Chapter: Medical Physiology: Fetal and Neonatal Physiology
Special Functional Problems in the Neonate
Special Functional Problems in the Neonate
An important characteristic of the neonate is instability of the various hormonal and neurogenic control systems. This results partly from immature development of the different organs of the body and partly from the fact that the control systems simply have not become adjusted to the new way of life.
Respiratory System
The normal rate of respiration in a neonate is about 40 breaths per minute, and tidal air with each breath aver-ages 16 milliliters. This gives a total minute respiratory volume of 640 ml/min, which is about twice as great in relation to the body weight as that of an adult. The func-tional residual capacity of the infant’s lungs is only one half that of an adult in relation to body weight. Thisdifference causes excessive cyclical increases and decreases in the newborn baby’s blood gas concentra-tions if the respiratory rate becomes slowed because it is the residual air in the lungs that smooths out the blood gas variations.
Circulation
Blood Volume. The blood volume of a neonate immedi-ately after birth averages about 300 milliliters, but if the infant is left attached to the placenta for a few minutes after birth or if the umbilical cord is stripped to force blood out of its vessels into the baby, an additional 75 milliliters of blood enters the infant, to make a total of 375 milliliters. Then, during the ensuing few hours, fluid is lost into the neonate’s tissue spaces from this blood, which increases the hematocrit but returns the blood volume once again to the normal value of about 300 mil-liliters. Some pediatricians believe that this extra blood volume caused by stripping the umbilical cord can lead to mild pulmonary edema with some degree of respira-tory distress, but the extra red blood cells are often very valuable to the infant.
Cardiac Output. The cardiac output of the neonateaverages 500 ml/min, which, like respiration and body metabolism, is about twice as much in relation to body weight as in the adult. Occasionally a child is born with an especially low cardiac output caused by hemorrhage of much of its blood volume from the placenta at birth.
Arterial Pressure. The arterial pressure during the firstday after birth averages about 70 mm Hg systolic and 50 mm Hg diastolic; this increases slowly during the next several months to about 90/60. Then there is a much slower rise during the subsequent years until the adult pressure of 115/70 is attained at adolescence.
Blood Characteristics. The red blood cell count in theneonate averages about 4 million per cubic millimeter. If blood is stripped from the cord into the infant, the red blood cell count rises an additional 0.5 to 0.75 million during the first few hours of life, giving a red blood cell count of about 4.75 million per cubic millimeter, as shown in Figure 83–6. Subsequent to this, however, few new red blood cells are formed in the infant during the first few weeks of life, presumably because the hypoxic stimulus of fetal life is no longer present to stimulate red cell production. Thus, as shown in Figure 83–6, the average red blood cell count falls to less than 4 million per cubic millimeter by about 6 to 8 weeks of age. From that time on, increasing activity by the baby provides the appropriate stimulus for returning the red blood cell
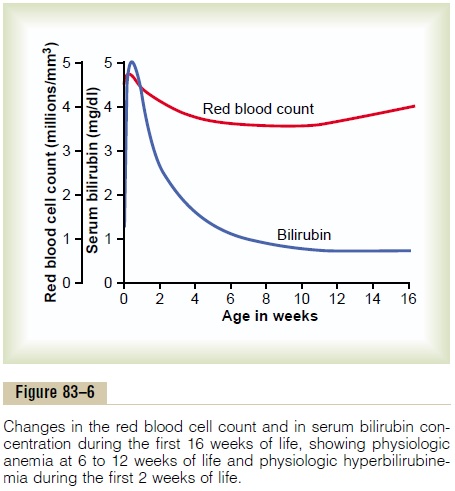
count to normal within another 2 to 3 months. Immedi-ately after birth, the white blood cell count of the neonate is about 45,000 per cubic millimeter, which is about five times as great as that of the normal adult.
Neonatal Jaundice and Erythroblastosis Fetalis. Biliru-bin formed in the fetus can cross the placenta into the mother and be excreted through the liver of the mother, but immediately after birth, the only means for ridding the neonate of bilirubin is through the neonate’s own liver, which for the first week or so of life functions poorly and is incapable of conjugating signi-ficant quantities of bilirubin with glucuronic acid for excretion into the bile. Consequently, the plasma biliru-bin concentration rises from a normal value of less than 1 mg/dl to an average of 5 mg/dl during the first 3 days of life and then gradually falls back to normal as the liver becomes functional. This effect, called physiologichyperbilirubinemia, is shown in Figure 83–6, and itis associated with mild jaundice (yellowness) of the infant’s skin and especially of the sclerae of its eyes for a week or two.
