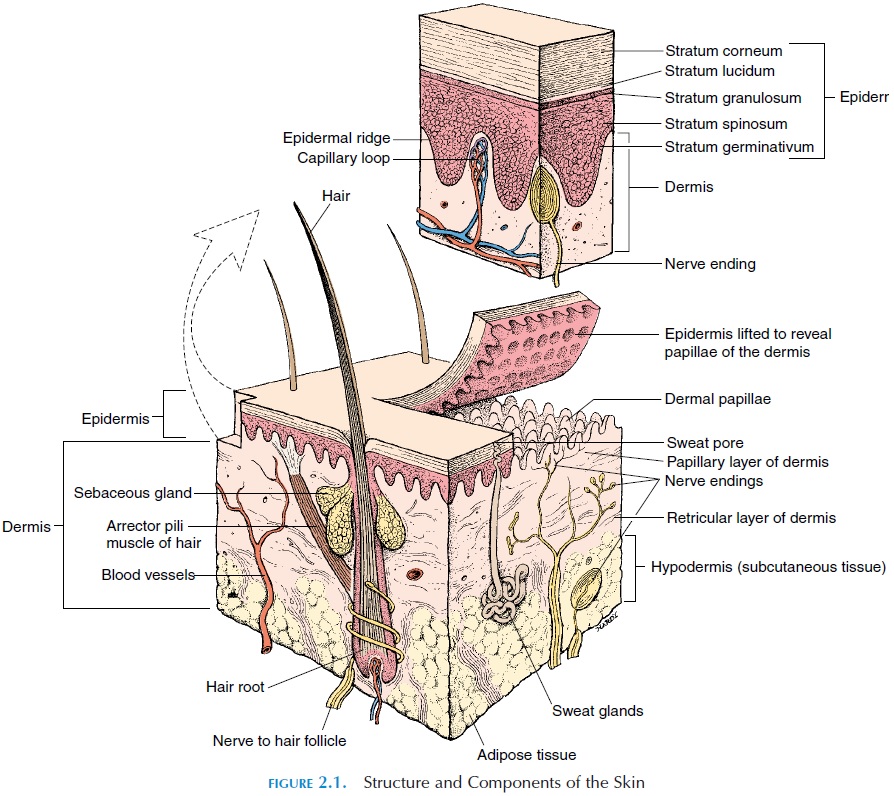
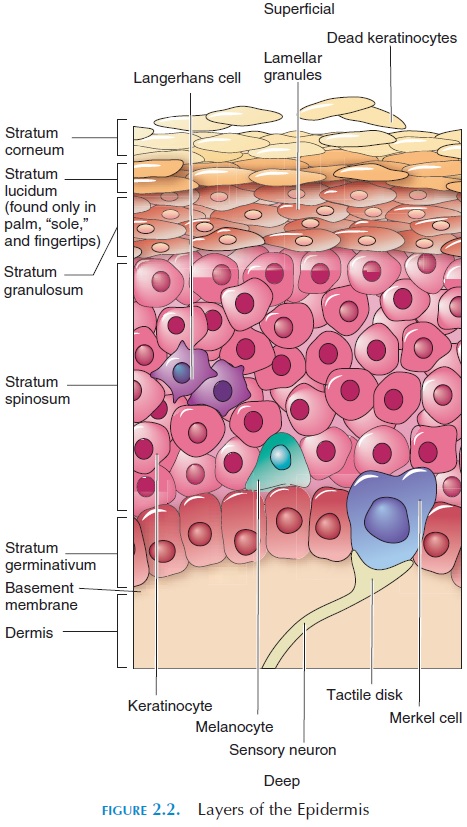
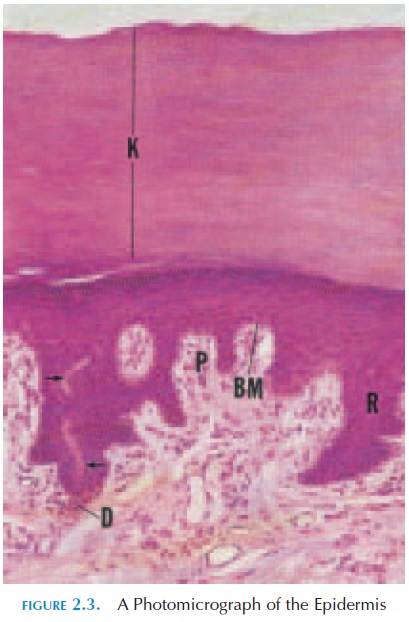
The epidermis (see Figures 2.2 and 2.3) is the most superficial layer of the skin and is composed of strat-ified squamous epithelium. The epidermis is sepa-rated from the dermis—the deeper layer—by the basement membrane. Not having a direct blood sup-ply, the epidermis relies on nutrients in the intersti-tial fluid that have diffused from the capillaries lo-cated in the dermis.
