Chapter: Medical Surgical Nursing: Gastrointestinal Intubation and Special Nutritional Modalities
Parenteral Nutrition
Parenteral Nutrition
Parenteral nutrition (PN) is a method of providing nutrients tothe
body by an IV route. It is a very complex admixture of indi-vidual chemicals
combined in a single container. The components of a PN admixture are proteins,
carbohydrates, fats, electrolytes, vitamins, trace minerals, and sterile water.
The goals of PN are to improve nutritional status, establish a positive
nitrogen balance, maintain muscle mass, promote weight gain, and enhance the
healing process.
ESTABLISHING POSITIVE NITROGEN BALANCE
When a
patient’s intake of protein and nutrients is significantly less than that required
by the body to meet energy expenditures, a state of negative nitrogen balance
results. In response, the body begins to convert the protein found in muscles
into carbohydrates to be used to meet energy needs. The result is muscle
wasting, weight loss, fatigue, and, if left uncorrected, death.
The
average postoperative adult patient requires approximately 1500 calories per
day to keep the body from using its own store of protein. Traditional IV fluids
do not provide sufficient calories or nitrogen to meet the body’s daily
requirements. PN solutions, which supply nutrients such as dextrose, amino
acids, elec-trolytes, vitamins, minerals, and fat emulsions, provide enough
calories and nitrogen to meet the patient’s daily nutritional needs. In
general, PN can provide 30 to 35 kcal/kg of body weight and 1.0 to 1.5 g of
protein/kg of body weight (Rombeau & Rolandelli, 2000).
The
patient with fever, trauma, burns, major surgery, or hy-permetabolic disease
may require up to 10,000 additional calo-ries daily. The volume of fluid
necessary to provide these calories would surpass fluid tolerance and lead to
pulmonary edema or heart failure. To provide the required calories in small
volume, it is necessary to increase the concentration of nutrients and use a
route of administration (ie, a large, high-flow vein [subclavian vein]) that
will rapidly dilute incoming nutrients to the proper levels of body tolerance.
When
highly concentrated glucose is administered, caloric re-quirements are
satisfied and the body uses amino acids for pro-tein synthesis rather than for
energy. Additional potassium is added to the solution to maintain proper
electrolyte balance and to transport glucose and amino acids across cell
membranes. To prevent deficiencies and fulfill requirements for tissue
synthesis, other elements, such as calcium, phosphorus, magnesium, and sodium
chloride, are added (Rombeau & Rolandelli, 2000).
CLINICAL INDICATIONS
The
indications for PN include a 10% deficit in body weight (compared with
preillness weight), an inability to take oral food or fluids within 7 days
after surgery, and hypercatabolic situations such as major infection with
fever. In both the home and hospi-tal setting, PN is indicated in the following
situations:
•
The patient’s intake is insufficient to maintain an
anabolic state (eg, severe burns, malnutrition, short bowel syndrome, AIDS,
sepsis, cancer).
•
The patient’s ability to ingest food orally or by
tube is im-paired (eg, paralytic ileus, Crohn’s disease with obstruction,
postradiation enteritis, severe hyperemesis gravidarum in pregnancy).
•
The patient is not interested in or is unwilling to
ingest ad-equate nutrients (eg, anorexia nervosa, postoperative elderly
patients).
•
The underlying medical condition precludes being
fed orally or by tube (eg, acute pancreatitis, high enterocuta-neous fistula).
•
Preoperative and postoperative nutritional needs
are pro-longed (eg, extensive bowel surgery).
FORMULAS
A
total of 2 to 3 L of solution is administered over a 24-hour period using a
filter (1.2-micron particulate filter). Before admin-istration, the PN infusion
must be inspected for clarity and any pre-cipitate. The label is compared with
the physician’s order, noting the expiration date. Fat emulsions (Intralipid)
may be infused si-multaneously with PN through a Y-connector close to the
infusion site. Fat emulsions should not be filtered. Before administration, the
fat emulsion solution is inspected for frothiness, separation, or oily
appearance. Usually 500 mL of a 10% emulsion is admin-istered over 4 to 6
hours, one to three times a week. Fat emulsions can provide up to 30% of the
total daily calorie intake.