However, by far the most important abnormal cause of serious neonatal jaundice is erythroblastosis fetalis. Briefly, the erythroblastotic baby inherits Rh-positive red cells from the father, while the mother is Rh negative. The mother then becomes immunized against the Rh-positive factor (a protein) in the fetus’s blood cells, and her antibodies destroy fetal red cells, releasing extreme quantities of bilirubin into the fetus’s plasma and often causing fetal death for lack of ade-quate red cells. Before the advent of modern obstetri-cal therapeutics, this condition occurred either mildly or seriously in 1 of every 50 to 100 neonates.
Fluid Balance, Acid-Base Balance, and Renal Function
The rate of fluid intake and fluid excretion in the newborn infant is seven times as great in relation to weight as in the adult, which means that even a slight percentage alteration of fluid intake or fluid output can cause rapidly developing abnormalities.
The rate of metabolism in the infant is also twice as great in relation to body mass as in the adult, which means that twice as much acid is normally formed, which gives a tendency toward acidosis in the infant. Functional development of the kidneys is not complete until the end of about the first month of life. For instance, the kidneys of the neonate can concentrate urine to only 1.5 times the osmolality of the plasma instead of the adult three to four times. Therefore, considering the immaturity of the kidneys, together with the marked fluid turnover in the infant and rapid formation of acid, one can readily understand that among the most important problems of infancy are acidosis, dehydration, and, more rarely, overhydration.
Liver Function
During the first few days of life, liver function in the neonate may be quite deficient, as evidenced by the following effects:
1.The liver of the neonate conjugates bilirubin with glucuronic acid poorly and therefore excretes bilirubin only slightly during the first few days of life.
2.The liver of the neonate is deficient in forming plasma proteins, so that the plasma protein concentration falls during the first weeks of life to 15 to 20 per cent less than that for older children. Occasionally the protein concentration falls so low that the infant develops hypoproteinemic edema.
3.The gluconeogenesis function of the liver is particularly deficient. As a result, the blood glucose level of the unfed neonate falls to about 30 to 40 mg/dl (about 40 per cent of normal), and the infant must depend mainly on its stored fats for energy until sufficient feeding can occur.
4. The liver of the neonate usually also forms too little of the blood factors needed for normal blood coagulation.
Digestion, Absorption, and Metabolism of Energy Foods; and Nutrition
In general, the ability of the neonate to digest, absorb, and metabolize foods is no different from that of the older child, with the following three exceptions.
First, secretion of pancreatic amylase in the neonate is deficient, so that the neonate uses starches less ade-quately than do older children.
Second, absorption of fats from the gastrointestinal tract is somewhat less than that in the older child. Con-sequently, milk with a high fat content, such as cow’s milk, is frequently inadequately absorbed.
Third, because the liver functions imperfectly during at least the first week of life, the glucose concentration in the blood is unstable and low.
The neonate is especially capable of synthesizing and storing proteins. Indeed, with an adequate diet, as much as 90 per cent of the ingested amino acids are used for formation of body proteins. This is a much higher per-centage than in adults.
Metabolic Rate and Body Temperature. The normal meta-bolic rate of the neonate in relation to body weight is about twice that of the adult, which accounts also for the twice as great cardiac output and twice as great minute respiratory volume in relation to body weight in the infant.
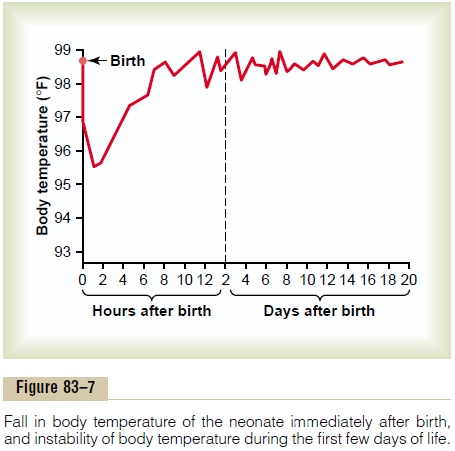
Because the body surface area is large in relation to body mass, heat is readily lost from the body. As a result, the body temperature of the neonate, particularly of premature infants, falls easily. Figure 83–7 shows that the body temperature of even a normal infant often falls several degrees during the first few hours after birth but returns to normal in 7 to 10 hours. Still, the body tem-perature regulatory mechanisms remain poor during the early days of life, allowing marked deviations in temperature, which are also shown in Figure 83–7.
Nutritional Needs During the Early Weeks of Life. At birth, aneonate is usually in complete nutritional balance, pro-vided the mother has had an adequate diet. Further-more, function of the gastrointestinal system is usually more than adequate to digest and assimilate all the nutritional needs of the infant if appropriate nutrients are provided in the diet. However, three specific prob-lems do occur in the early nutrition of the infant.
Need for Calcium and Vitamin D
The neonate is in a stage of rapid ossification of its bones at birth, so that a ready supply of calcium throughout infancy is needed. This is ordinarily supplied adequately by the usual diet of milk. Yet absorption of calcium by the gastrointestinal tract is poor in the absence of vitamin D. Therefore, the vitamin D– deficient infant can develop severe rickets in only a few weeks. This is particularly true in premature babies because their gastrointestinal tracts absorb calcium even less effectively than those of normal infants.
