Chapter: Medical Surgical Nursing: Management of Patients With Chest and Lower Respiratory Tract Disorders
Pleural Effusion - Pleural Conditions
PLEURAL EFFUSION
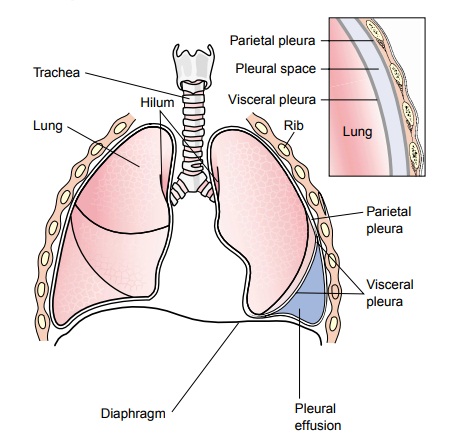
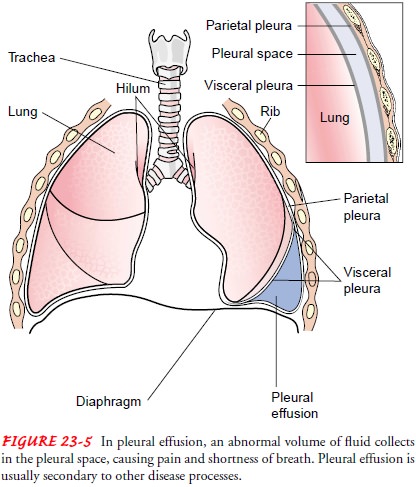
Pleural
effusion, a collection of fluid in the pleural space, is rarely a primary
disease process but is usually secondary to other dis-eases. Normally, the pleural
space contains a small amount of fluid (5 to 15 mL), which acts as a lubricant
that allows the pleural surfaces to move without friction (Fig. 23-5). Pleural
ef-fusion may be a complication of heart failure, TB, pneumonia, pulmonary
infections (particularly viral infections), nephrotic syndrome, connective
tissue disease, pulmonary embolism, and neoplastic tumors. Bronchogenic
carcinoma is the most common malignancy associated with a pleural effusion.
Pathophysiology
In certain disorders, fluid may accumulate in the pleural space to a point where it becomes clinically evident. This almost always has pathologic significance. The effusion can be composed of a relatively clear fluid, or it can be bloody or purulent.
An effusion of
clear fluid may be a transudate or an exudate. A transudate (filtrates of
plasma that move across intact capillary walls) occurs when factors influencing
the formation and reabsorption of pleural fluid are altered, usually by
imbalances in hydrostatic or oncotic pressures. The finding of a transudative
effusion generally implies that the pleural membranes are not diseased. The
most common cause of a transudative effusion is heart failure. An exu-date
(extravasation of fluid into tissues or a cavity) usually results from
inflammation by bacterial products or tumors involving the pleural surfaces.
Clinical Manifestations
Usually
the clinical manifestations are those caused by the underly-ing disease.
Pneumonia causes fever, chills, and pleuritic chest pain, whereas a malignant
effusion may result in dyspnea and coughing. The size of the effusion and the
patient’s underlying lung disease determine the severity of symptoms. A large
pleural effusion causes shortness of breath. When a small to moderate pleural
effusion is present, dyspnea may be absent or only minimal. The severity of the
symptoms assessed depends on the time course of the develop-ment of the pleural
effusion and the patient’s underlying disease.
Assessment and Diagnostic Findings
Assessment
of the area of the pleural effusion reveals decreased or absent breath sounds,
decreased fremitus, and a dull, flat sound when percussed. In an extremely
large pleural effusion, the as-sessment reveals a patient in acute respiratory
distress. Tracheal deviation away from the affected side may also be noted.
Physical
examination, chest x-ray, chest CT scan, and thora-centesis confirm the
presence of fluid. In some instances, a lateral decubitus x-ray is obtained.
For this x-ray, the patient lies on the affected side in a side-lying position.
A pleural effusion can be di-agnosed because this position allows for the
“layering out” of the fluid, and an air–fluid line is visible.
Pleural
fluid is analyzed by bacterial culture, Gram stain, acid-fast bacillus stain
(for TB), red and white blood cell counts, chemistry studies (glucose, amylase,
lactic dehydrogenase, pro-tein), cytologic analysis for malignant cells, and
pH. A pleural biopsy also may be performed.
Medical Management
The
objectives of treatment are to discover the underlying cause, to prevent
reaccumulation of fluid, and to relieve discomfort, dyspnea, and respiratory
compromise. Specific treatment is di-rected at the underlying cause (eg, heart
failure, pneumonia, lung cancer, cirrhosis). If the pleural fluid is an
exudate, more exten-sive diagnostic procedures are performed to determine the
cause. Treatment for the primary cause is then instituted.
Thoracentesis
is performed to remove fluid, to obtain a spec-imen for analysis, and to
relieve dyspnea and respiratory com-promise. Thoracentesis may be performed
under ultrasound guidance. Depending on the size of the pleural effu-sion, the
patient may be treated by removing the fluid during the thoracentesis procedure
or by inserting a chest tube connected to a water-seal drainage system or
suction to evacuate the pleural space and re-expand the lung.
If
the underlying cause is a malignancy, however, the effusion tends to recur
within a few days or weeks. Repeated thoracenteses result in pain, depletion of
protein and electrolytes, and some-times pneumothorax. Once the pleural space
is adequately drained, a chemical pleurodesis may be performed to obliterate
the pleural space and prevent reaccumulation of fluid. Pleurode-sis may be
performed using a thoracoscopic approach or via a chest tube. Chemically
irritating agents (eg., bleomycin or talc) are instilled in the pleural space.
With the chest tube insertion approach, after the agent is instilled, the chest
tube is clamped for 60 to 90 minutes and the patient is assisted to assume
various po-sitions to promote uniform distribution of the agent and to
max-imize its contact with the pleural surfaces. The tube is unclamped as
prescribed, and chest drainage may be continued several days longer to prevent
reaccumulation of fluid and to promote the for-mation of adhesions between the
visceral and parietal pleurae.
Other
treatments for malignant pleural effusions include sur-gical pleurectomy,
insertion of a small catheter attached to a drainage bottle for outpatient
management, or implantation of a pleuroperitoneal shunt. A pleuroperitoneal
shunt consists of two catheters connected by a pump chamber containing two
one-way valves. Fluid moves from the pleural space to the pump chamber and then
to the peritoneal cavity. The patient manually pumps on the reservoir daily to
move fluid from the pleural space to the peritoneal space (Taubert &
Wright, 2000).
Nursing Management
The
nurse’s role in the care of the patient with a pleural effusion includes
implementing the medical regimen. The nurse prepares and positions the patient
for thoracentesis and offers support throughout the procedure. Pain management
is a priority, and the nurse assists the patient to assume positions that are
the least painful. However, frequent turning and ambulation are impor-tant to
facilitate drainage. The nurse administers analgesics as pre-scribed and as
needed.
If
a chest tube drainage and water-seal system is used, the nurse is responsible
for monitoring the system’s function and recording the amount of drainage at
prescribed intervals. Nurs-ing care related to the underlying cause of the
pleural effusion is specific to the underlying condition.
If
the patient is to be managed as an outpatient with a pleural catheter for
drainage, the nurse is responsible for educating the pa-tient and family
regarding management and care of the catheter and drainage system.
Related Topics