Chapter: Essentials of Anatomy and Physiology: Heart
Regulation of Heart Function
REGULATION OF HEART FUNCTION
Various measurements can be taken to assess the heart’s function. Cardiac output (CO) is the volume of blood pumped by eitherventricle of the heart each minute. Stroke volume (SV) is the vol-ume of blood pumped per ventricle each time the heart contracts, and the heart rate (HR) is the number of times the heart contracts each minute. Cardiac output can be calculated by multiplying the stroke volume times the heart rate:
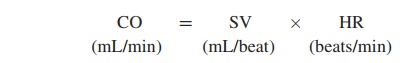
Under resting conditions, the heart rate is approximately 72 beats/min, and the stroke volume is approximately 70 mL/beat. Consequently, the cardiac output is slightly more than 5 L/min:
CO = SV × HR
= 70 mL/beat × 72 bpm
= 5040 mL/min (approximately 5 L/min)
The heart rate and the stroke volume vary considerably among people. Athletes tend to have a higher stroke volume and lower heart rate at rest because exercise has increased the size of their hearts. Nonathletes are more likely to have a higher heart rate and lower stroke volume. During exercise, the heart rate in a nonathlete can increase to 190 bpm, and the stroke volume can increase to 115 mL/beat. Therefore, the cardiac output increases to approximately 22 L/min:
CO = SV × HR
=115 mL/beat × 190 bpm
=21,850 mL/min (approximately 22 L/min
This cardiac output is several times greater than the cardiac output under resting conditions. Athletes can increase their cardiac output to a greater degree than nonathletes. The control mecha-nisms that modify the stroke volume and the heart rate are classi-fied as intrinsic and extrinsic.
Intrinsic Regulation Of The Heart
Intrinsic regulation refers to mechanisms contained within theheart itself. The force of contraction produced by cardiac muscle is related to the degree of stretch of cardiac muscle fibers. The amount of blood in the ventricles at the end of ventricular diastole determines the degree to which cardiac muscle fibers are stretched. Venous return is the amount of blood that returns to the heart, andthe degree to which the ventricular walls are stretched at the end of diastole is called preload. If venous return increases, the heart fills to a greater volume and stretches the cardiac muscle fibers, produc-ing an increased preload. In response, cardiac muscle fibers contract with a greater force. The greater force of contraction causes an increased volume of blood to be ejected from the heart, resulting in an increased stroke volume. As venous return increases, resulting in an increased preload, cardiac output increases. Conversely, if venous return decreases, resulting in a decreased preload, the cardiac output decreases. The relationship between preload and stroke volume is called Starling’s law of the heart.
Because venous return is influenced by many conditions, Starling’s law of the heart has a major influence on cardiac output. For example, muscular activity during exercise causes increased venous return, resulting in increased preload, stroke volume, and cardiac output. This is beneficial because increased cardiac output is needed during exercise to supply O2 to exercising skeletal muscles.
Afterload refers to the pressure against which the ventriclesmust pump blood. People suffering from hypertension have an increased afterload because their aortic pressure is elevated dur-ing contraction of the ventricles. The heart must do more work to pump blood from the left ventricle into the aorta, which increases the workload on the heart and can eventually lead to heart failure. A reduced afterload decreases the work the heart must do. People who have lower blood pressure have a reduced afterload and develop heart failure less often than people who have hypertension. However, the afterload influences cardiac output less than preload influences it. The afterload must increase substantially before it decreases the volume of blood pumped by a healthy heart.
Extrinsic Regulation Of The Heart
Extrinsic regulation refers to mechanisms external to the heart,such as either nervous or chemical regulation.
Nervous Regulation: Baroreceptor Reflex
Nervous influences of heart activity are carried through the auto-nomic nervous system. Both sympathetic and parasympathetic nerve fibers innervate the heart and have a major effect on the SA node. Stimulation by sympathetic nerve fibers causes the heart rate and the stroke volume to increase, whereas stimulation by parasympathetic nerve fibers causes the heart rate to decrease.
The baroreceptor (bar′ ̄o -r̄e -sep′ ter; baro, pressure) reflex is a mechanism of the nervous system that plays an important role in regulating heart function. Baroreceptors are stretch receptors that monitor blood pressure in the aorta and in the wall of the internal carotid arteries, which carry blood to the brain. Changes in blood pressure result in changes in the stretch of the walls of these blood vessels—and changes in the frequency of action potentials produced by the baroreceptors. The action potentials are transmitted along nerve fibers from the stretch receptors to the medulla oblongata of the brain.
