Chapter: Clinical Dermatology: Skin tumours
Premalignant tumours
Premalignant tumours
Keratoacanthoma
Some
argue that this rapidly growing tumour should be classed as benign, but a very
few transform into a squamous cell carcinoma.
Cause
Photosensitizing chemicals such as tar and mineral oils can act as cocarcinogens with ultraviolet radiation. They may also follow therapeutic immunosuppression.
Clinical features
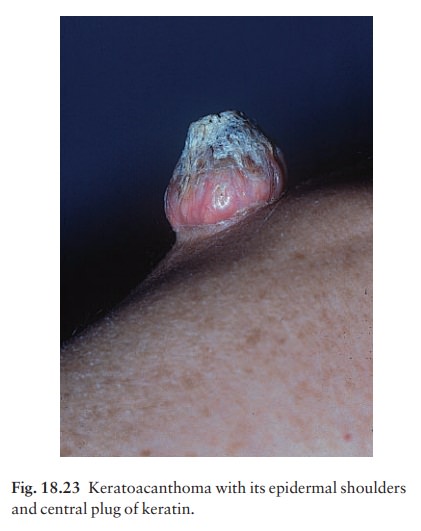
They
occur mainly on the exposed skin of fair indi-viduals. More than two-thirds are
on the face and most of the rest are on the arms. The lesion starts as a pink
papule that rapidly enlarges; it may reach a diameter of 1 cm in a month or
two. After 5 or 6 weeks the centre of the nodule forms either a keratinous plug
or a crater (Fig. 18.23). If left, the lesion often resolves spontaneously over
6ŌĆō12 months but leaves an ugly depressed scar.
Differential diagnosis
Squamous
cell carcinoma is the main tumour to be distinguished from a keratoacanthoma.
However, carcinomas grow more slowly and usually lack symmetry.
Histology
It is not possible to tell a keratoacanthoma from a squamous cell carcinoma histologically unless the architecture of the whole lesion can be assessed, including its base (Fig. 18.24).
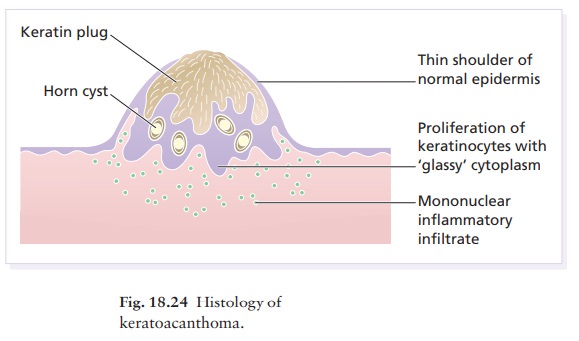
A typical lesion is symmetrical and composed of proliferating fronds of
epidermis that show mitotic activity but retain a well-differentiated squamous
appearance with the production of much ŌĆśglassyŌĆÖ keratin. The centre of the
cup-shaped mass is filled with keratin.
Treatment
Excision
or curettage and cautery are both effective. Occasionally, a further curetting
may be needed but this should be performed only once; if this is still
ineffective, the lesion must be excised.
Intraepidermal carcinoma (BowenŌĆÖs disease)
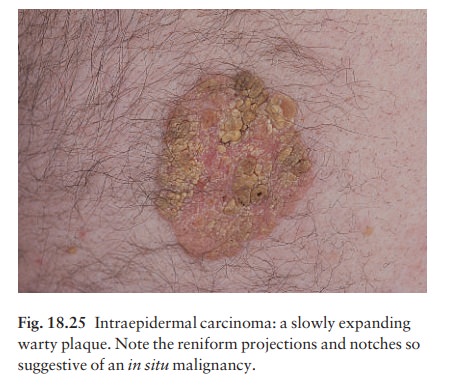
Usually
single, these slowly expanding pink scaly plaques (Fig. 18.25) take years to
reach a diameter of a few centimetres. Their border is sharply defined, with
reniform projections and notches. About 3%
The presence of several may be a clue to previous exposure to carcinogens (e.g. excessive sun exposure, arsenic in a tonic when young).
Differential diagnosis
An
intraepidermal carcinoma is often mistaken for psoriasis , discoid eczema,
super-ficial basal cell carcinoma or for
PagetŌĆÖs disease in the peri-anal region.
Treatment
These
lesions are unaffected by local steroids. Small lesions may occasionally be
left under observation in the frail and elderly. Cryotherapy or curettage are
the treatments of choice for small lesions on a site where healing should be
good (e.g. face or trunk); excision is an alternative. Photodynamic therapy is useful for large lesions on a poor healing
site (e.g. the lower legs of the elderly). Topical 5-fluorouracil or imiquimod
is helpful for multiple lesions (see Guidelines in Further reading).
