Chapter: Ophthalmology: Glaucoma
Primary Angle Closure Glaucoma
Primary Angle Closure Glaucoma
Definition
Acute episodic increase in intraocular
pressure to several times the normal value (10 – 20 mm Hg) due to sudden
blockage of drainage. Production of aqueous humor and trabecular resistance are
normal.
Epidemiology:
The incidence among persons over the age of 60 is one
perthousand. Women are three times as likely to be affected as men. Inuit are
more frequently affected than other ethnic groups, whereas the disorder is rare
in blacks.
Etiology:
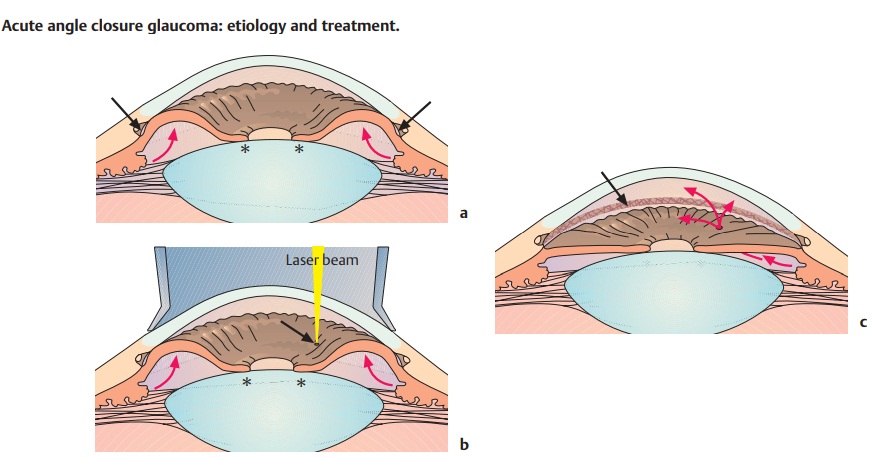
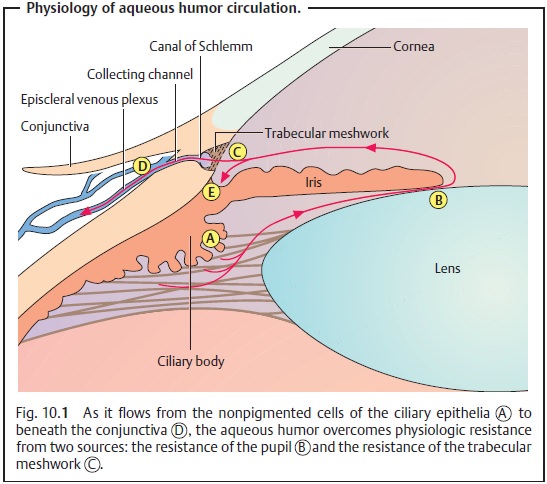
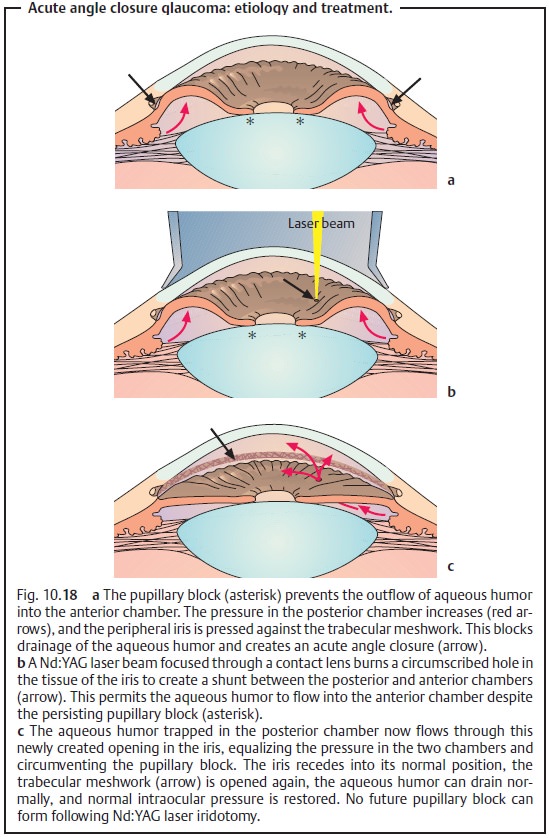
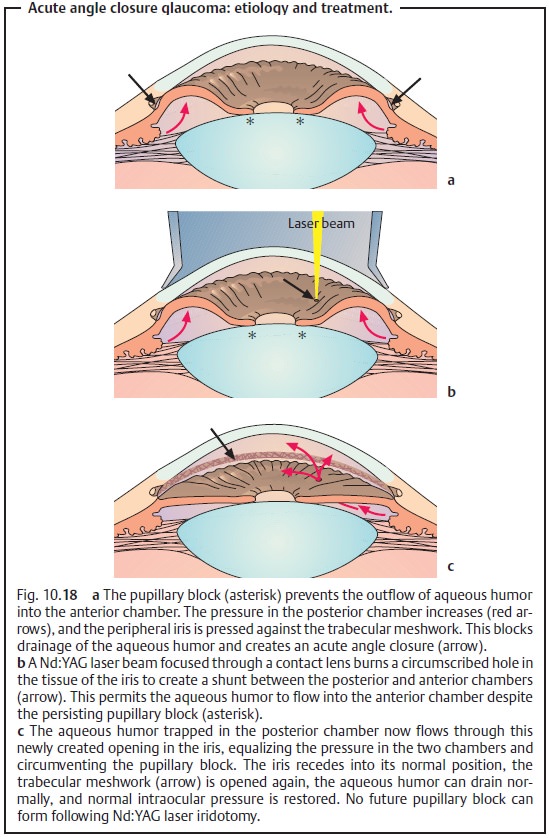
(See also physiology and pathophysiology of aqueous humor circu
Anatomically predisposed eyes with shallow anterior chambers (see Fig. 10.1) pose a relative impediment to the flow of aqueous humor
through the pupil. This pupillary block increases the pressure in the posterior cham-ber (Fig. 10.18a). The pressure displaces the iris anteriorly toward the
trabecular meshwork, suddenly blocking the outflow of aqueous humor (angle closure). A typical glaucoma attack occurs unilaterally due to widening
of the pupil either in dark surroundings and/or under emotional stress (dismay
or fear). A typical situation is the evening mystery movie on television.
Iatrogenic pharmacologic mydriasis and systemic psychotropic drugs can also
trigger a glaucoma attack.
Bear in mind that mydriatic agents entail a
risk of triggering a glaucoma attack by widening the pupil. Therefore, it is
important to evaluate the depth of the anterior chamber in every patient even
prior to a routine fundus examination.