Necessity for Iron in the Diet
If the mother has had adequate amounts of iron in her diet, the liver of the infant usually has stored enough iron to keep forming blood cells for 4 to 6 months after birth. But if the mother has had insufficient iron in her diet, severe anemia is likely to occur in the infant after about 3 months of life. To prevent this possibility, early feeding of the infant with egg yolk, which contains rea-sonably large quantities of iron, or the administration of iron in some other form is desirable by the second or third month of life.
Vitamin C Deficiency in Infants
Ascorbic acid (vitamin C) is not stored in significant quantities in the fetal tissues; yet it is required for proper formation of cartilage, bone, and other intercel-lular structures of the infant. Furthermore, milk has poor supplies of ascorbic acid, especially cow’s milk, which has only one fourth as much as human milk. For this reason, orange juice or other sources of ascorbic acid are often prescribed by the third week of life.
Immunity
The neonate inherits much immunity from the mother because many protein antibodies diffuse from the mother’s blood through the placenta into the fetus. However, the neonate does not form antibodies of its own to a significant extent. By the end of the first month, the baby’s gamma globulins, which contain the anti-bodies, have decreased to less than one half the original level, with a corresponding decrease in immunity.There-after, the baby’s own immunity system begins to form antibodies, and the gamma globulin concentration returns essentially to normal by the age of 12 to 20 months.
Despite the decrease in gamma globulins soon after birth, the antibodies inherited from the mother protect the infant for about 6 months against most major child-hood infectious diseases, including diphtheria, measles, and polio. Therefore, immunization against these diseases before 6 months is usually unnecessary. Conversely, the inherited antibodies against whooping cough are normally insufficient to protect the neonate; therefore, for full safety, the infant requires immuniza-tion against this disease within the first month or so of life.
Allergy. The newborn infant is seldom subject to allergy.Several months later, however, when the infant’s own antibodies first begin to form, extreme allergic states can develop, often resulting in serious eczema, gas-trointestinal abnormalities, and even anaphylaxis. As the child grows older and still higher degrees of immu-nity develop, these allergic manifestations usually dis-appear.
Endocrine Problems
Ordinarily, the endocrine system of the infant is highly developed at birth, and the infant seldom exhibits any immediate endocrine abnormalities. However, there are special instances in which the endocrinology of infancy is important:
1. If a pregnant mother bearing a female child is treated with an androgenic hormone or if an androgenic tumor develops during pregnancy, the child will be born with a high degree of masculinization of her sexual organs, thus resulting in a type of hermaphroditism.
2.The sex hormones secreted by the placenta and by the mother’s glands during pregnancy occasionally cause the neonate’s breasts to form milk during the first days of life. Sometimes the breasts then become inflamed, or infectious mastitis develops.
3.An infant born of an untreated diabetic mother will have considerable hypertrophy and hyperfunction of the islets of Langerhans in the pancreas.As a consequence, the infant’s blood glucose concentration may fall to lower than 20 mg/dl shortly after birth. Fortunately, however, in the neonate, unlike in the adult, insulin shock or coma from this low level of blood glucose concentration only rarely develops.
Maternal type II diabetes is the most common cause of large babies. Type II diabetes in the mother is associated with resistance to the metabolic effects of insulin and compensatory increases in plasma insulin concentration. The high levels of insulin are believed to stimulate fetal growth factor and contribute to increased birth weight. Increased supply of glucose and other nutrients to the fetus may also contribute to increased fetal growth. However, most of the increased fetal weight is due to increased body fat; there is usually little increase in body length although the size of some organs may be increased (organomegaly).
In the mother with uncontrolled type I diabetes (caused by lack of insulin secretion), fetal growth may be stunted because of metabolic deficits in the mother, and growth and tissue maturation of the neonate are often impaired. Also, there is a high rate of intrauterine mortality, and among those fetuses that do come to term, there is still a high mortality rate. Two thirds of the infants who die succumb to respiratory distress syndrome.
4.Occasionally a child is born with hypofunctional adrenal cortices, often resulting from agenesis of the adrenal glands or exhaustion atrophy, which can occur when the adrenal glands have been vastly overstimulated.
5.If a pregnant woman has hyperthyroidism or is treated with excess thyroid hormone, the infant is likely to be born with a temporarily hyposecreting thyroid gland. Conversely, if before pregnancy a woman had had her thyroid gland removed, her pituitary gland may secrete great quantities of thyrotropin during gestation, and the child might be born with temporary hyperthyroidism.
6.In a fetus lacking thyroid hormone secretion, the bones grow poorly and there is mental retardation. This causes the condition called cretin dwarfism.
Related Topics