Lipid
emulsions can be admixed with other components of PN to create a total nutrient admixture (TNA). TNA is
com-monly called a “three-in-one” formulation. All the parenteral nu-trient
components are mixed in one container and administered to the patient over a
24-hour period. A special final filter (1.5 micron filter) is used with this
solution. Before administration, the solu-tion is observed for oil droplets
that have separated from the so-lution, forming a noticeable layer (cracking of
lipid emulsion); such a solution should be discarded. Advantages of the TNA
over PN are cost savings in preparation and equipment, decreased risk of
contamination, decreased risk of catheter contamination, decreased pharmacy
preparation time, less nursing time, and increased patient convenience and
satisfaction. Ideally, the pharmacist, nutritionist, and physician collaborate
to determine the specific formula needed.
INITIATING THERAPY
PN
solutions are initiated slowly and advanced gradually each day to the desired
rate, as the patient’s fluid and glucose tolerance per-mits. The patient’s
laboratory test results and response to PN therapy are monitored on an ongoing
basis by the nutritional support team. Standing orders are initiated for
weighing the pa-tient; monitoring intake, output, and blood glucose; and
baseline and periodic monitoring of complete blood count, platelet count, and
chemistry panel, including serum carbon dioxide, magne-sium, phosphorus,
triglycerides, and prealbumin. A 24-hour urine nitrogen determination may be
performed for analysis of nitrogen balance. In most hospitals, the physician
prescribes PN solutions on a daily standard PN order form. The formulation of
the PN solutions is calculated carefully each day to meet the com-plete
nutritional needs of the individual patient.
ADMINISTRATION METHODS
Various
vascular access devices are used to administer PN solu-tions in clinical
practice. PN may be administered by either pe-ripheral or central IV lines,
depending on the patient’s condition and the anticipated length of therapy.
Peripheral Method
To
supplement oral intake when complete bowel rest is not indi-cated and NG or
nasoenteric suction is not required, a peripheral parenteral nutrition (PPN)
formula may be prescribed. PPN is ad-ministered through a peripheral vein; this
is possible because the solution is less hypertonic than PN solution. PPN
formulas are not nutritionally complete. Protein and dextrose are limited.
Dex-trose concentrations of more than 10% should not be adminis-tered through
peripheral veins because they irritate the intima (innermost walls) of small
veins, causing chemical phlebitis. Lipids are administered simultaneously to
buffer the PPN and to protect the peripheral vein from irritation. The usual
length of therapy using PPN is 5 to 7 days (Hamilton, 2000).
Central Method
Because
PN solutions have five or six times the solute con-centration of blood (and
exert an osmotic pressure of about 2000 mOsm/L), they are injurious to the
intima of peripheral veins. Therefore, to prevent phlebitis and other venous
compli-cations, these solutions are administered into the vascular system
through a catheter inserted into a high-flow, large blood vessel (the
subclavian vein). Concentrated solutions are then very rapidly di-luted to
isotonic levels by the blood in this vessel.
Four
types of central venous access devices
(CVAD) are available—nontunneled (or percutaneous) central catheters,
pe-ripherally inserted central catheters, tunneled catheters, and im-planted
ports. Whenever one of these catheters is inserted, catheter tip placement
should be confirmed by x-ray studies before PN therapy is initiated. The
optimal position is the midproximal third of the superior vena cava.
