Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Rheumatic Disorders
Rheumatoid Arthritis - Diffuse Connective Tissue Diseases
RHEUMATOID ARTHRITIS
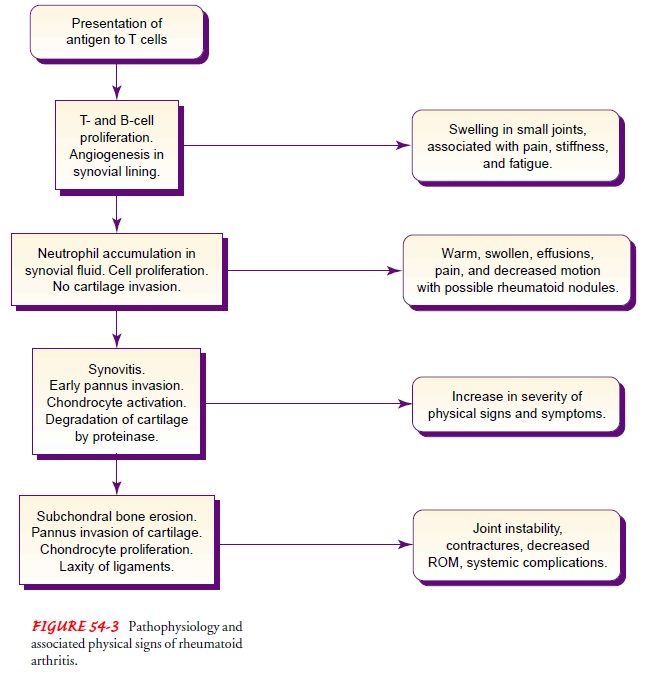
Pathophysiology
RA
is commonly used as the prototype for inflammatory arthritis. The incidence
rate is approximately 3%, with a two to three times greater incidence in women
(Ruddy et al., 2001). In RA, the autoimmune reaction (Fig. 54-3) primarily
occurs in the synovial tissue. Phagocytosis produces enzymes within the joint.
The en-zymes break down collagen, causing edema, proliferation of the synovial membrane,
and ultimately pannus formation. Pannus destroys cartilage and erodes the bone.
The consequence is loss of articular surfaces and joint motion. Muscle fibers
undergo de-generative changes. Tendon and ligament elasticity and contrac-tile
power are lost.
Clinical Manifestations
Clinical manifestations of RA vary, usually
reflecting the stage and severity of the disease. Joint pain, swelling, warmth,
ery-thema, and lack of function are classic. Palpation of the joints re-veals
spongy or boggy tissue. Often fluid can be aspirated from the inflamed joint.
Characteristically, the pattern of joint in-volvement begins with the small
joints in the hands, wrists, and feet. As the disease progresses, the knees,
shoulders, hips, elbows, ankles, cervical spine, and temporomandibular joints
are in-volved. The onset of symptoms is usually acute. Symptoms are usually
bilateral and symmetric. In addition to joint pain and swelling, another
classic sign of RA is joint stiffness, especially in the morning, lasting for more
than 30 minutes (Klippel, 2001).
In the early stages of disease, even before bony
changes occur, limitation in function can occur when there is active
inflamma-tion in the joints. Joints that are hot, swollen, and painful are not
easily moved. The patient tends to guard or protect these joints through
immobilization. Immobilization for extended periods can lead to contractures,
creating soft tissue deformity.
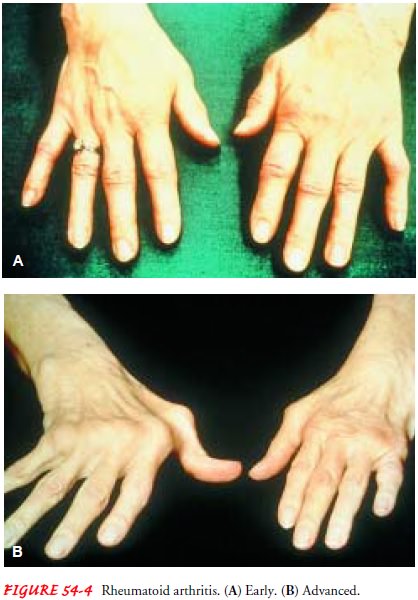
Deformities of the hands and feet are common in RA
(Fig. 54-4). The deformity may be caused by misalignment re-sulting from
swelling, progressive joint destruction, or the sub-luxation (partial
dislocation) that occurs when a bone slips over another and eliminates the
joint space.