There are four types of skin cells:
· keratinocytes
· melanocytes
· Merkel cells
· Langerhans cells (Figure 2.2).
Keratinocytes make up 90% of the epidermis; they lie in many distinct layers and produce a tough fi-brous protein called keratin. Keratin helps protect the skin from heat, microorganisms, and chemicals in the environment.
The layers of the epidermis can be identified by ex-amining a section under the microscope. Beginning with the basement membrane, which separates the epidermis from the dermis, the following layers can be identified:
· stratum germinativum, or stratum basale
· stratum spinosum
· stratum granulosum
· stratum lucidum
· stratum corneum.
In areas where skin is exposed to friction, such as the palm of the hand, sole of the foot, and fingertips, the skin is thick and consists of all five layers. In other areas, such as the eyelids, the skin is thin and stratum lucidum is absent.
The Stratum Germinativum
This single-celled layer, consisting of cuboidal or columnar epithelium, is attached to the basement membrane. It is thrown into folds known as epider-mal ridges that extend into the dermis (Figure 2.2).The projections of the dermis adjacent to the ridges are known as the dermal papillae. The surface of the skin follows the ridge pattern. This pattern, referred to as whorls, is especially obvious in the palms and soles. These ridges increase friction and surface area, providing a better, more secure grip of objects. The shapes of the ridges are genetically determined and unique to an individual; they do not change with time. For this reason, fingerprints can be used for identification.
As its name suggests, this layer contains germina-tive, or basal cells, that multiply rapidly and replace cells in the superficial layer that have been lost or shed. The keratinocytes are large and contain keratin filaments in the cytoskeleton. The keratin filaments attach the cells to each other and to the basement membrane. Areas of skin that lack hair contain spe-cialized cells known as Merkel cells. These cells are in close contact with touch receptors and stimulate these sensory nerve endings. Pigment cells, known as melanocytes, are also located in this layer and are responsible for the color of the skin. Melanocytes are scattered throughout this layer and their processes extend to the more superficial layers of the skin.
Melanocytes
Melanocytes form 8% of all skin cells and manufac-ture the pigment melanin. Melanocytes contain the enzymes required for converting the amino acid tyro-sine into melanin. The melanin pigment, packaged in-side the cell in small vesicles called melanosomes, is transferred along the processes that extend into the su-perficial layers of skin. In the superficial layers, the vesicles are transferred into other cells, coloring them temporarily, until they fuse with lysosomes and are then destroyed. In individuals with light skin, less transfer of melanosomes occurs among cells, and the superficial layers lose their pigments faster. In individ-uals with dark skin, the melanosomes are larger and transfer occurs in many of the superficial layers. In-terestingly, the number of melanocytes per square mil-limeter of skin is the same for both dark- and light-skinned individuals. It is the melanin synthesis rate that is different. The number of melanocytes is in-creased in some areas of the body, such as the penis, nipples, areolae (area around the nipple), face, and limbs.