Symptoms: Acute onset of intense pain. The elevated intraocular pressureacts on the
corneal nerves (the ophthalmic nerve or first branch of the trigeminal nerve)
to cause dull pain. This pain may be referred to the temples, back of the head,
and jaws via the three branches of the trigeminal nerve, which can mask its
ocular origin.
Nausea and vomiting occur due to irritation of the vagus nerve and can simu-late
abdominal disorders. The generalized symptoms such as headache, vomiting, and
nausea may dominate to the extent that the patient fails to notice local
symptoms.
Diminished visual acuity.Patients notice obscured vision and colored halosaround lights
in the affected eye. These symptoms are caused by the corneal epithelial edema
precipitated by the enormous increase in pressure.
Prodromal symptoms.Patients report transitory episodes of blurred
visionor the appearance of colored halos around lights prior to the attack.
These prodromal symptoms may go
unnoticed or may be dismissed as unimportant by the patient in mild episodes
where the eye returns to normal. Early identi-fication of those risk patients
with shallow anterior chambers and gonio-scopic findings is important as damage
to the structures of the angle may be well advanced before clinical symptoms appear.
The full clinical syndrome of acute glaucoma
will not always be present. The diminished visual acuity may go unnoticed if
the other eye has nor-mal vision. Patients’ subjective perception of pain
intensity can vary greatly.
Diagnostic considerations (Fig. 10.17):
The diagnosis is made on the basis of a triad
of symptoms:
❖Unilateral red eye with conjunctival or
ciliary injection.
❖ Fixed and dilated pupil.
❖Hard eyeball on palpation.
