Chapter: Clinical Dermatology: Reactive erythemas and vasculitis
Polyarteritis nodosa
Polyarteritis
nodosa
Cause
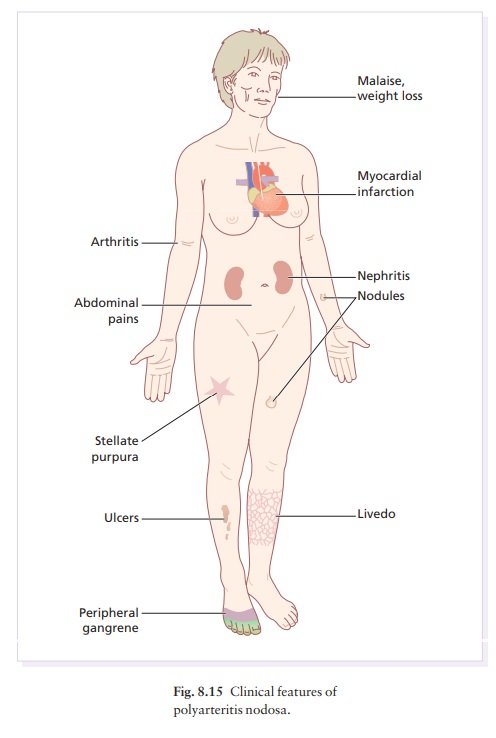
This necrotizing vasculitis of large arteries causes skin nodules, infarctive ulcers and peripheral gangrene.
Immune
complexes may initiate this vasculitis, and sometimes contain hepatitis B or C
virus or antigen. Other known causes are adulterated drugs, B-cell lymphomas
and immunotherapy.
Presentation
Tender
subcutaneous nodules appear along the line of arteries. The skin over them may
ulcerate or develop stellate patches of purpura and necrosis. Splinter
haemorrhages and a peculiar net-like vascular pat-tern (livedo reticularis) aid
the clinical diagnosis. The disorder may be of the skin only (cutaneous
polyarteritis nodosa), or also affect the kidneys, heart muscle, nerves and
joints (Fig. 8.15). Patients may be febrile, lose weight and feel pain in the
muscles, joints or abdomen. Some develop peripheral neuro-pathy, hypertension
and ischaemic heart disease. Renal involvement, with or without hypertension,
is common.
Course
Untreated,
systemic polyarteritis nodosa becomes chronic. Death, often from renal disease,
is common, even in treated patients.
Differential diagnosis
Embolism,
panniculitis and infarctions can cause a sim-ilar clinical picture. Wegener’s
granulomatosis, allergic granulomatosis, temporal arteritis, and the vasculitis
that accompanies systemic lupus erythematosus and rheumatoid arthritis should
be considered.
Investigations
The
laboratory findings are non-specific. An elevated ESR, neutrophil count, and
gammaglobulin level are common. Investigations for cryoglobulins, rheumatoid
factor, antinuclear antibody, antineutrophil antibod-ies and hepatitis C and B
surface antigen are worth-while, as are checks for disease in the kidneys,
heart, liver and gut. Low levels of complement suggest active disease. The use
of biopsy to confirm the diagnosis of large vessel vasculitis is not always
easy as the arterial involvement may be segmental, and surgery itself difficult.
Histological confirmation is most likely when biopsies are from a fresh lesion.
Affected vessels show aneurysmal dilatation or necrosis, fibrinoid changes in
their walls, and an intense neutrophilic infiltrate around and even in the
vessel wall.
Treatment
Systemic
steroids and cyclophosphamide improve chances of survival. Low-dose systemic
steroids alone are usually sufficient for the purely cutaneous form.
Related Topics