The melanin pigment protects the skin from the harmful effects of ultraviolet (UV) radiation. Expo-sure to UV rays stimulates those enzymes that pro-duce melanin and produces a “tan” skin. The tan fades when the keratinocytes containing melanin are lost. Melanin production is also increased by secre-tion of melanocyte-stimulating hormones by the an-terior pituitary gland.
Because melanin pigment is concentrated around the nucleus, it works like an umbrella, absorbing UV rays and shielding the nucleus and its high deoxyri-bonucleic acid (DNA) content. Melanin also protects the skin from sunburn. However, the rate of melanin synthesis is not rapid enough to provide complete protection; it is possible to get a sunburn easily, espe-cially in the first few days of prolonged sun exposure. Mild sunburn consists of varying degrees of redness that appear 2–12 hours after exposure to the sun. Scaling and peeling follow any overexposure to sun-light. Dark skin also burns and may appear grayish or gray–black.
The cumulative effects of UV radiation exposure can damage fibroblasts located in the dermis, leading to faulty manufacture of connective tissue and wrin-kling of the skin. UV rays also stimulate the produc-tion of oxygen free radicals that disrupt collagen and elastic fibers in the extracellular regions. Although a small amount of UV radiation is beneficial, larger amounts may cause alterations in the genetic mater-ial in the nucleus of cells—especially the rapidly mul-tiplying cells in the stratum germinativum, increas-ing the risk of cancer. Depletion of the ozone layer and overexposure to the sun may be responsible for increased incidence of skin cancer.
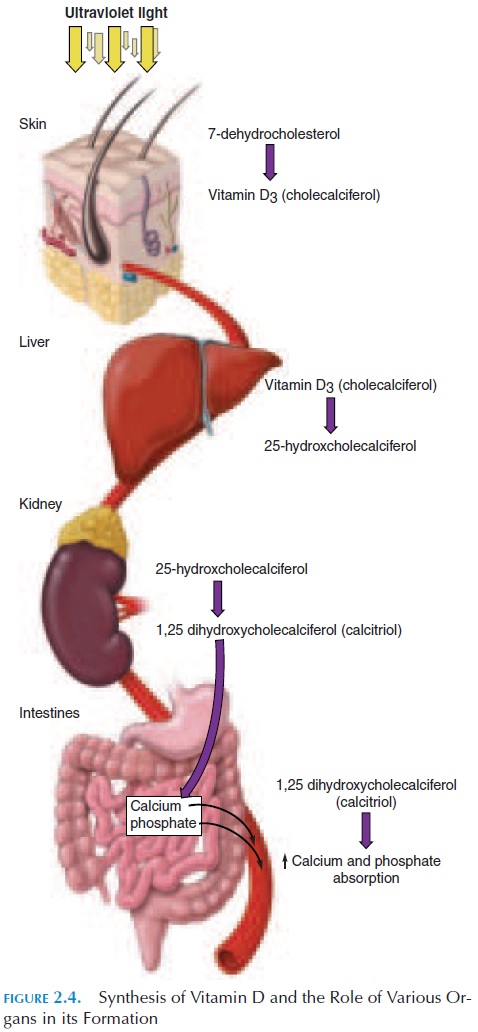
Synthesis of Vitamin D
Excessive exposure to sunlight is harmful; however, some exposure to sunlight is useful and needed by the body. The cells in the stratum germinativum and stratum spinosum convert the compound 7-dehydro-cholesterol into a precursor of vitamin D. Vitamin D is a group of closely related steroids produced by the action of ultraviolet light on 7-dehydrocholesterol. Vitamin D synthesized in the skin is transported to the liver and then to the kidneys where it is converted into a more potent form (see Figure 2.4). Vitamin D increases calcium absorption in the intestines and is an important hormone in calcium metabolism. Lack of vitamin D can lead to improper bone mineraliza-tion and a disease called rickets (in children) and os-teomalacia (in adults).