RA is a systemic disease with multiple extra-articular features. Most common are fever, weight loss, fatigue, anemia, lymph node enlargement, and Raynaud’s phenomenon (cold- and stress-induced vasospasm causing episodes of digital blanching or cyanosis).
Rheumatoid
nodules may be noted in patients with more advanced RA and develop at some time
in up to half of pa-tients (Klippel, 2001). These nodules are usually nontender
and movable in the subcutaneous tissue. They usually appear over bony prominences
such as the elbow, are varied in size, and can disappear spontaneously. Nodules
occur only in individuals who have rheumatoid factor. The nodules often are
associated with rapidly progressive and destructive disease. Other
extra-articular features include arteritis, neuropathy, scleritis,
pericarditis, spleno-megaly, and Sjögren’s syndrome (dry eyes and dry mucous
membranes).
Assessment and Diagnostic Findings
Several factors can contribute to a diagnosis of
RA: rheumatoid nodules, joint inflammation detected on palpation, and certain
laboratory findings. The history and physical examination ad-dress
manifestations such as bilateral and symmetric stiffness, ten-derness,
swelling, and temperature changes in the joints. The patient is also assessed
for extra-articular changes; these often in-clude weight loss, sensory changes,
lymph node enlargement, and fatigue. Rheumatoid factor is present in more than
80% of pa-tients with RA, but its presence alone is not diagnostic of RA. The
erythrocyte sedimentation rate (ESR) is significantly elevated with RA. The red
blood cell count and C4 complement compo-nent are decreased. C-reactive protein
and antinuclear antibody test results may also be positive. Arthrocentesis
shows synovial fluid that is cloudy, milky, or dark yellow and contains
numerous inflammatory components, such as leukocytes and complement.
X-ray
studies, performed to help diagnose and monitor the progression of disease,
show characteristic bony erosions and nar-rowed joint spaces occurring later in
the disease.
Medical Management
EARLY-STAGE RA
In
patients with early RA, treatment begins with education, a bal-ance of rest and
exercise, and referral to community agencies for support. Medical management
begins with therapeutic doses of salicylates or NSAIDs. When used in full
therapeutic dosages, these medications provide both anti-inflammatory and
analgesic effects. Taking medications as prescribed to maintain a consistent
blood level is necessary to optimize the effectiveness of the anti-inflammatory
medication.
Several COX-2 inhibitors, another class of NSAIDs,
have been approved for treatment of RA. COX (cyclo-oxygenase) is an enzyme
involved in the inflammatory process. COX-2 inhibitors block the enzyme
involved in inflammation while leaving intact the enzyme involved in protecting
the stomach lining. As a result, COX-2 inhibitors are less likely to cause
gastric irritation and ulceration than other NSAIDs (Bombardier et al., 2000).
The trend in management is toward a more aggressive
pharma-cologic approach earlier in the disease. A window of opportunity for
symptom control and improved disease management occurs within the first 2 years
of disease onset. Therefore, the disease-modifying antirheumatic agents
(antimalarials, gold, penicillamine, or sulfasalazine) are initiated early in
treatment. If symptoms ap-pear to be aggressive (ie, early bony erosions as
seen on x-rays), methotrexate may be considered. Methotrexate is currently the
gold standard in the treatment of RA because of its success in im-proving
disease parameters (ie, pain, tender and swollen joints, quality of life). The
goals are to control symptoms and prevent destruction of the joints (Koopman,
2001).
An alternative treatment approach for RA has
emerged in the area of biologic therapies. Biologic response modifiers are a
group of agents that consist of molecules produced by cells of the im-mune
system or by cells that participate in the inflammatory re-actions (Koopman,
2001). Recent studies (Moreland et al., 1999; Weinblatt et al., 1999) using
tumor necrosis factor-alpha in-hibitors, both alone and in combination with
other medications, have shown that patients demonstrate significant improvement
based on American College of Rheumatology criteria (Felson et al., 1995). Two
examples of biologic response modifiers that are cur-rently available are
enatercept (Enbrel) and infliximab (Remicade). These agents inhibit the
function of tumor necrosis factor-alpha, a key cytokine known to play a role in the disease process in RA (Miller,
2001). Research in this area is ongoing.
