Chapter: Clinical Dermatology: Drug eruptions
Some common reaction patterns and drugs which can cause them
Some
common reaction patterns and drugs which can cause them
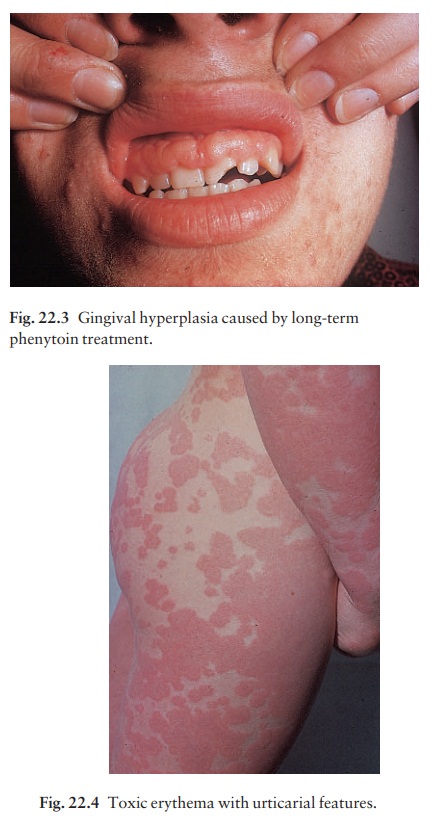
Toxic (reactive) erythema
This vague term describes the most common type of drug eruption, looking sometimes like measles or scarlet fever, and sometimes showing prominent urticarial Fig. 22.4) or erythema multiforme-like elements. Itching and fever may accompany the rash. Culprits include antibiotics (especially ampicillin), sulphonamides and related compounds (diuretics and hypoglycaemics), bar-biturates, phenylbutazone and para-aminosalicylate (PAS).
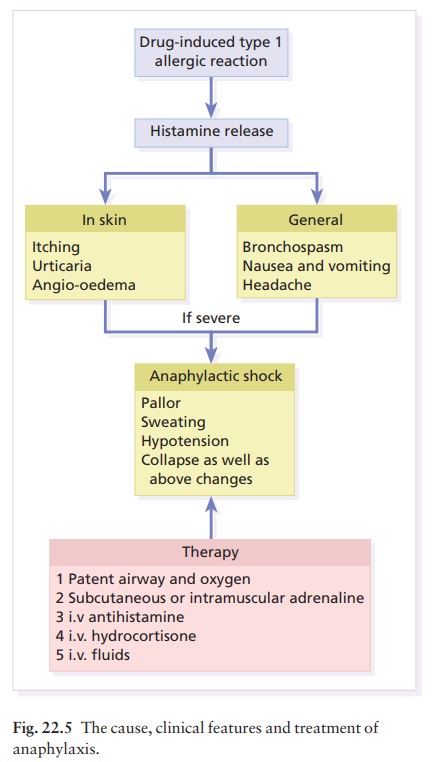
Urticaria
Many
drugs may cause this but salicylates are the most common, often working
non-immunologically as histamine releasers. Antibiotics are also often to
blame. Insect repellents and nitrogen mustards can cause urticaria on contact.
Urticaria may be part of a severe and generalized reaction (anaphylaxis) that
includes bronchospasm and collapse (Fig. 22.5).
Allergic vasculitis
The
clinical changes range from urticarial papules, through palpable purpura, to
necrotic ulcers. Erythema nodosum may occur. Sulphonamides,
phenylbutazone,indomethacin (indometacin), phenytoin and oral con-traceptives
are among the possible causes.
Erythema multiforme
Target-like
lesions appear mainly on the extensor aspects of the limbs, and bullae may
form. In the Stevens–Johnson syndrome, the patients are often ill and the
mucous membranes are severely affected. Sulphonamides, barbiturates,
lamotrigine and phenyl-butazone are known offenders.
Purpura
The
clinical features are seldom distinctive apart from the itchy brown petechial
rash on dependent areas that is characteristic of carbromal reactions.
Thrombocytopenia and coagulation defects should be excluded . Thiazides,
sulphonamides, phenylbutazone, sulphonylureas, barbiturates and quinine are
among the drugs reported to cause purpura.