Stratum Spinosum
Stratum spinosum consists of 8–10 layers of cells lo-cated immediately above the stratum germinativum. As the cells multiply in the stratum germinativum, they are pushed upward into the stratum spinosum. Observed under the microscope, these cells have a spiny appearance, hence, their name. This layer of cells, in addition to keratinocytes, contains Langer-hans cells, which are involved in defense mecha-nisms. Langerhans cells protect the skin from pathogens and destroy abnormal cells, such as cancer cells, that may be present.
Stratum Granulosum
Stratum granulosum consists of 3–5 layers. By the time the keratinocytes reach this layer from the lay-ers below, they have flattened and stopped dividing. The cells have a granular appearance when viewed under the microscope and contain a granular protein known as keratohyalin, which organizes keratin into thicker bundles. The cells also contain lamellargranules, which release a lipid-rich secretion intothe spaces between the cells. These lipid-rich secre-tions work as a sealant and slow the loss of body flu- ids. As the cells manufacture keratohyalin, they be-come flatter and thinner and the cell membranes become thicker and impermeable to water. With time, a thick layer of interlocking keratin fibers sur-rounded by keratohyalin may be seen within the cell membrane of the original cells, which have now lost their organelles. These structural changes provide protection against pathogens and are responsible for the impermeability of skin to water.
Stratum Lucidum
Stratum lucidum, as its name indicates, is translu-cent and consists of densely packed, flat cells that are filled with keratin. This layer is more prominent in the palms of the hands and soles of the feet.
Stratum Corneum
Stratum corneum is the most superficial layer and mostly consists of dead cells and keratin. The trans-formation from live cells to the dead cells in this layer is known askeratinization, or cornification (corne, hard or hooflike). There are about 15–30 layers ofthese cells, which are periodically shed individually or in sheets. It usually takes about 15–30 days for the cells to reach this layer from the stratum germina-tivum. The cells then remain in the stratum corneum for about 14 days before they are shed. The dryness of this superficial layer, together with the coating of lipid secretions from sebaceous and sweat glands, makes the skin unsuitable for growth of microorgan-isms. If the skin is exposed to excessive friction, the layer abnormally thickens and forms a callus.
Although dead cells make the skin resistant to wa-ter, it does not prevent the loss of water by evapora-tion from the interstitial tissue. About 500 mL of wa-ter per day is lost via the skin. This loss of water is known as insensible perspiration, which is different from that actively lost by sweating, called sensibleperspiration.
Promotion of Epidermal Growth
Epidermal growth is promoted by a peptide known as epidermal growth factor (EGF). EGF is secreted by various tissues, such as the salivary gland and glands in the duodenum. This factor combines with receptors on the cell membrane of multiplying cells in the epidermis and promotes cell division, produc-tion of keratin, and development and repair after in-jury. So potent, a small sample of EGF from a per-son’s tissue has been used outside the body to form sheets of epidermal cells to cover severe burns.
THE DERMIS
The dermis is the connective tissue layer that lies deep to the epidermis. It contains protein fibers and all the cells in the connective tissue proper, such as fi-broblasts, macrophages, adipose cells, and mast cells. It supports the epidermis and is the primary source of its nutrients. The dermis contains loose connective tissue that lies closer to the epidermis (papillarylayer, or pars papillaris) and dense irregular con-nective tissue deep to the papillary layer (reticularlayer, or pars reticularis). Collagen and elastic fibersimpart strength, elasticity, and extensibility of the skin. The dermis is vascular and contains a network of blood vessels. Lymphatic vessels are also present in abundance in this layer. Accessory structures, such as sweat glands and hair follicles, are located in the der-mis. In addition, the dermis contains numerous nerve endings and nerves that convey various sensa-tions from the skin to the central nervous system.
