Chapter: Basic & Clinical Pharmacology : Diuretic Agents
Potassium-Sparing Diuretics
POTASSIUM-SPARING DIURETICS
Potassium-sparing
diuretics prevent K+ secretion by antagonizing the effects of aldosterone in
collecting tubules. Inhibition may occur by direct pharmacologic antagonism of
mineralocorticoid receptors (spironolactone,
eplerenone) or by inhibition of Na+ influx through ion
channels in the luminal membrane (amiloride,triamterene).
This latter property appears to be shared by ade-nosine antagonists, which
primarily blunt Na+ reabsorption in the PCT, but also blunt Na+ reabsorption and K+ secretion in
collecting tubules. Finally, ularitide (recombinant urodilatin), which is
currently still under investigation, blunts Na + uptake and Na+/K+-ATPase in collecting
tubules and increases GFR through its vascular effects. Nesiritide, which is
now commercially available for intravenous use only, increases GFR and blunts
Na+ reabsorption in both
proximal and collecting tubules.
Chemistry & Pharmacokinetics
The
structures of spironolactone and amiloride are shown in Figure 15–9.
Spironolactone is a synthetic steroid that acts as a competitive antagonist to
aldosterone. Onset and duration of its action are determined by the kinetics of
the aldosterone response in the tar-get tissue. Substantial inactivation of
spironolactone occurs in the liver. Overall, spironolactone has a rather slow
onset of action, requiring several days before full therapeutic effect is
achieved. Eplerenone is a spironolactone analog with much greater selectiv-ity
for the mineralocorticoid receptor. It is several hundredfold less active on
androgen and progesterone receptors than spironolac-tone, and therefore,
eplerenone has considerably fewer adverse effects.
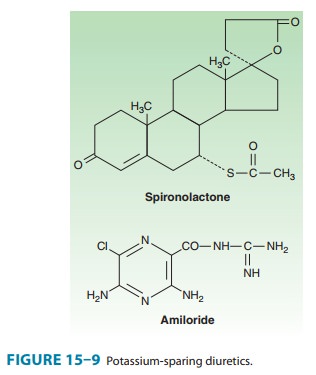
Amiloride
and triamterene are direct inhibitors of Na+ influx in the CCT
(cortical collecting tubule). Triamterene is metabolized in the liver, but
renal excretion is a major route of elimination for the active form and the
metabolites. Because triamterene is exten-sively metabolized, it has a shorter
half-life and must be given more frequently than amiloride (which is not
metabolized).
Pharmacodynamics
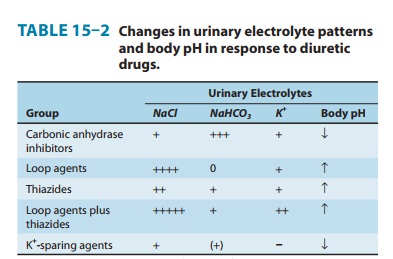
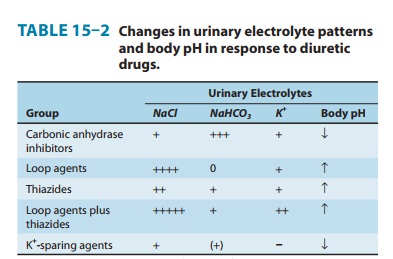
Potassium-sparing diuretics reduce Na+ absorption in the collect-ing tubules and ducts. Potassium absorption (and K+ secretion) at this site is regulated by aldosterone, as described above. Aldosterone antagonists interfere with this process. Similar effects are observed with respect to H+ handling by the intercalated cells of the collect-ing tubule, in part explaining the metabolic acidosis seen with aldosterone antagonists (Table 15–2).
Spironolactone
and eplerenone bind to mineralocorticoid recep-tors and blunt aldosterone
activity. Amiloride and triamterene do not block aldosterone, but instead
directly interfere with Na+ entry through the epithelial Na+ channels (ENaC,
Figure 15-5), in the apical membrane of the collecting tubule. Since K+ secretion is coupled
with Na+ entry in this segment, these agents are also effec-tive K+-sparing diuretics.
The
actions of the aldosterone antagonists depend on renal pros-taglandin
production. The actions of K+-sparing diuretics can be inhibited by NSAIDs under certain
conditions.
