Chapter: Medicine Study Notes : Psychological Medicine
Psychiatric History
History
·
This will include the patient‟s
narrative, and is therefore subject to revision and embellishment according to
the state of mind of the individual and the relationship with the interviewer.
The patient may adjust the history according to the interviewer‟s hypothesis
and values. History taking is therefore collaborative and therapeutic. It is
helping to construct the illness story
·
Identifying Data
o Name, date of interview, age, sex, race, country of birth, occupation,
date of hospital admission, marital status
o Use as opportunity to put the patient at ease, build rapport
·
Reasons for and circumstances of referral/admission
o Who made the referral, why now, what expectations
·
List of presenting symptoms and their duration
o List each symptom and duration, use patient‟s own words
o Is the situation acute or chronic
o Suggested questions:
§ What sort of problems are troubling you/were troubling you when you came
to hospital?
§ What have been the main difficulties
·
History of Current Illness
o Need to know the patient‟s story: patient‟s situation and
preceding/precipitating events
o Narrative account of development of symptoms
o Include medication and compliance
o Suggested questions:
§ When did you last feel well?
§ What are the worst worries in your life?
·
Systematic enquiry
o Should screen for all these in every patient
o Anxiety Symptoms
§ See Topic: History Taking in Anxiety Disorders
o Mood Symptoms
§ Refers to long-term/sustained emotional state (ie over last week/months) and is subjective experience of the patient
§ Prevailing mood at the time: quality (eg depressed, sad, angry, irritable, happy, elated, suspicious, perplexed, anhedonia), intensity (ask about extremes), reactivity, duration (when was it last normal)
§ Persisting or fluctuating: if so what pattern
§ Aggravating or relieving factors
§ Associated symptoms
§ Patient‟s attribution of mood
o Psychotic symptoms
§ = Thought disorder, delusions or hallucinations
§ Thought disorder = abnormalities in the thinking process – evidenced by disorganised speech, thinking or behaviour
§ Delusions
·
= Fixed, false belief,
abnormal/bizarre beliefs held with conviction, are without evidence and are
culturally inconsistent
·
Fixedness is key, resisting
coercion to change, and preoccupying
· Ask about unusual concerns, preoccupations, thoughts that others find strange
§ Hallucinations = abnormal perceptual phenomena. Ask about visions,
sensations, noises that are unusual or not shared by other people
o Suicidibility or other dangerous behaviour: See Topic: Suicide Assessment and Management
o Cognitive functioning: See Topic Cognition
o Neurophysiological changes
§ Measure severity of primary process
§ Changed sleep, energy/motivation, concentration, appetite/weight (look
for a 5% change over several weeks), sex
§ Sleep: initial, middle, terminal phases, how much in total, is it
restful
o Alcohol or drug use
§ Present or past
§ Smoking, alcohol, illicit drugs, sleeping tablets/tranquillisers
o Stressors
o Medications and Compliance
o Impulse-Control Screen: Screen for gambling
(comorbidity of gambling with other pscyh
symptoms is common)
·
Past Psychiatric History
o Dates, duration, diagnoses, treatment, response to treatment and outcome
o Suggested questions:
§ Have you had any psychiatric treatment before?
§ Is the present illness like the previous one?
·
Medical History: Past serious illnesses,
disabilities, current illnesses and medication
·
Family History
o Parents and siblings: age, state of health (mental & physical),
occupations, situation, personalities, relationship to patient. May help to
draw up a family tree
o Get idea of family atmosphere during childhood: personalities of parents
and relationships have lasting influence on subsequent relationships. How much
care did you get from each parent? How controlling/protective were they?
o Ask about grandparents, and parents up brining
o Has anyone in the family been treated for nerves, had a breakdown, been
admitted to a psych hospital, committed or attempted suicide, had an A & D
problem?
o Categorise under:
§ Structure of family
§ Description of key people
§ Description of important relationships
§ Family roles
§ Family history of psychiatric illness or alcohol abuse
·
Personal and Social History
o Important events and influences in patient‟s life
o Start open ended: Tell me a bit about your childhood and background?
What are the important things you remember?
o Birth: difficulties, parents situation at time
o Childhood: family situation, illnesses, injury, nervous symptoms (eg enuresis/bedwetting, fears, phobias, how did they feel going to school, etc). Did you ever have any unpleasant experiences – did anyone ever harm you, hit you, interfere with you sexually?
o School: primary to tertiary. Academic, sporting, relationships with peers and teachers
o Employment: types of jobs, reason for leaving, work performance & satisfaction, relationships at work
o Sexual: age at puberty, sexual orientation, sexual experience (current and past), sexual satisfaction, contraception, sexual abuse, unpleasant or distressing sexual experiences. Introduce when talking about adolescence. Aim is to establish abnormalities or concerns about sexual functioning or relationships
o Marital: duration of courtship, age at marriage, age, occupation and health of spouse, marital relationship and problems
o Children: pregnancies, ages and names of children, health,
personalities, schooling, occupations, difficulties in relationship with parent
o Friendships: long-standing friends and confidences
o Current living situation
o Difficulties with law
o Leisure activities and interests
o Religion: upbringing, beliefs and practices, changes in religious belief
(important to ask, won‟t volunteer)
·
Premorbid personality
o Patient‟s opinions and interviewer‟s impressions of premorbid
personality
o Personality = enduring characteristics, so requires evaluation over time
·
Patient’s Attribution of Illness
o What the patient thinks is the cause of the illness
o Possibility include under „insight‟ in mental state exam
· Insert Mental State Exam write-up here
·
Formulation
o Core of the psychiatric assessment: why did this person become ill in
this way at this time?
o Opinion about what explains the presentation and what treatment may work
o Manner in which patient‟s problems are unique. Not a summary of problems but the crucial factors, based on a theoretical knowledge of the aetiology of psychiatric illness. The linkages/connections between different aspects should add something new – all the raw material should have been presented before
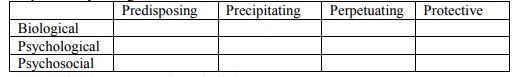
o Should cover the 4 Ps: Predisposing factors, precipitating factors,
perpetuating factors, protective factors
o Conceptualise by filling in this table:
o Suggest outline (one paragraph per bullet):
§ Describe problem
§ Why is this patient at risk of a psychiatric illness, using
bio-psycho-social framework
§ Describe triggers to presentation
§ Describe relevant prognostic factors, positive and negative
§ Balanced assessment of risks: especially of suicide and violent
behaviour
·
Diagnosis and Differential Diagnosis
o Manner in which patient‟s problems are similar to others (cf formulation
which emphasises uniqueness)
o Usually presented using DSM-IV or ICD-10.
o In differential diagnosis: concisely state evidence for and against each possible diagnosis in order of probability – only include evidence that discriminates between diagnoses
o Don‟t forget general medical conditions if there is sufficient evidence
·
Management Plan
o Safety: how will the risks identified be contained or minimised. Is the
patient consenting or committed?
o Medical: any medical conditions requiring attention
o Diagnosis: is it clear? If not, what needs to be done?
o Psychiatric Management: can be divided into management of target symptoms and management aimed at underlying disease. Can be considered under bio-psycho-social headings. Divide into timeframes – now, the next day or two, longer term
o Always mention family in plan: information and support for them, their
role in helping the patient, assistance with the significant stresses the
family may face, etc
·
Experience Interviewing the Patient:
difficulties interviewing the patient, reactions/emotions evoked by patient, how you dealt with these
Related Topics