Within the medulla oblongata is a cardioregulatory center, which receives and integrates action potentials from the barore-ceptors. The cardioregulatory center controls the action potential frequency in sympathetic and parasympathetic nerve fibers that extend from the brain and spinal cord to the heart. The cardio-regulatory center also influences sympathetic stimulation of the adrenal gland. Epinephrine and norepinephrine, released from the adrenal gland, increase the stroke volume and heart rate.
Figure 12.20 shows how the baroreceptor reflex keeps the heart rate and stroke volume within normal ranges. When the blood pressure increases, the baroreceptors are stimulated. Action poten-tials are sent along the nerve fibers to the medulla oblongata at increased frequency. This prompts the cardioregulatory center to increase parasympathetic stimulation and decrease sympathetic stimulation of the heart. As a result, the heart rate and stroke vol-ume decrease, causing blood pressure to decline.
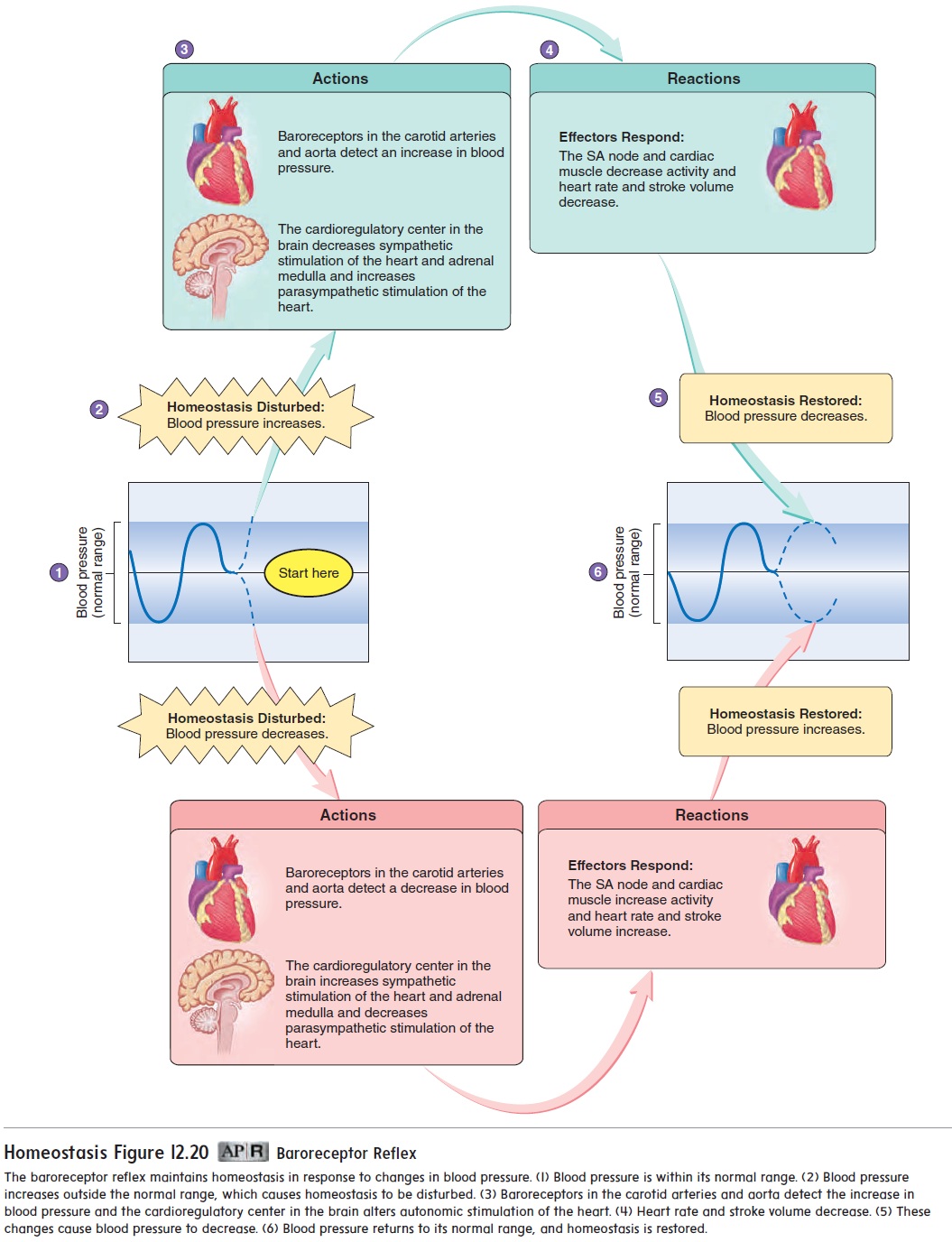
When the blood pressure decreases, less stimulation of the baroreceptors occurs. A lower frequency of action potentials is sent to the medulla oblongata of the brain, and this triggers a response in the cardioregulatory center. The cardioregulatory center responds by increasing sympathetic stimulation of the heart and decreasing parasympathetic stimulation. Consequently, the heart rate and stroke volume increase, causing blood pressure to increase. If the decrease in blood pressure is large, sympathetic stimulation of the adrenal medulla also increases. The epinephrine and norepinephrine secreted by the adrenal medulla increase the heart rate and stroke volume, also causing the blood pressure to increase toward its normal value (figure 12.20).