Clinical Indications & Dosage
(Table 15–6)
Potassium-sparing
diuretics are most useful in states of mineralo-corticoid excess or
hyperaldosteronism (also called aldosteronism), due either to primary
hypersecretion (Conn’s syndrome, ectopic adrenocorticotropic hormone
production) or secondary hyperal-dosteronism (evoked by heart failure, hepatic
cirrhosis, nephrotic syndrome, or other conditions associated with diminished
effec-tive intravascular volume). Use of diuretics such as thiazides or loop
agents can cause or exacerbate volume contraction and may cause secondary
hyperaldosteronism. In the setting of enhanced mineralocorticoid secretion and
excessive delivery of Na+ to distal nephron sites, renal K+ wasting occurs.
Potassium-sparing diuret-ics of either type may be used in this setting to
blunt the K+ secre-tory response.
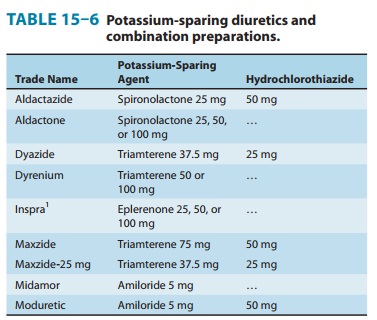
It has also been found that low doses of eplerenone (25–50 mg/d) may interfere with some of the fibrotic and inflammatory effects of aldosterone. By doing so, it can slow the progression of albu-minuria in diabetic patients. More important is that eplerenone has been found to reduce myocardial perfusion defects after myo-cardial infarction. In one clinical study, eplerenone reduced mortality rate by 15% (compared with placebo) in patients with mild to moderate heart failure after myocardial infarction.
Toxicity
A. Hyperkalemia
Unlike
most other diuretics, K+-sparing diuretics reduce urinary excretion of K+ (Table 15–2) and can
cause mild, moderate, or even life-threatening hyperkalemia. The risk of this
complication is greatly increased by renal disease (in which maximal K+ excre-tion may be
reduced) or by the use of other drugs that reduce or inhibit renin (β blockers, NSAIDs,
aliskiren) or angiotensin II activity (angiotensin-converting enzyme
inhibitors, angiotensin receptor inhibitors). Since most other diuretic agents
lead to K+ losses, hyperkalemia is more common when K+-sparing diuretics are
used as the sole diuretic agent, especially in patients with renal
insufficiency. With fixed-dosage combinations of K+-sparing and thiazide
diuretics, the thiazide-induced hypokalemia and meta-bolic alkalosis are ameliorated.
However, because of variations in the bioavailability of the components of
fixed-dosage forms, the thiazide-associated adverse effects often predominate.
Therefore, it is generally preferable to adjust the doses of the two drugs
separately.
B. Hyperchloremic Metabolic
Acidosis
By
inhibiting H+ secretion in parallel with K+ secretion, the K+-sparing diuretics can
cause acidosis similar to that seen with type IV renal tubular acidosis.
C. Gynecomastia
Synthetic
steroids may cause endocrine abnormalities by actions on other steroid
receptors. Gynecomastia, impotence, and benign prostatic hyperplasia (very
rare) all have been reported with spironolactone. Such effects have not been
reported with epler-enone, presumably because it is much more selective than
spironolactone for the mineralocorticoid receptor and virtually inactive on
androgen or progesterone receptors.
D. Acute Renal Failure
The
combination of triamterene with indomethacin has been reported to cause acute
renal failure. This has not been reported with other K+-sparing diuretics.
E. Kidney Stones
Triamterene
is only slightly soluble and may precipitate in the urine, causing kidney
stones.
Contraindications
Potassium-sparing
agents can cause severe, even fatal, hyper-kalemia in susceptible patients.
Patients with chronic renal insuf-ficiency are especially vulnerable and should
rarely be treated with these diuretics. Oral K+ administration should
be discontinued if K+-sparing diuretics are administered. Concomitant use of other
agents that blunt the renin-angiotensin system (β blockers, ACE
inhibitors,
ARBs) increases the likelihood of hyperkalemia. Patients with liver disease may
have impaired metabolism of tri-amterene and spironolactone, so dosing must be
carefully adjusted. Strong CYP3A4 inhibitors (eg, erythromycin, fluconazole,
dilti-azem, and grapefruit juice) can markedly increase blood levels of
eplerenone, but not spironolactone.
Related Topics