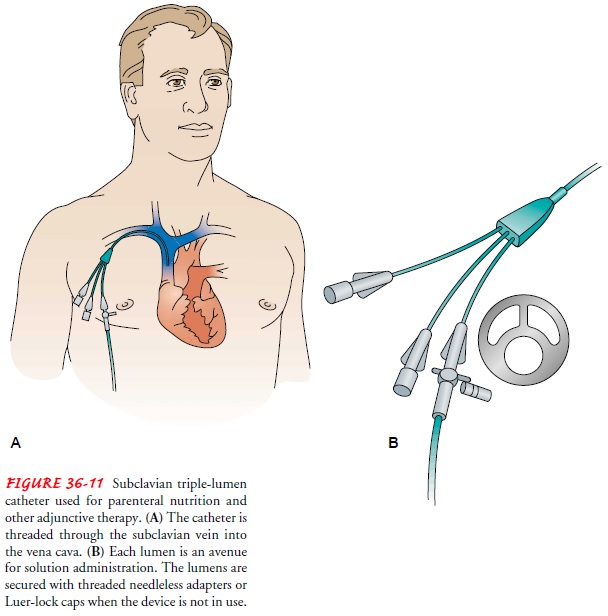
NONTUNNELED CENTRAL CATHETERS
Nontunneled
central catheters are used for short-term (less than 30 days) IV therapy in the
acute care, long-term care, and home care settings. The physician inserts these
catheters. Examples of non-tunneled central catheters are Vas Cath,
Percutaneous Subclavian, and Hohn catheters. The subclavian vein is the most
common ves-sel used, because the subclavian area provides a stable insertion
site to which the catheter can be anchored, allows the patient freedom of
movement, and provides easy access to the dressing site. The jugular or femoral
vein also may be used. Single-, double-, and triple-lumen central catheters are
available for central lines. To en-sure accessibility, a triple-lumen
subclavian catheter should be used, because it offers three ports for various
uses (Fig. 36-11). The 16-gauge distal lumen can be used to infuse blood or
other viscous flu-ids. The 18-gauge middle lumen is reserved for PN infusion.
The 18-gauge proximal port can be used for administration of blood or
medications. A port not being used for fluid administration can be used for
obtaining blood specimens if indicated.
If a
single-lumen central catheter is used for administering PN, various
restrictions apply. Blood cannot be drawn from the catheter and medications
cannot be administered through it, because the medication may be incompatible
with the components of the nu-tritional solution (insulin is an exception). If
medications must be given, they must be infused through a separate peripheral
IV line, not by piggyback into the PN line. Transfusions of blood products also
cannot be given through the main line, because red cells may possibly coat the
lumen of the catheter, thereby reducing the flow of the nutritional solution.
PERIPHERALLY INSERTED CENTRAL CATHETERS
Peripherally inserted central catheters (PICC) are used
forintermediate-term (3 to 12 months) IV therapy in the hospital, long-term
care, or home setting. These catheters may be inserted at the bedside or in the
outpatient setting by a specially trained nurse. The basilic or cephalic vein
is accessed through the ante-cubital space, and the catheter is threaded to a
designated loca-tion, depending on the type of solution to be infused (superior
vena cava for PN). Taking of blood pressure and blood specimens from the
extremity with the PICC is avoided.
TUNNELED CENTRAL CATHETERS
Tunneled
central catheters are for long-term use and may remain in place for many years.
These catheters are cuffed and can have single or double lumens; examples are
the Hickman, Goshong, and Permacath. These catheters are inserted surgically.
They are threaded under the skin (reducing the risk of ascending infection) to
the subclavian vein, and the distal end of the catheter is ad-vanced into the
superior vena cava 2 to 3 cm above the junction with the right atrium.
IMPLANTED PORTS
Implanted ports are also used for long-term home IV therapy; ex-amples include the Port-A-Cath, Mediport, Hickman Port, and P.A.S. Port. Instead of exiting from the skin, as do the Hickman and Groshong catheters, the end of the catheter is attached to a small chamber that is placed in a subcutaneous pocket, either on the anterior chest wall or on the forearm. The subcutaneous port requires minimal care and allows the patient complete freedom of activity.
Implanted ports are more expensive than the external catheters, and
access requires passing a special needle (Huber-tipped) through the skin into the
chamber to initiate IV therapy. Taking of blood pressure and blood specimens
from the extremity with the port system is avoided.