Chemical Regulation: Chemoreceptor Reflex
Epinephrine and small amounts of norepinephrine released from the adrenal medulla in response to exercise, emotional excitement, or stress also influence the heart’s function. Epinephrine and nor-epinephrine bind to receptor proteins on cardiac muscle and cause increased heart rate and stroke volume. Excitement, anxiety, or anger can affect the cardioregulatory center, resulting in increased sympathetic stimulation of the heart and increased cardiac output. Depression, on the other hand, can increase parasympathetic stim-ulation of the heart, causing a slight reduction in cardiac output.
The medulla oblongata of the brain also contains chemorecep-tors that are sensitive to changes in pH and CO2 levels. A decrease in pH, often caused by an increase in CO2, results in sympathetic stimulation of the heart (figure 12.21).
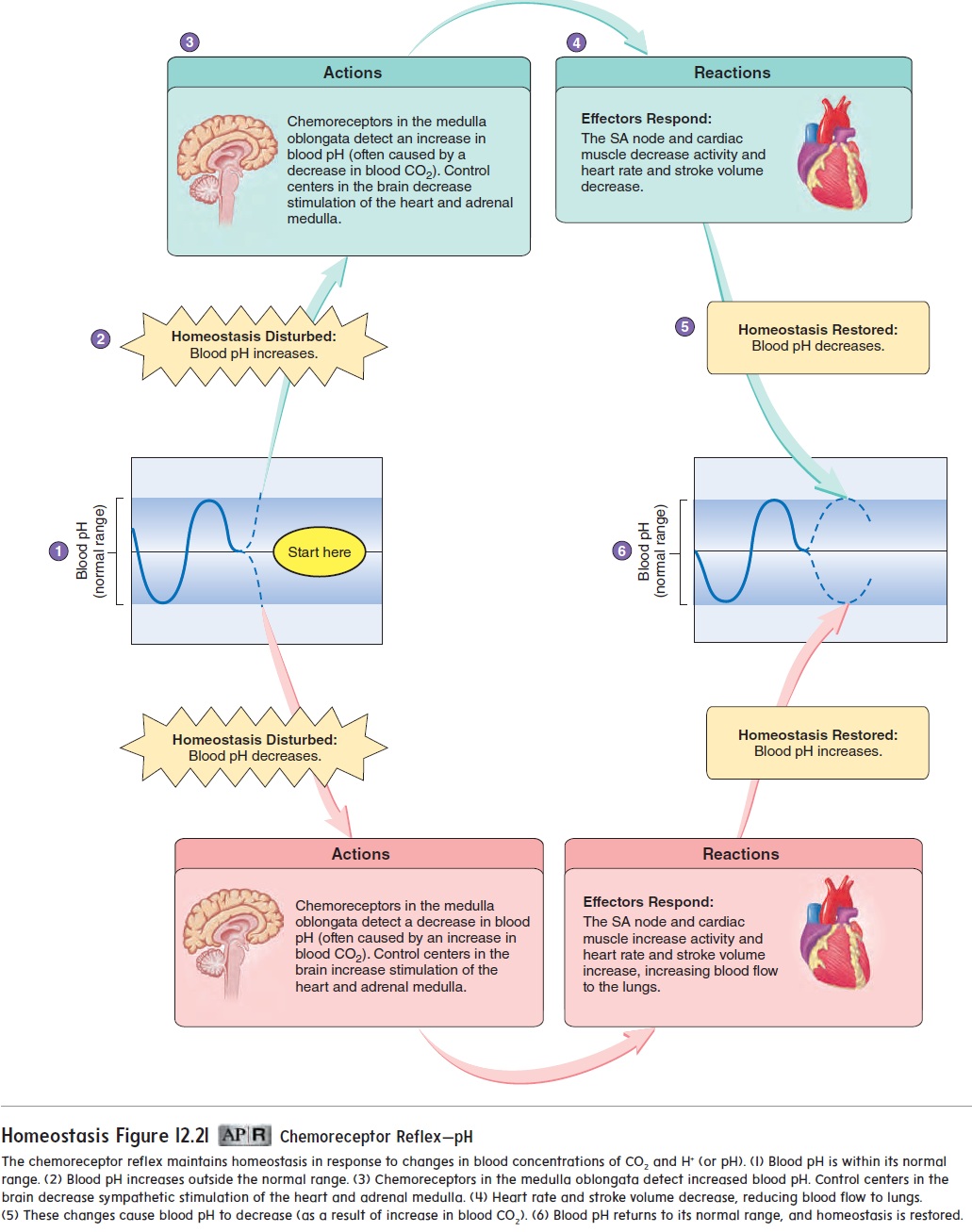