Bullous eruptions
Some
of the reactions noted above can become bullous. Bullae may also develop at
pressure sites in drug-induced coma.
Eczema
This
is not a common pattern and occurs mainly when patients sensitized by topical
applications are given the drug systemically. Penicillin, sulphonamides,
neo-mycin, phenothiazines and local anaesthetics should be considered.
Exfoliative dermatitis
The
entire skin surface becomes red and scaly. This can be caused by drugs
(particularly phenylbutazone, PAS, isoniazid and gold), but can also be caused
by widespread psoriasis and eczema.
Fixed drug eruptions
Round, erythematous or purple, and sometimes bullous plaques recur at the same site each time the drug is taken (Fig. 22.6).

Pigmentation persists between acute episodes. The glans penis seems to be a favoured site. The causes of fixed drug eruptions in any country follow the local patterns of drug usage there; but these change as old drugs drop out of use and are replaced by new ones with an unknown potential for causing this type of reaction. For example, in the UK, three of the four most common causes of fixed drug eruptions in 1970 (barbiturates, phenolphthalein and oxyphen-butazone) are no longer common causes. Paracetamol is currently the most common offender in the UK; trimethoprim-sulfa leads the list in the USA. Non-steroidal anti-inflammatory drugs (NSAIDs; includ-ing aspirin), antibiotics, systemic antifungal agents and psychotropic drugs lie high on the list of other possible offenders.
Acneiform eruptions
Lithium,
iodides, bromides, oral contraceptives, an-drogens or glucocorticosteroids,
antituberculosis and anticonvulsant therapy may cause an acneiform rash .
Lichenoid eruptions
These resemble lichen planus , but not always very closely as mouth lesions are uncommon and as scaling and eczematous elements may be seen. Consider antimalarials, NSAIDs, gold, phenothiazines and PAS.
Toxic epidermal necrolysis
In
adults, this ‘scalded skin’ appearance is usually drug-induced (e.g.
sulphonamides, barbiturates, phenylbu-tazone, oxyphenbutazone, phenytoin,
carbamazepine, lamotrigine or penicillin).
Hair loss
This
is a predictable side-effect of acitretin and cytotoxic agents, an
unpredictable response to some anticoagulants, and sometimes seen with
antithyroid drugs. Diffuse hair loss may occur during, or just after, the use
of an oral contraceptive.
Hypertrichosis
This
is a dose-dependent effect of diazoxide, minoxidil and cyclosporin A.
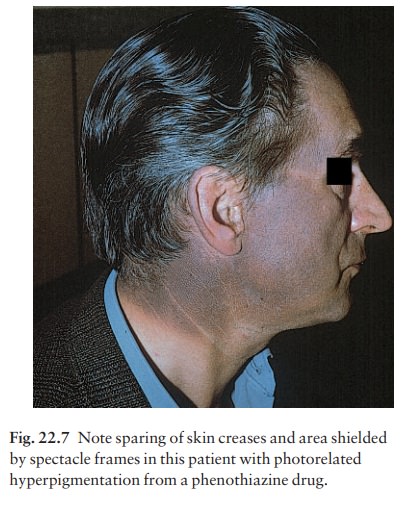
Pigmentation
Chloasma may follow an oral contraceptive plus sun
exposure. Large doses of phenothiazines impart a blue-grey colour to exposed
areas (Fig. 22.7); heavy metals can cause a generalized browning; clofazimine
makes the skin red; mepacrine turns the skin yellow; and minocycline turns leg
skin a curious greenish grey colour that suggests a bruise.
Photosensitivity
This
is dealt earily. Always exclude the common drug causes (thiazides,
tetracyclines, phenothiazines, sulphonamides or psoralens).
Xerosis
The
skin can become rough and scaly in patients receiving oral retinoids, nicotinic
acid or lithium.
Exacerbation of pre-existing skin conditions
Psoriasis
and acne are good examples of this. Psoriasis may be made worse by giving β-blockers, antimalarials, terbinafine or lithium.
Glucocorticoids, progesterone, androgens, anticonvulsants, bromides, iodidies
and lithium may exacerbate acne.
Related Topics