NONTUNNELED CENTRAL CATHETER INSERTION
The
procedure is explained so that the patient understands the importance of not touching
the catheter insertion site and is aware of what to expect during the insertion
procedure. To insert the catheter, the patient is placed supine, in head-low
position (to produce dilation of neck and shoulder vessels, which makes entry
easier and prevents air embolus). The area is shaved if necessary, and the skin
is prepared with acetone and alcohol to remove sur-face oils. Final skin
preparation includes cleaning with tincture of 2% iodine or chlorhexidine. To
afford maximal accuracy in the placement of the catheter, the patient is
instructed to turn the head away from the site of venipuncture and to remain
motion-less while the catheter is inserted and the wound is dressed.
The
preferred insertion route is the subclavian vein, which leads into the superior
vena cava. The external jugular route can be used, but usually only in
emergency situations. Because a non-tunneled central catheter is always a
potential source of serious infection, the site should be changed every 4 weeks
or as recom-mended by the Centers for Disease Control and Prevention.
Sterile
drapes are applied to the upper chest. The patient may be asked to wear a
facemask to prevent the spread of micro-organisms. Procaine or lidocaine is
injected to anesthetize the skin and underlying tissues. The target area is the
inferior border at the midpoint of the clavicle. A large-bore needle on a
syringe is inserted and moved parallel to and beneath the clavicle until it
enters the vein. The syringe is then detached and a radiopaque catheter is
inserted through the needle into the vein.
When
the catheter is positioned, the needle is withdrawn and the hub of the catheter
is attached to the IV tubing. Until the sy-ringe is detached from the needle
and the catheter is inserted, the patient may be asked to perform the Valsalva
maneuver. (To do this, the patient is instructed to take a deep breath, hold
it, and bear down with mouth closed. Compression of the abdomen may also
accomplish the maneuver.) The Valsalva maneuver is per-formed to produce a positive
phase in central venous pressure, to lessen the possibility of air being drawn
into the circulatory sys-tem (air embolism). The physician sutures the catheter
to the skin to avoid inadvertent removal.
The
catheter insertion site is swabbed with either tincture of 2% iodine or a
chlorhexidine solution. A gauze or transparent dressing is applied using strict
sterile technique. An isotonic IV solution, such as dextrose 5% in water (D5W), is administered to
keep the vein patent.
The
position of the tip of the catheter is checked with fluo-roscopy to confirm its
location in the superior vena cava and to rule out a pneumothorax resulting
from puncture of the pleura. Once the catheter position is confirmed, the
prescribed PN so-lution is started. The initial rate of infusion is usually 50
mL/hour, and the rate is gradually increased to the maintenance rate or
predetermined dose (eg, 100 to 125 mL/hour). An infusion pump is always used
for administration of PN or PPN.
An
injection site cap is attached to the end of each central catheter lumen,
creating a closed system. IV infusion tubing is connected to the insertion site
cap of the central catheter with a threaded needleless adapter or Luer-lock
device. Each lumen is la-beled according to location (proximal, middle,
distal). To ensure patency, all lumens are flushed with a diluted heparin flush
initially, daily when not in use, after each intermittent infusion, after blood
drawing, and whenever an infusion is disconnected. Force is never used to flush
the catheter. If resistance is met, aspiration may be effective in cleansing
the lumen; if this is not effective, the physician is notified. Low-dose t-PA
(alteplase) may be prescribed to dissolve a clot or fibrin sheath. If attempts
to clear the lumen are ineffective, the lumen is labeled as “clotted off.”
DISCONTINUING PARENTERAL NUTRITION
The PN
solution is discontinued gradually to allow the patient to adjust to decreased
levels of glucose. After administration of the PN solution is terminated,
isotonic glucose is administered for several hours to protect against rebound
hypoglycemia. Provid-ing oral carbohydrates will shorten the tapering time.
Specific symptoms of rebound hypoglycemia include weakness, faintness,
sweating, shakiness, feeling cold, confusion, and increased heart rate. Once
all IV therapy is completed, the nurse (with a physi-cian’s order) removes the
nontunneled central venous catheter or PICC and applies an occlusive dressing
to the exit site. Tunneled catheters and implanted ports are removed by the
physician.
In
cases of serious illness when death is imminent, some pa-tients or families may
request that PN be discontinued. This dif-ficult issue poses many ethical
questions, some of which are discussed in Chart 36-3.
Related Topics