Chapter: Medical Physiology: Regulation of Acid-Base Balance
Regulation of Renal Tubular Hydrogen Ion Secretion
Regulation of Renal Tubular Hydrogen Ion Secretion
As discussed earlier, H+ secretion by the tubular epithelium is necessary for both HCO3– reabsorption and generation of new HCO3– associated with titrat-able acid formation. Therefore, the rate of H+ secre-tion must be carefully regulated if the kidneys are to effectively perform their functions in acid-base home-ostasis. Under normal conditions, the kidney tubules must secrete at least enough H+ to reabsorb almost all the HCO3– that is filtered, and there must be enough H+ left over to be excreted as titratable acid or NH4+ to rid the body of the nonvolatile acids produced each day from metabolism.
In alkalosis, tubular secretion of H+ must be reduced to a level that is too low to achieve complete HCO3– reabsorption, enabling the kidneys to increase HCO3– excretion. In this condition, titratable acid and ammonia are not excreted because there is no excess H+available to combine with nonbicarbonate buffers; therefore, there is no new HCO3– added to the urine in alkalosis. During acidosis, the tubular H+ secretion must be increased sufficiently to reabsorb all the filtered HCO3– and still have enough H+ left over to excrete large amounts of NH4+ and titratable acid, thereby contributing large amounts of new HCO3– to the total body extracellular fluid. Themost important stimuli for increasing H+ secretion by the tubules in acidosis are (1) an increase in PCO2 of the extracellular fluid and (2) an increase in H+ concentration of the extracellular fluid (decreased pH).
The tubular cells respond directly to an increase in PCO2 of the blood, as occurs in respiratory acidosis, with an increase in the rate of H+ secretion as follows: The increased PCO2 raises the PCO2 of the tubular cells, causing increased formation of H+ in the tubular cells, which in turn stimulates the secretion of H+. The second factor that stimulates H+ secretion is an increase in extracellular fluid H+ concentration (decreased pH).
A special factor that can increase H+ secretion under some pathophysiologic conditions is excessive aldos-terone secretion. Aldosterone stimulates the secretion of H+ by the intercalated cells of the collecting duct. Therefore, oversecretion of aldosterone, as occurs in Conn’s syndrome, can cause excessive secretion of H+ into the tubular fluid and, consequently, increased amounts of bicarbonate added back to the blood. This usually causes alkalosis in patients with excessive aldosterone secretion.
The tubular cells usually respond to a decrease in H+ concentration (alkalosis) by reducing H+ secretion. The decreased H+ secretion results from decreased extracellular PCO2, as occurs in respiratory alkalosis, or from a decrease in H+ concentration per se, as occurs in both respiratory and metabolic alkalosis.
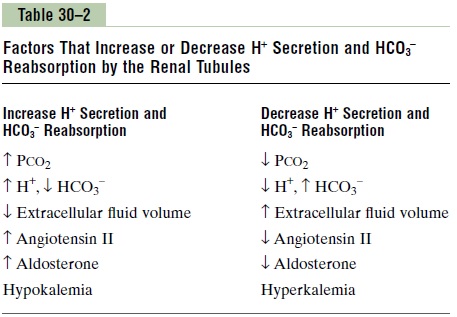
Table 30–2 summarizes the major factors that influ-ence H+ secretion and HCO3– reabsorption. Some of these are not directly related to the regulation of acid-base balance. For example, H+ secretion is coupled to Na+ reabsorption by the Na+-H+ exchanger in the proximal tubule and thick ascending loop of Henle. Therefore, factors that stimulate Na+ reabsorption, such as decreased extracellular fluid volume, may also secondarily increase H+ secretion.
Extracellular fluid volume depletion stimulates sodium reabsorption by the renal tubules and increases H+ secretion and HCO3–reabsorption through multiple mechanisms, including (1) increased angiotensin II levels, which directly stimulate the activ-ity of the Na+-H+ exchanger in the renal tubules, and (2) increased aldosterone levels, which stimulate H+ secretion by the intercalated cells of the cortical col-lecting tubules. Therefore, extracellular fluid volume depletion tends to cause alkalosis due to excess H+ secretion and HCO3– reabsorption.
Changes in plasma potassium concentration can also influence H+ secretion, with hypokalemia stimu-lating and hyperkalemia inhibiting H+ secretion in the proximal tubule. A decreased plasma potassium con-centration tends to increase the H+ concentration in the renal tubular cells. This, in turn, stimulates H+ secretion and HCO3– reabsorption and leads to alka-losis. Hyperkalemia decreases H+ secretion and HCO3– reabsorption and tends to cause acidosis.
Related Topics