Actinic keratoses
These
discrete rough-surfaced lesions crop up on sun-damaged skin. They are
premalignant, although only a few turn into a squamous cell carcinoma.
Cause
The effects of sun exposure are cumulative. Those with fair complexions living near the equator are most at risk and invariably develop these ŌĆśsun wartsŌĆÖ.
A
recent UK survey showed that one-third of men over 70 years had actinic
keratoses. Melanin protects, and actinic keratoses are not seen in black skin.
Con-versely, albinos are especially prone to develop them.
Presentation
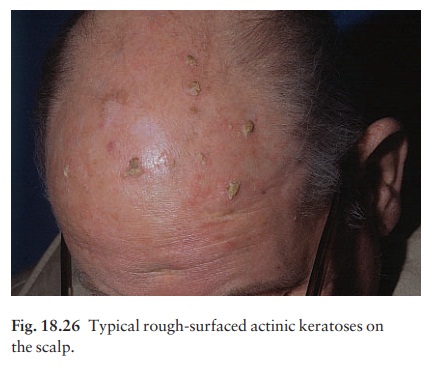
They
affect the middle-aged and elderly in temperate climates, but younger people in
the tropics. The pink or grey rough scaling macules or papules seldom exceed 1
cm in diameter (Fig. 18.26). Their rough surface is sometimes better felt than
seen.
Complications
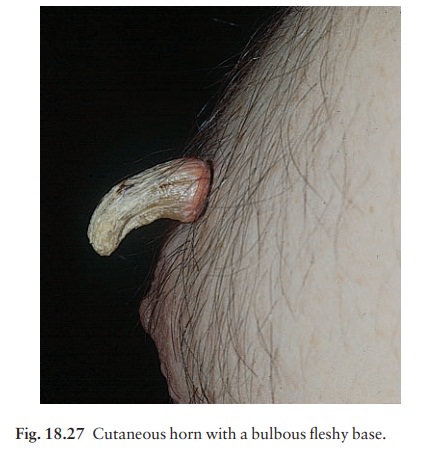
Transition
to a squamous cell carcinoma, although rare, should be suspected if a lesion
enlarges, ulcerates or bleeds. Luckily such tumours seldom metastasize. A
ŌĆścutaneous hornŌĆÖ is a hard keratotic protrusion based on an actinic keratosis,
a squamous cell papil-loma or a viral wart (Fig. 18.27).
Differential diagnosis
There
is usually no difficulty in telling an actinic ker-atosis from a seborrhoeic
wart, a viral wart, a keratoacanthoma, an intraepidermal carcinoma or a squamous
cell carcinoma.
Investigations
A biopsy is needed if there is concern over malignant change.
Histology
Alternating
zones of hyper- and parakeratosis overlie a thickened or atrophic epidermis.
The normal mat-uration pattern of the epidermis may be lost and occasional
pleomorphic keratinocytes may be seen. Solar elastosis is seen in the
superficial dermis.
Treatment
Freezing
with liquid nitrogen or carbon dioxide snow is simple and effective. Curettage
is best for large lesions and cutaneous horns. Multiple lesions, including
subclinical ones, can be treated with 5-fluorouracil cream (Formulary 1) after
special-ist advice. The cream is applied once or twice daily until there is a
marked inflammatory response in the treated area. This takes about 3 weeks and
only then should the applications be stopped. Healing is rapid and most
patients are very pleased with their ŌĆśnewŌĆÖ smooth skin. Severe discomfort from
the treatment may be alleviated by the short-term application of a local
steroid. 5-Fluorouracil cream is more effective for keratoses on the face than
on the arms. Altern-atively, less effective but causing less inflammation,
5-fluorouracil cream can be applied on just one or two days a week for 8 weeks.
Recently, 3% sodium diclofenac made up in a hyaluronan gel has come on the
market with a product licence to treat actinic
Photo-dynamic therapy, using
aminolaevulinic acid hydrochloride followed by blue light, is effective but
requires specialist facilities. Lesions that do not respond should be regarded
with suspicion, and biopsied.
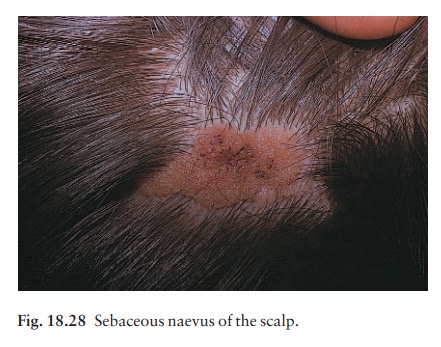
Sebaceous naevi (Fig.
18.28)
A
flat hairless area at birth, usually in the scalp, these naevi become yellower
and more raised at puberty. Basal cell carcinomas appear on some in adult life.
Related Topics