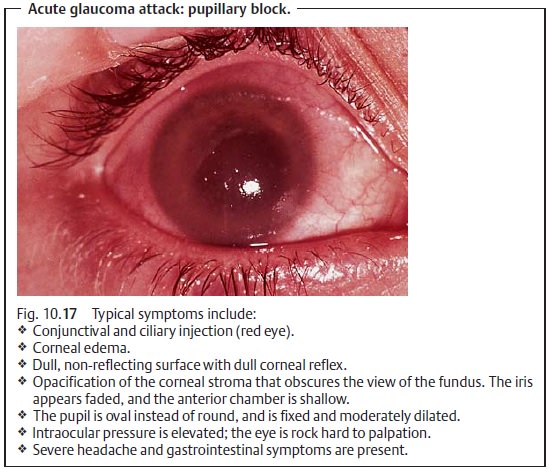
Other findings.
❖ The
cornea is dull and steamy with epithelial edema.
❖The anterior chamber is shallow or completely
collapsed. This will be apparent when the eye is illuminated by a focused
lateral light source (Fig. 1.12, p. 12) and upon slit-lamp examination. Inspection of the
shallow anterior chamber will be difficult. Details of the surface of the iris
will be visible, and the iris will appear faded.
❖The fundus is generally obscured due to
opacification of the corneal epithelium. When the fundus can be visualized as
symptoms subside and the cornea clears, the spectrum of changes to the optic
disk will range from a normal vital optic disk to an ill-defined hyperemic
optic nerve. In the lat-ter case, venous congestion will be present. The
central artery of the retina will be seen to pulse on the optic disk as blood
can only enter the eye during the systolic phase due to the high intraocular
pressure.
❖ Visual
acuity is reduced to perception of hand motions.
Differential diagnosis:
Misdiagnosis is possible as the wide variety of symp-toms can
simulate other disorders.
❖ General symptoms such as headache, vomiting, and nausea often predom-inate and
can easily be mistaken for appendicitis
or a brain tumor.
❖In iritis and iridocyclitis, the eye is also red and the iris appears faded.However,
intraocular pressure tends to be decreased rather than elevated.
Treatment:
An acute glaucoma attack is an emergency, and
the patient requires immediate treatment by an ophthalmologist. The underlying
causes of the disorder require surgical treatment, although initial therapy is
con-servative.
Medical therapy.Goals of conservative therapy:
❖ Decrease intraocular pressure.
❖ Allow the cornea to clear (important for
subsequent surgery).
❖ Relieve pain.
Time factor in reducing intraocular pressure:
Principles of medical therapy in primary angle closure glaucoma
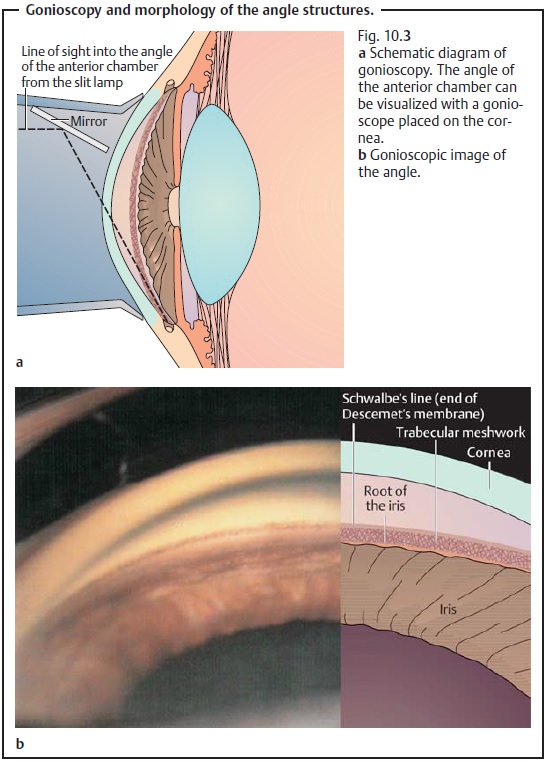
(see Fig. 10.3):
❖ Osmotic reduction in the volume of the
vitreous body is achieved via sys-temic hyperosmotic
solutions (oral glycerin, 1.0 – 1.5 g/kg of body weight, or intravenous
mannitol, 1.0 – 2.0 g/kg of body weight).