Additional
analgesia may be prescribed for periods of extreme pain. Opioid analgesics are
avoided because of the potential for continuing need for pain relief.
Nonpharmacologic pain man-agement techniques (eg, relaxation techniques, heat
and cold applications) are taught.
MODERATE, EROSIVE RA
For
moderate, erosive RA, a formal program with occupational and physical therapy
is prescribed to educate the patient about principles of joint protection,
pacing activities, work simplifica-tion, range of motion, and
muscle-strengthening exercises. The patient is encouraged to participate
actively in the management program. The medication program is reevaluated
periodically, and appropriate changes are made if indicated. Cyclosporine,an
immunomodulator, may be added to enhance the disease-modifying effect of
methotrexate.
PERSISTENT, EROSIVE RA
For persistent, erosive RA, reconstructive surgery
and cortico-steroids are often used. Reconstructive surgery is indicated when
pain cannot be relieved by conservative measures. Surgical pro-cedures include
synovectomy (excision of the synovial membrane), tenorrhaphy (suturing a
tendon), arthrodesis (surgical fusion of the joint), and arthroplasty (surgical repair and replacement of the joint).
Surgery is not performed during disease flares.
Systemic corticosteroids are used when the patient
has un-remitting inflammation and pain or needs a “bridging” medication while
waiting for the slower disease-modifying antirheumatic agent (eg, methotrexate)
to begin working. Low-dose cortico-steroid therapy is prescribed for the
shortest time necessary to minimize side effects. Joints that are severely
inflamed and fail to respond promptly to the measures outlined previously may
be treated by local injection of a corticosteroid (Ruddy et al., 2001).
ADVANCED, UNREMITTING RA
For
advanced, unremitting RA, immunosuppressive agents are prescribed because of
their ability to affect the production of anti-bodies at the cellular level.
These include high-dose methotrexate (Rheumatrex), cyclophosphamide (Cytoxan),
and azathioprine (Imuran). These medications, however, are highly toxic and can
produce bone marrow suppression, anemia, gastrointestinal dis-turbances, and
rashes.
Through
all stages of RA, depression and sleep deprivation may require the short-term
use of low-dose antidepressant med-ications, such as amitriptyline (Elavil),
paroxetine (Paxil), or ser-traline (Zoloft), to reestablish an adequate sleep
pattern and to manage chronic pain better.
The FDA has approved a medical device for use in
treating pa-tients with more severe and longstanding cases of RA who have
failed to respond to or are intolerant of disease-modifying anti-rheumatic
drugs. The device, a protein A Immunoadsorption column (Prosorba), is used in
12 weekly 2-hour apheresis treat-ments to bind IgG (ie, circulating immune
complex). In this unique population of patients, a significant improvement
using the American College of Rheumatology Criteria for Improvement has been
demonstrated in several studies using the Prosorba column (Felson et al., 1999;
Gendreau, 2001).
Nutrition Therapy
Patients with RA frequently experience anorexia,
weight loss, and anemia. A dietary history identifies usual eating habits and
food preferences. Food selection should include the daily requirements from the
basic food groups, with emphasis on foods high in vit-amins, protein, and iron
for tissue building and repair. For the extremely anorexic patient, small,
frequent feedings with in-creased protein supplements may be prescribed. Some
medica-tions (ie, oral corticosteroids) used in RA treatment stimulate the
appetite and, when combined with decreased activity, may lead to weight gain.
Therefore, patients may need to be counseled about eating a healthy, calorie-restricted
diet.
Nursing Management
Nursing care of the patient with RA follows the
basic plan of care presented earlier. The most common issues for the patient
with RA include pain, sleep disturbance, fatigue, altered mood, and limited
mobility. The patient with newly diag-nosed RA needs information about the
disease to make daily self-management decisions and to cope with having a
chronic disease.
Because
of repeated contact with the patient, the nurse has the opportunity to assess
and intervene in patient concerns and issues that occur with the diagnosis of a
chronic illness such as RA. Because the disease commonly affects young women,
major con-cerns may be related to the effects of the disease on childbearing
potential, caring for family, or work responsibilities. The patient with a
chronic illness may seek a “cure” or have questions about alternative
therapies. Frequently, however, patients are hesitant to share their concerns
with health care professionals (American College of Rheumatology, 1998).
Related Topics