Chapter: Essentials of Psychiatry: Anxiety Disorders: Social and Specific Phobias
Social and Specific Phobias: Psychosocial Treatments
Psychosocial Treatments
Specific Phobias
Numerous studies have shown that exposure-based treatments are effective
for helping patients to overcome a variety of specificphobias including fears
of blood, injections dentists, spiders, snakes, rats), enclosed places, thunder
and lightning, water, flying, heights, choking and balloons. Furthermore, the
way in which exposure is conducted may make a difference. Exposure-based
treatments can vary on a variety of dimensions including the degree of
therapist involvement, duration and intensity of exposure, frequency and number
of sessions, and the degree to which the feared situation is confronted in
imagination versus in real life. In addition, because individuals with certain
specific phobias often report a fear of panicking in the feared situation,
investigators have suggested that adding various panic manage-ment strategies
(e.g., cognitive restructuring, exposure to feared sensations) may help to
increase the efficacy of behavioral treat-ments for specific phobias. It
remains to be shown whether the addition of these strategies will improve the
efficacy of treat-ments that include only exposure.
Exposure seems to work best when sessions are spaced close together.
Secondly, prolonged exposure seems to be more effective than exposure of
shorter duration. Thirdly, during ex-posure sessions, patients should be
discouraged from engaging in subtle avoidance strategies (e.g., distraction)
and over-reliance on safety signals (e.g., being accompanied by one’s spouse
during ex-posure). Fourth, real-life exposure is more effective than exposure
in imagination. Fifthly, exposure with some degree of therapist involvement
seems to be more effective than exposure that is ex-clusively conducted without
the therapist present. Exposure may be conducted gradually or quickly. Both
approaches seem to work equally well, although patients may be more compliant
with a grad-ual approach. Finally, in the case of blood and injection phobias,
the technique called applied muscle tension should be considered as an
alternative or addition to exposure therapy. Applied muscle tension involves
having patients repeatedly tense their muscles, which leads to a temporary
increase in blood pressure and pre-vents fainting upon exposure to blood or
medical procedures.
Cognitive strategies have also been used either alone or in conjunction
with exposure for treating specific phobias. The evidence suggests that the
addition of cognitive strategies to ex-posure may provide added benefit for
some individuals. For a de-tailed guide to integrating cognitive strategies
with exposure see Antony and Swinson (2000).
Specific phobias are among the most treatable of the anxi-ety disorders.
For example, in as little as one session of guided exposure lasting 2 to 3
hours, the majority of individuals with animal or injection phobias are judged
much improved or com-pletely recovered. A recent study demonstrated that one
session of exposure treatment was effective in the treatment of children and
adolescents with various specific phobias and exposure con-ducted with a parent
present was equally effective as exposure treatment conducted alone. However,
despite how straightfor-ward the concept of exposure may seem, many subtle
clinical issues can lead to problems in implementing exposure-based treatments.
For example, although a patient might be compliant with therapist-assisted exposure
practices, he or she may refuse to attempt exposure practices alone between
sessions. In such cases, involving a spouse or other family member as a coach
dur-ing practices at home may help. In addition, gradually increasing the
distance between therapist and patient during the therapist-assisted exposures
will help the patient to feel comfortable when practicing alone. However, to
maintain the patient’s trust and to maximize the effectiveness of behavioral
interventions, it is im-portant that exposure practices proceed in a
predictable way, so that the patient is not surprised by unexpected events.
Several self-help
books and manuals for treating a range of specific pho-bias have been published
in the past decade. Whereas some of these manuals were developed to be used
with the assistance of a therapist (Bourne, 1998; Antony et al., 1995;
Craske et al., 1997),
others were developed for self-administration (Brown, 1996).
Recent developments in technology have started to have an impact on the
treatment of specific phobias. Videotapes are com-monly used to show feared
stimuli to patients during exposure. Computer administered treatments have also
been used. More recent is the use of virtual reality to expose patients to
simulated situations that are more difficult to replicate in vivo such as flying (Kahan et
al., 2000) and heights (Rothbaum et
al., 1995). Emerg-ing data on the effectiveness of virtual reality is
encouraging. However, other preliminary studies indicate that in vivo exposure is still superior
(Dewis et al., 2001).
Social Phobia
Empirically validated psychosocial interventions for social pho-bia have
primarily come from a cognitive–behavioral perspec-tive and include four main
types of treatment: 1) exposure-based strategies; 2) cognitive therapy; 3)
social skills training; and 4) applied relaxation. Exposure-based treatments
involve repeat-edly approaching fear-provoking situations until they no longer
elicit fear. Through repeated exposure, patients learn that their fearful
predictions do not come true despite their having con-fronted the situation.