❖ Production of aqueous humor is decreased by inhibiting carbonic anhy-drase (intravenous
acetazolamide, 250 – 500 mg). Both steps are taken ini-tially to reduce
intraocular pressure to below 50 – 60 mm Hg.
❖The iris is withdrawn from the angle of the
anterior chamber by adminis-tering topical
miotic agents. Pilocarpine 1% eyedrops should be applied every 15 minutes.
If this is not effective, pilocarpine can be applied more often, every five
minutes, and in concentrations up to 4%. Miotic agents are not the medications
of first choice because the sphincter pupillae muscle is ischemic at pressures
exceeding 40 – 50 mm Hg and will not respond to miotic agents. Miotic agents
also relax the zonule fibers, which causes anterior displacement of the lens
that further compresses the anterior chamber. This makes it important to first
initiate therapy with hyper-osmotic agents to reduce the volume of the vitreous
body.
❖ Symptomatic therapy with analgesic agents, antiemetic agents, and seda-tives may be initiated where necessary.
Mechanical indentation of the cornea: Simple repetitive indentation of thecentral
cornea with a muscle hook or glass rod for approximately 15 – 30 sec-onds
presses the aqueous humor into the periphery of the angle of the ante-rior
chamber, which opens the angle. If this manipulation succeeds in keep-ing the
trabecular meshwork open for a few minutes, it will permit aqueous humor to
drain and reduce intraocular pressure. This improves the response to
pilocarpine and helps clear up the cornea.
Surgical management (shunt between the posterior and anterior
cham-bers).Once the cornea is
clear, theunderlying causes of the
disorder are treatedsurgically by creating a shunt between the posterior
and anterior chambers.
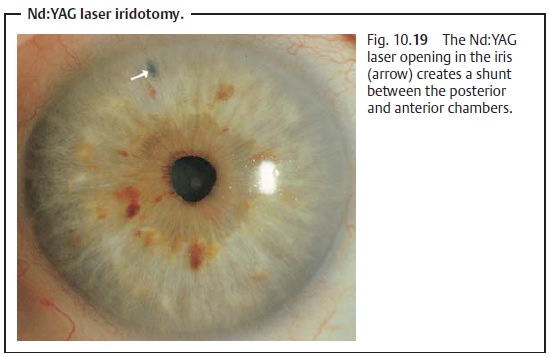
Neodymium:yttrium-aluminum-garnet laser iridotomy (nonincisional pro-cedure): The Nd:YAG laser can be used to create an opening in the peripheraliris (iridotomy) by tissue lysis without having to open the globe (Figs. 10.18a – c). The operation can be performed under topical anesthesia (Fig. 10.19).
Peripheral iridectomy (incisional procedure): Where the cornea is still swollenwith edema or
the iris is very thick, an open procedure may be required to create a shunt. A
limbal incision is made at 12 o’clock under topical anesthesia or general
anesthesia, through which a basal iridectomy is performed. Today peripheral
iridectomy is rarely performed, in only in 1 – 2% of all cases.
Prophylaxis:
When the patient reports clear prodromal symptoms and theangle of the anterior chamber appears constricted, the safest prophylaxis is to perform a Nd:YAG laser iridotomy or peripheral iridectomy. If one eye has already suffered an acute attack, the fellow eye should be treated initially every 4 – 6 hours with pilocarpine 1% to minimize the risk of a glaucoma attack. The second eye should then be treated with a Nd:YAG laser to prevent glaucoma once surgical stabilization of the first eye has been achieved.
Prognosis:
One can usually readily release a pupillary block and
lowerintraocular pressure in an initial attack with medication and permanently
prevent further attacks with surgery. However, recurrent acute angle closure
glaucoma or angle closure persisting longer than 48 hours can produce
peripheral synechia between the root of the iris and the trabecular meshwork
opposite it. These persisting cases of angle closure glaucoma cannot be cured
by Nd:YAG laser iridotomy or iridectomy, and the angle closure will persist
despite surgery. Filtration surgery is indicated in these cases.
Where intraocular pressure is controlled and
the cornea is clear, gonios-copy is indicated to demonstrate that the angle is
open again and to exclude persistent angle closure.
Related Topics