Chapter: Basic & Clinical Pharmacology : Drugs Used in Heart Failure
Pathophysiology of Cardiac Performance
Pathophysiology of Cardiac Performance
Cardiac performance is a function of four primary factors:
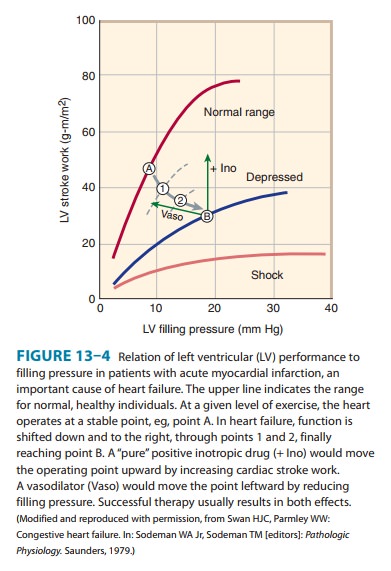
1. Preload: When some measure of left ventricular performancesuch as stroke volume or stroke work is plotted as a function of left ventricular filling pressure or end-diastolic fiber length, the resulting curve is termed the left ventricular function curve (Figure 13–4). The ascending limb (< 15 mm Hg filling pres-sure) represents the classic Frank-Starling relation described in physiology texts. Beyond approximately 15 mm Hg, there is a plateau of performance. Preloads greater than 20–25 mm Hg result in pulmonary congestion. As noted above, preload is usu-ally increased in heart failure because of increased blood volume and venous tone. Because the function curve of the failing heart is lower, the plateau is reached at much lower values of stroke work or output. Increased fiber length or filling pressure increases oxygen demand in the myocardium, as described. Reduction of high filling pressure is the goal of salt restriction and diuretic therapy in heart failure. Venodilator drugs (eg, nitroglycerin) also reduce preload by redistributing blood away from the chest into peripheral veins.
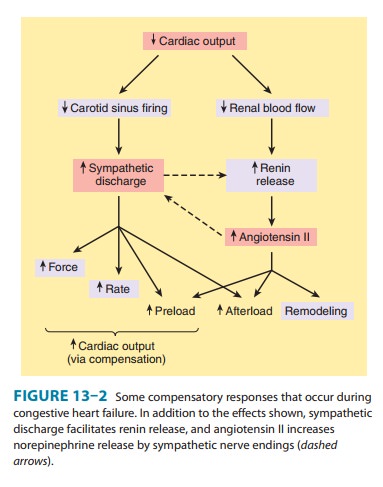
2. Afterload: Afterload is the resistance against which the heartmust pump blood and is represented by aortic impedance and systemic vascular resistance. As noted in Figure 13–2, as cardiac output falls in chronic failure, a reflex increase in systemic vas-cular resistance occurs, mediated in part by increased sympa-thetic outflow and circulating catecholamines and in part by activation of the renin-angiotensin system. Endothelin, a potent vasoconstrictor peptide, is also involved. This sets the stage for the use of drugs that reduce arteriolar tone in heart failure.
3. Contractility: Heart muscle obtained by biopsy from patientswith chronic low-output failure demonstrates a reduction in intrinsic contractility. As contractility decreases in the patient, there is a reduction in the velocity of muscle shortening, the rate of intraventricular pressure development (dP/dt), and the stroke output achieved (Figure 13–4). However, the heart is usually still capable of some increase in all of these measures of contractility in response to inotropic drugs.
4. Heart rate: The heart rate is a major determinant of cardiacoutput. As the intrinsic function of the heart decreases in fail-ure and stroke volume diminishes, an increase in heart rate— through sympathetic activation of β adrenoceptors—is the first compensatory mechanism that comes into play to maintain cardiac output.
Related Topics