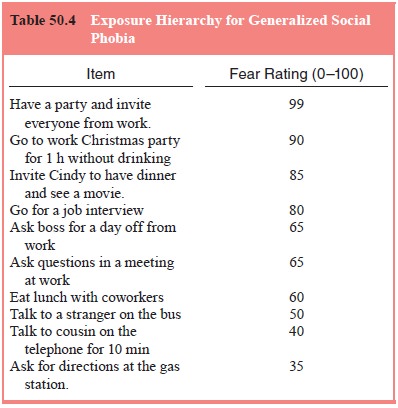
Table 50.4 illustrates an example of an ex-posure hierarchy that might be used
to structure a patient’s expo-sure practices. An exposure hierarchy is a list
of feared situations that are rank ordered by difficulty and used to guide
exposure practices for phobic disorders including social phobia and specific
phobia. The patient and therapist generate a list of situations that the
patient finds anxiety provoking. Items are placed in descend-ing order from
most anxiety provoking to least anxiety provok-ing, and each item is rated with
respect to how anxious the patient might be to practice the item. Exposure
practices are designed to help the patient become more comfortable engaging in
the activi-ties from the hierarchy. Cognitive therapy helps patients identify
and change anxious thoughts (e.g., “Others will think I am stupid
if I participate in a conversation at work”) by teaching them to
consider alternative ways of interpreting situations and to exam-ine the
evidence for their anxious beliefs. Social skills training is designed to help
patients to become more socially competent when they interact with others.
Treatment strategies may include modeling, behavioral rehearsal, corrective
feedback, social rein-forcement and homework assignments. Finally, applied
relaxa-tion involves learning to relax one’s muscles during rest, during
movement and eventually in anxiety-provoking social situations.
Although these methods are presented as four distinct treatment
approaches, there is often overlap among the various treatments. Social skills
training typically requires exposure to the phobic situation so that new skills
may be practiced (e.g., behavioral rehearsal). The same may be said of applied
relaxa-tion, which includes learning to conduct relaxation exercises in the
phobic situation. In fact, most treatments for social phobia involve some type
of exposure to anxiety-provoking social inter-actions and performance-related
tasks. Furthermore, many cog-nitive–behavioral therapists treat patients using
several different strategies delivered in a comprehensive package.
Studies demonstrating the efficacy of CBT for social phobia are too
numerous to describe in detail. Several studies have compared various
cognitive–behavioral strategies and their combinations for treating social
phobia. For example, Wlazlo and colleagues (1990) compared social skills
training to ex-posure therapy conducted either individually or in groups. All
three treatments led to significant improvements and there were no differences
between treatments. However, exposure therapy conducted in groups tended to be
more effective for the subset of patients with social skills deficits, most
likely by enabling those individuals with deficits to develop their skills
through exposure to social situations and interactions in the group. There is
con-flicting evidence that guided exposure is more effective when cognitive
therapy is included than when exposure is conducted without cognitive therapy.
Heimberg and colleagues (1990) compared supportive psy-chotherapy with a
comprehensive CBGT package that included exposure to simulated and real social
situations as well as cogni-tive restructuring for the treatment of social
phobia. Although both groups improved on most measures, patients receiving CBGT
were significantly more improved immediately after treat-ment and at 3- and
6-month follow-up. CBGT was more effective despite that patient ratings of
treatment credibility and expecta-tions for improvement were equal for both
treatments. Patients receiving CBGT continued to be more improved at 5-year
follow-up, although only 41% of the original sample participated in the
follow-up study, which limited the validity of these findings.
Four treatments for social phobia have been compared: 1) CBGT, 2)
phenelzine, 3) supportive psychotherapy, and 4) pla-cebo. Overall, both
phenelzine and CBGT were equally effective after 12 weeks of treatment and were
significantly more effective than placebo or supportive psychotherapy.
Phenelzine tended to work more quickly than CBGT and appeared to be more
effec-tive on a few measures. However, preliminary analyses of long-term outcome
showed that after discontinuing treatment, patients receiving CBGT were more
likely than patients who received phenelzine to maintain their gains, with
approximately half of patients taking phenelzine relapsing, compared with none
of the patients who responded to CBGT.