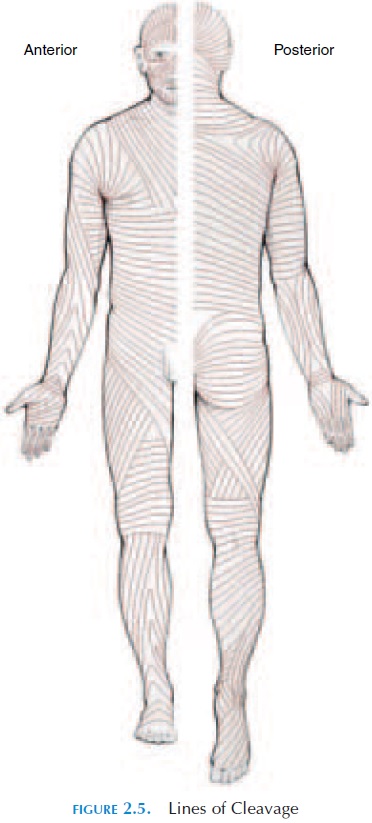
The consistency and texture of skin is largely de-termined by the water content and the collagen and elastic fibers in the dermis. The water content helps maintain the flexible and resilient properties of the skin, or the skin turgor. The collagen and elastic fibers are arranged in parallel bundles. The orienta-tion of the bundles allows the skin to resist the stress placed on it during movement. Although the elastic fibers stretch and come back to their original length, the collagen fibers are tough, resisting stretch but al-lowing twisting and bending.
Figure 2.5 shows the lines of cleavage of skin. This is the pattern of collagen and elastic fiber bun-dles established in the dermis that follow the lines of tension in the skin. The lines of cleavage are of im-portance, as injuries to the skin that are at right an-gles to these lines tend to gap because the cut elastic fibers recoil and tend to pull the wound apart. Healing is slower and there is more scarring in this type of injury compared with those injuries parallel to the lines of cleavage.
NERVE SUPPLY TO THE SKIN
The skin is supplied by autonomic nerves, which in-nervate the blood vessels and glands in the skin. Briefly, au-tonomic nerves supply glands, blood vessels, and in-ternal organs. There are two types: sympathetic and parasympathetic.
Sympathetic stimulation and circulating epineph-rine and norepinephrine produce vasoconstriction. There are no known vasodilator fibers to the cuta-neous blood vessels; dilation is caused by a decrease in the constrictor tone of the sympathetic nerves. Chemicals, such as bradykinin from sweat glands,histamine from mast cells, and vasodilator metabo-lites from injured cells, have a direct effect on the cal-iber of blood vessels.
In addition to the autonomic nerves, there are nu-merous sensory receptors, which respond to sensa-tions such as touch, pressure, pain, cold, and warmth. Mild stimulations, especially if produced by some-thing that moves across the skin, cause itching and tickling sensations . Any given receptor signals or responds to only one kind of cutaneous sen-sation. The receptors may be free nerve endings or modified to form special structures that have a sur-rounding capsule or expanded tips. Some are found wound around hair follicles. The number of sensory receptors per unit area varies from region to region. More receptors are present in areas, such as the face, lips, and fingers, that are more sensitive to sensations.
