Chapter: Basic & Clinical Pharmacology : Agents Used in Dyslipidemia
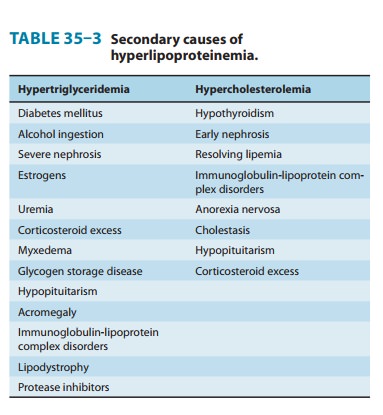
Secondary Hyperlipoproteinemia
SECONDARY HYPERLIPOPROTEINEMIA
Before primary
disorders can be diagnosed, secondary causes of the phenotype must be
considered. The more common conditions are summarized in Table 35–3. The
lipoprotein abnormality usu-ally resolves if the underlying disorder can be
treated successfully.
DIETARY MANAGEMENT OF HYPERLIPOPROTEINEMIA
Dietary
measures are initiated first—unless the patient has evident coronary or
peripheral vascular disease—and may obviate the need for drugs. Patients with
familial hypercholesterolemia or familial combined hyperlipidemia always
require drug therapy. Cholesterol and saturated and trans-fats are the principal factors that increase LDL, whereas
total fat, alcohol, and excess calories increase triglycerides.
Sucrose
and fructose raise VLDL. Alcohol can cause significant hypertriglyceridemia by
increasing hepatic secretion of VLDL. Synthesis and secretion of VLDL are
increased by excess calories. During weight loss, LDL and VLDL levels may be
much lower than can be maintained during neutral caloric balance. The
con-clusion that diet suffices for management can be made only after weight has
stabilized for at least 1 month.
General
recommendations include limiting total calories from fat to 20–25% of daily
intake, saturated fats to less than 8%, and cholesterol to less than 200 mg/d.
Reductions in serum cholesterol range from 10% to 20% on this regimen. Use of
complex carbo-hydrates and fiber is recommended, and cis-monounsaturated fats should predominate. Weight reduction,
caloric restriction, and avoidance of alcohol are especially important for
patients with elevated VLDL and IDL.
The
effect of dietary fats on hypertriglyceridemia is dependent on the disposition
of double bonds in the fatty acids. Omega-3 fatty acids found in fish oils, but
not those from plant sources, activate peroxisome proliferator-activated
receptor-alpha (PPAR-α) and can induce profound reduction
of triglycerides in some patients. They also have anti-inflammatory and
antiarrhythmic activities. Omega-3 fatty acids are available over the counter
as triglycerides from marine sources or as a prescription medication (Lovaza)
containing ethyl esters of omega-3 fatty acids. The rec-ommended dose of Lovaza
is 4 g/d. It is necessary to determine the content of docosahexaenoic acid and
eicosapentaenoic acid in over-the-counter preparations. Appropriate amounts
should be taken to provide up to 3–4 g of these fatty acids daily. It is
impor-tant to select preparations free of mercury and other contami-nants. The
omega-6 fatty acids present in vegetable oils may cause triglycerides to
increase.
Patients
with primary chylomicronemia and some with mixed lipemia must consume a diet
severely restricted in total fat (10–20 g/d, of which 5 g should be vegetable
oils rich in essen-tial fatty acids), and fat-soluble vitamins should be given.
Homocysteine,
which initiates proatherogenic changes in endothelium, can be reduced in many
patients by restriction of total protein intake to the amount required for
amino acid replacement. Supplementation with folic acid plus other B vita-mins
is indicated in severe homocysteinemia.
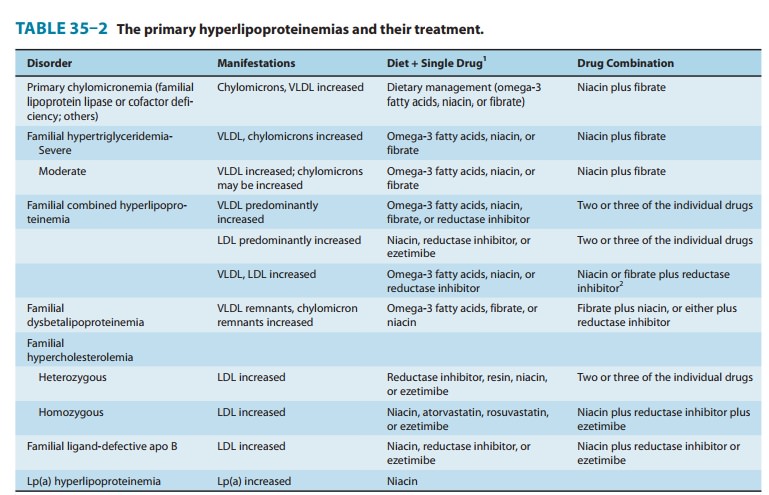
BASIC & CLINICAL PHARMACOLOGY OF DRUGS USED IN HYPERLIPIDEMIA
The decision to use
drug therapy for hyperlipidemia is based on the specific metabolic defect and
its potential for causing athero-sclerosis or pancreatitis. Suggested regimens
for the principal lipoprotein disorders are presented in Table 35–2. Diet
should be continued to achieve the full potential of the drug regimen. These
drugs should be avoided in pregnant and lactating women and those likely to
become pregnant. All drugs that alter plasma lipo-protein concentrations may
require adjustment of doses of warfa-rin and indandione anticoagulants.
Children with heterozygous familial hypercholesterolemia may be treated with a
resin or reductase inhibitor, usually after 7 or 8 years of age, when
myeli-nation of the central nervous system is essentially complete. The
decision to treat a child should be based on the level of LDL, other risk
factors, the family history, and the child’s age. Drugs are rarely indicated
before age 16 in the absence of multiple risk factors or compound genetic
dyslipidemias.
Related Topics