Changes in the extracellular concentration of K+, Ca2+, and Na+, which influence other electrically excitable tissues, also affect cardiac muscle function. An excess of extracellular K+ causes the heart rate and stroke volume to decrease. If the extra-cellular K+ concentration increases further, normal conduction of action potentials through cardiac muscle is blocked, and death can result. An excess of extracellular Ca2+ causes the heart to contract arrhythmically. Reduced extracellular Ca2+ cause both the heart rate and stroke volume to decrease.
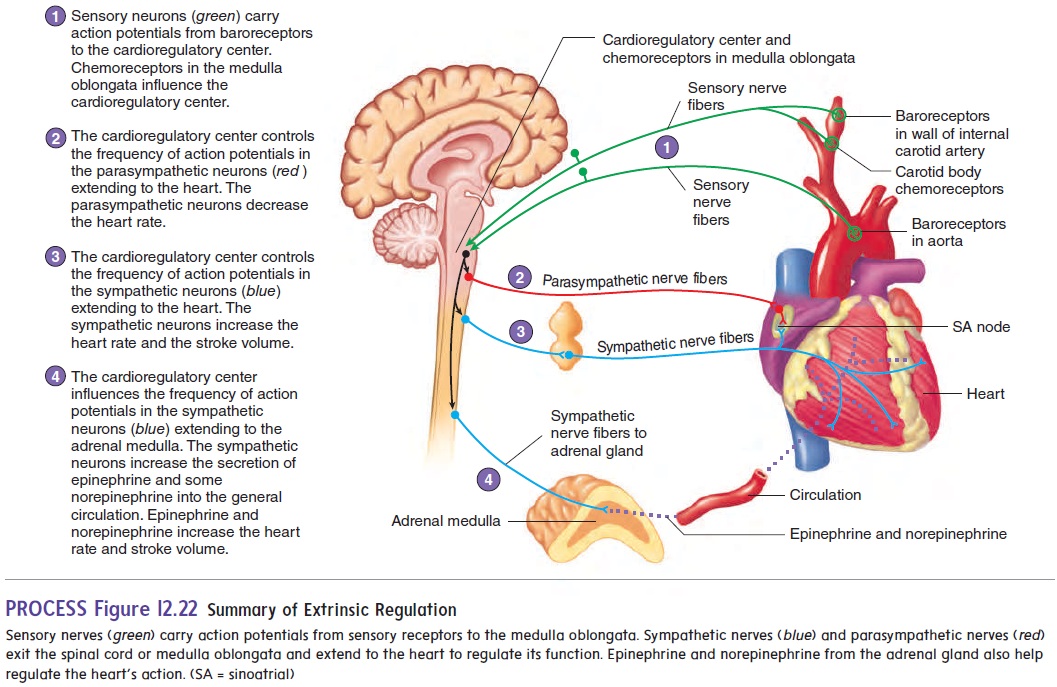
Figure 12.22 summarizes how nervous and chemical factors interact to regulate the heart rate and stroke volume.
Body temperature affects the metabolism in the heart just as it affects other tissues. Elevated body temperature increases the heart rate, and reduced body temperature slows the heart rate. Forexample, the heart rate is usually elevated when a person has a fever. During heart surgery, the body temperature is sometimes intentionally lowered to slow the heart rate and metabolism.
Related Topics