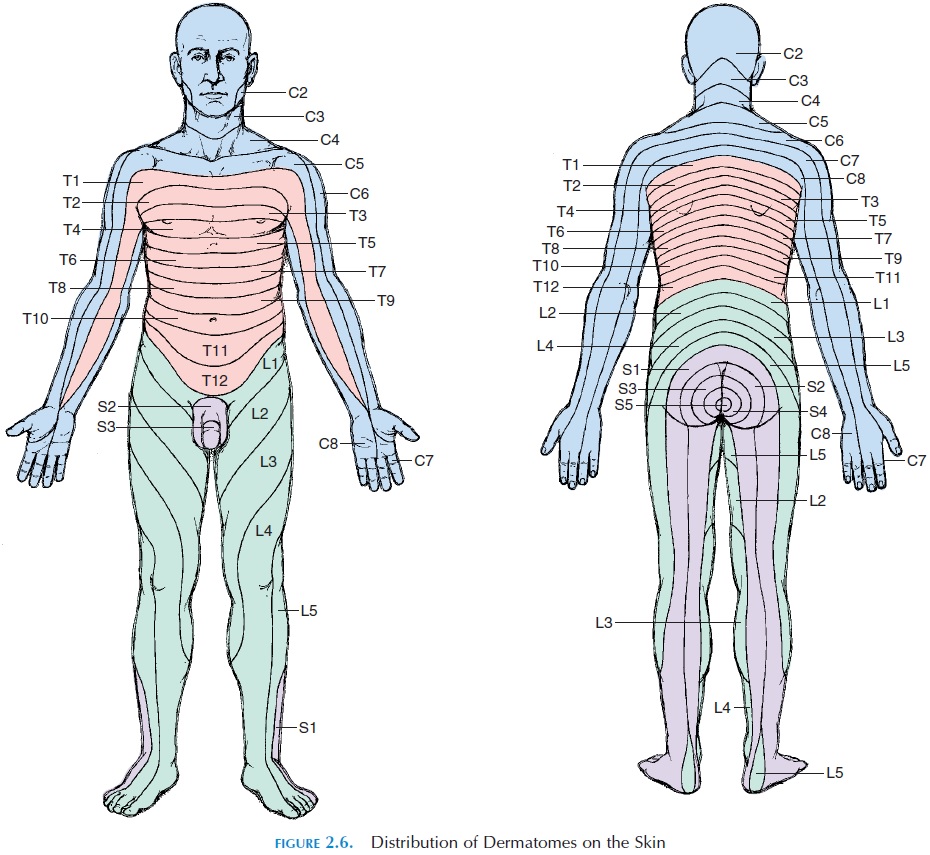
The receptors are continuous with sensory nerves. Sensory nerves from the skin take the impulses gen-erated in the receptors to the central nervous system. The sensory nerves from a specific area of the skin en-ter a particular segment of the spinal cord. The area of skin supplied by the nerves from a particular spinal segment is known as the dermatome. The der-matomes of the different spinal nerves throughout the surface of the body have been traced (see Figure 2.6). These patterns are of clinical importance as damage to a spinal nerve results in loss of sensation in the specific dermatome.
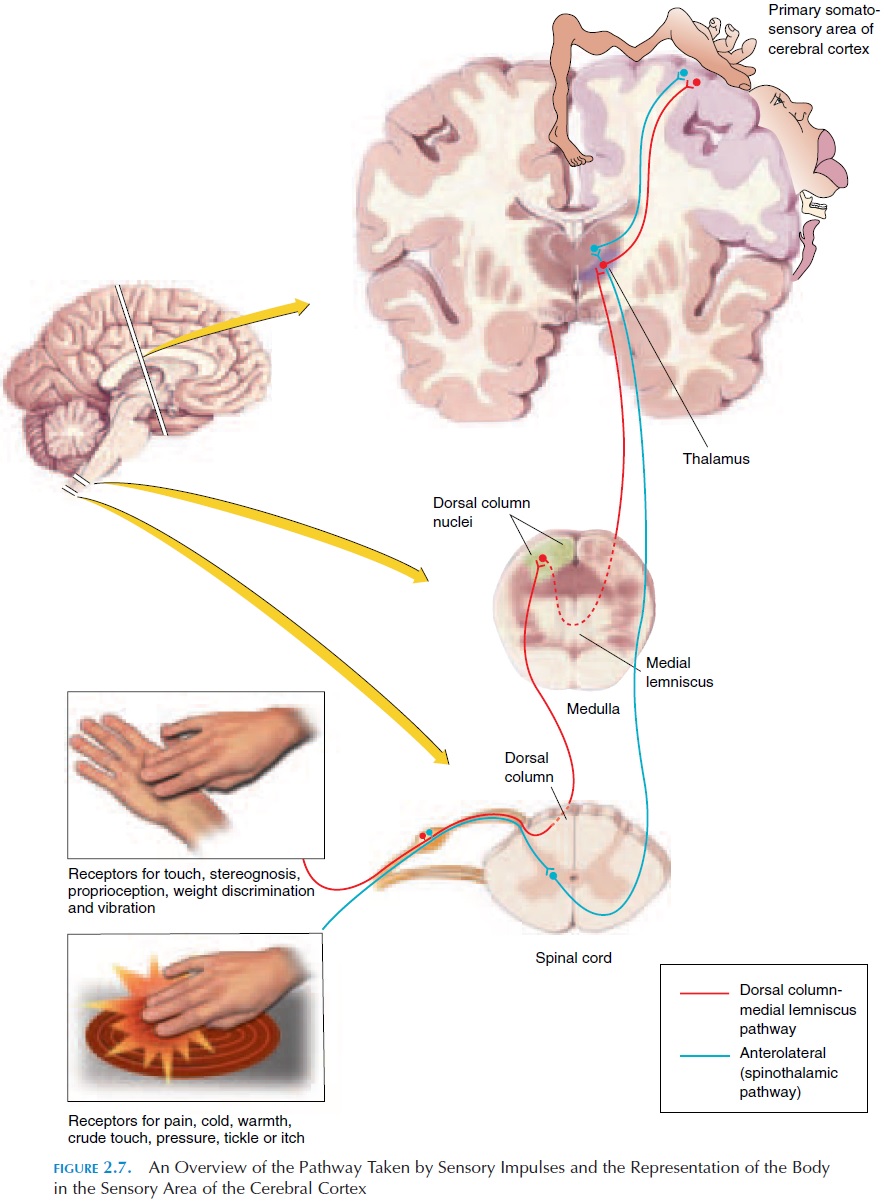
The intimate association between the skin and the brain can be appreciated by the fact that the brain has a map, representing the entire body, in the area that perceives sensations. There is a larger represen-tation for regions that are more sensitive than others (see Figure 2.7). The pathway taken by impulses gen-erated by the sensory receptors of the skin is also very specific. This is why we are able to locate exactly—up to a few millimeters—where we have been touched on the skin. Many consider the skin an extension of the brain through which interactions between the mind and body can be made by touch. It is interest-ing to note that during prenatal development, both the skin and the nervous system are derived from the same embryonic layer, the ectoderm (in the embryo, all the structures of the body are derived from three layers—ectoderm, mesoderm, and endoderm).
BLOOD CIRCULATION IN THE SKIN
The skin has an extensive blood supply; 8–10% of the total blood flow in the body can be found in the skin. The heat lost from the body is regulated by altering the volume of blood flowing through the skin.
The arteries supplying the skin form a network at the junction of the subcutaneous layer with the der-mis. This junction is known as the cutaneousplexus. Branches from these arteries supply the adi-pose tissue located in the subcutaneous layer. Other branches supply the accessory structures as they travel toward the epidermis. These branches form an-other network at the junction of the dermis and epi-dermis that follows the contours of the papilla. This junction is known as the papillary plexus. The cap- illaries at this junction join and rejoin to form venules and veins. In many regions, such as the fin-gers, palms, toes, and ear lobes, direct connections, known asarteriovenous anastomoses, link arteri-oles and venules. These links allow blood diversion, without it entering the superficial capillaries from which heat dissipates.
The blood vessels to the skin are well innervated by the autonomic nervous system. Blood flow can vary widely in response to changing temperatures, from as little as 1 mL to 150 mL/100 g of skin per minute. The plexuses in the skin, to some extent, serve as blood reservoirs. When blood is lost, these vessels constrict, propelling blood into the systemic circulation to maintain blood flow to the vital organs.
Related Topics