In a randomized clinical trial comparing cognitive therapy to
moclobemide for social phobia, Oosterbaan and colleagues (2001) found that
cognitive therapy was significantly better than moclobemide, but not placebo,
after 15 weeks of active treatment. After a 2-month follow-up period, cognitive
therapy was signifi-cantly better than both moclobemide and placebo. In
addition, treatment gains in the cognitive therapy group were maintained over a
15-month follow-up period.
Exposure therapy alone or in combination with sertraline for generalized
social phobia in a primary care setting has been studied. Family physicians
(FPs) were trained for 30 hours in assessment of social phobia and in the
application of exposure therapy. FPs reported satisfaction with the training
program and found that the exposure treatment was also useful for treating
pa-tients with other conditions. Although exposure therapy and ser-traline were
effective alone, the combination of exposure therapy and sertraline appeared to
confer added benefit.
According to cognitive models of social phobia, one of the mechanisms by
which CBT works is by causing a positive shift in an individual’s
self-representation (e.g., decreased negative self-focused thoughts and
increased task-focused thoughts and positive self-focused thoughts). Indeed,
there is evidence that fol-lowing CBT, individuals report significantly fewer
negative self-focused thoughts. Similarly, cognitive biases are reduced
follow-ing successful pharmacotherapy treatment as well and are related to the
degree of symptomatic improvement in both psychological and pharmacological
treatments.
In summary, it seems clear that effective psychosocial treatments and
medications for social phobia exist. Although both types of treatments appear
to be equally effective, each has advantages and disadvantages. Medication
treatments may work more quickly and are less time-consuming for the patient
and therapist. In contrast, improvement after CBT appears to last longer. Due
to medication side effects, CBT may be more appropriate for some individuals.
More studies are needed to examine the efficacy of combined medication and
psychoso-cial treatments for social phobia. A meta-analysis of 24 stud-ies
examining cognitive–behavioral and medication treatments for social phobia
found that both treatments were more effec-tive than control conditions (Gould et al., 1997). In this study, the SSRIs
and benzodiazepines tended to have the largest effect sizes among medications
and treatments involving exposure ei-ther alone or with cognitive therapy had
the largest effect sizes among CBT. Another meta-analytic study of 108
psychological and pharmacological treatment-outcome trials found that the
pharmacotherapies (SSRIs, benzodiazepines, MAO inhibitors) were the most
consistently effective treatments, with both SS-RIs and benzodiazepine
treatments equally effective and more effective than control groups (Fedoroff
and Taylor, 2001). Fur-ther, maintenance of treatment gains for CBT was
moderate and continued during follow-up intervals. In comparison, it is not
known the extent to which treatment gains for medication treatments are
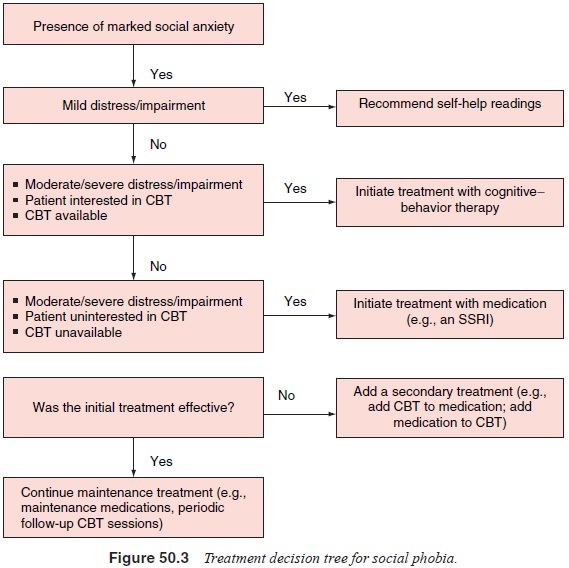
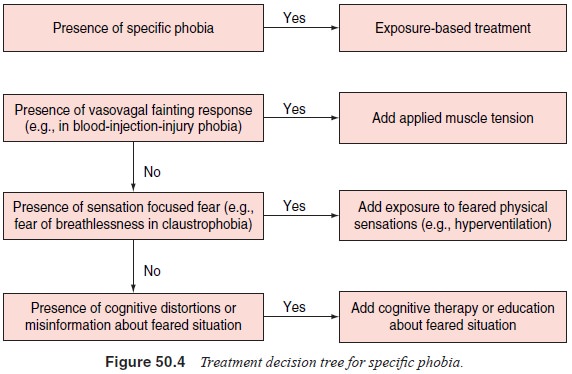
maintained following discontinuation. Treatment decision trees for social and
specific phobias are presented in Figures 50.3 and 50.4.
Related Topics