Chapter: Essentials of Anatomy and Physiology: Endocrine System
Parathyroid Glands - Endocrine Glands and Their Hormones
Parathyroid Glands
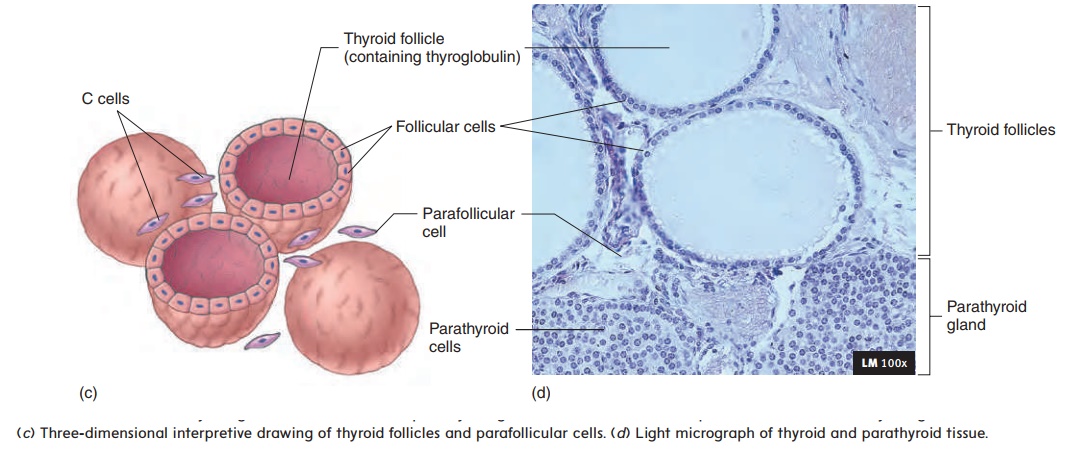
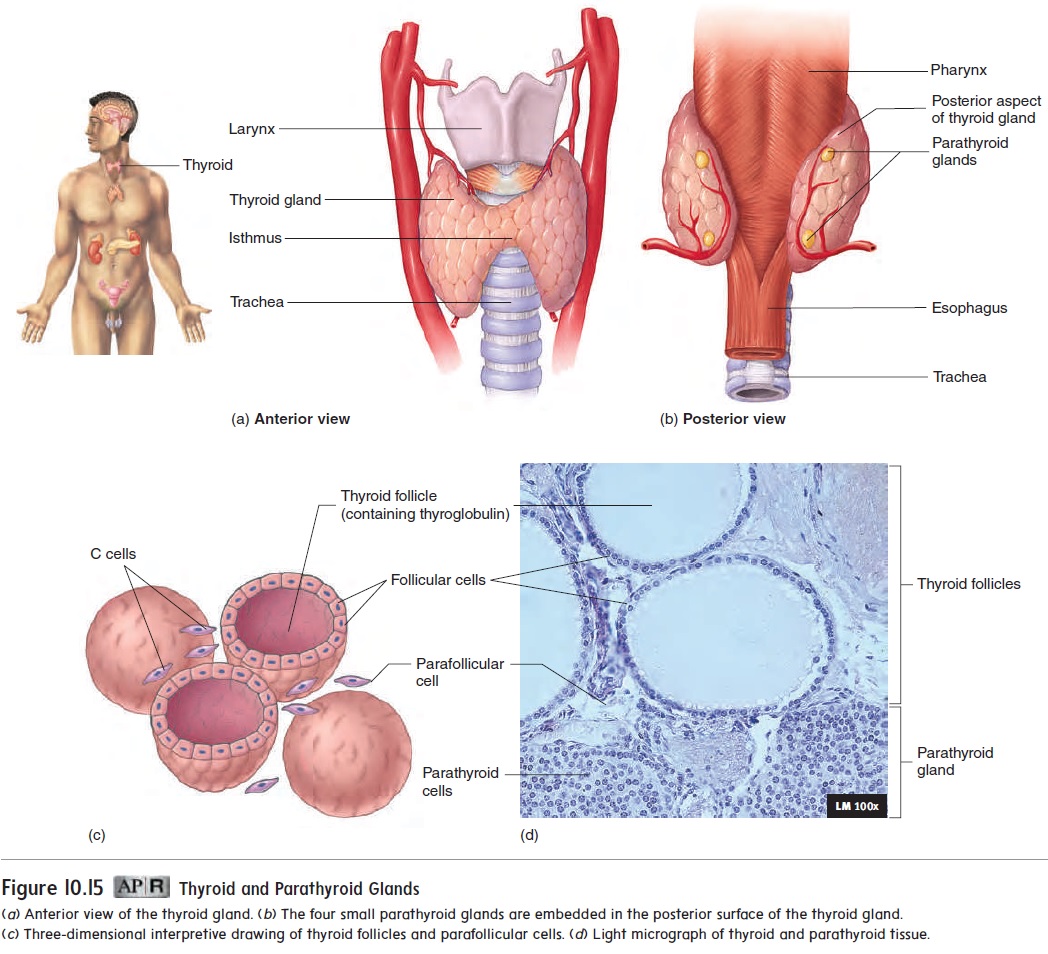
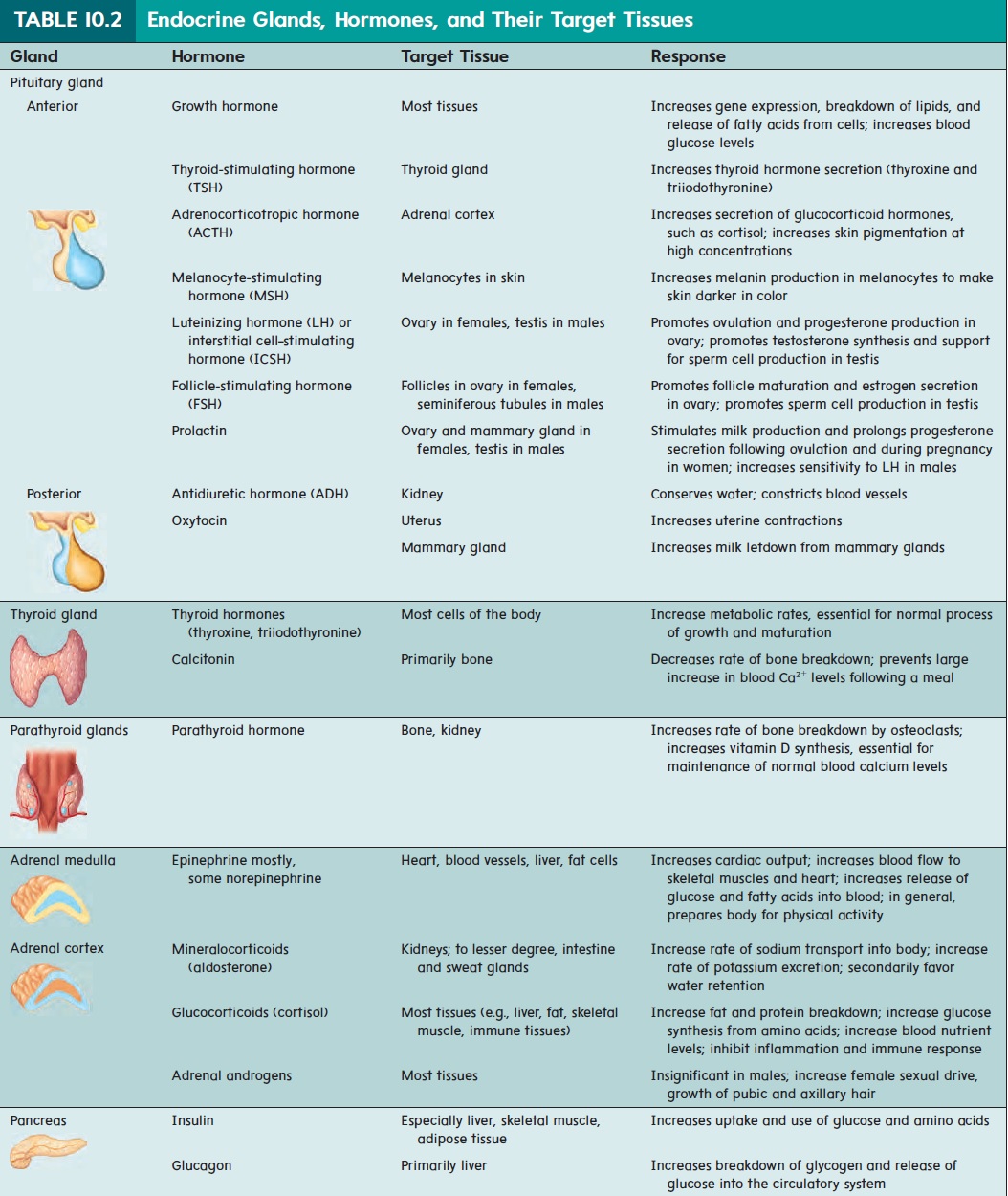
Four tiny parathyroid (par-ă-thı̄′ royd) glands are embedded in the posterior wall of the thyroid gland (see figure 10.15b,d). The parathyroid glands secrete a hormone called parathyroid hormone(PTH), which is essential for the regulation of blood calcium levels(table 10.2). In fact, PTH is more important than calcitonin in regulating blood Ca2+ levels. PTH has many effects:
1. PTH binds to membrane-bound receptors of renal tubule cells, which increases active vitamin D formation.Vitamin D causes the epithelial cells of the intestine to increase Ca2+ absorption.
2. PTH binds to receptors on osteoblasts. Substancesreleased by the osteoblasts increase osteoclast activity and cause reabsorption of bone tissue to release Ca2+ into the circulatory system.
3. PTH binds to receptors on cells of the renal tubules and decreases the rate at which Ca2+ is lost in the urine.
4. PTH acts on its target tissues to raise blood Ca2+ levels to normal.
Vitamin D is produced from precursors in the skin that are modified by the liver and kidneys. Ultraviolet light acting on the skin is required for the first stage of vitamin D synthesis, and the final stage of synthesis in the kidney is stimulated by PTH. Vitamin D can also be supplied in the diet.
Decreasing blood Ca2+ levels stimulate an increase in PTH secretion (figure 10.17). For example, if too little Ca2+ is consumed in the diet or if a person suffers from a prolonged lack of vitamin D, blood Ca2+levels decrease, and PTH secretion increases. The increased PTH increases the rate of bone reabsorption. Blood Ca2+ levels can be maintained within a normal range, but prolonged reabsorption of bone results in reduced bone density, as manifested by soft, flexible bones that are easily deformed in young people and porous, fragile bones in older people.
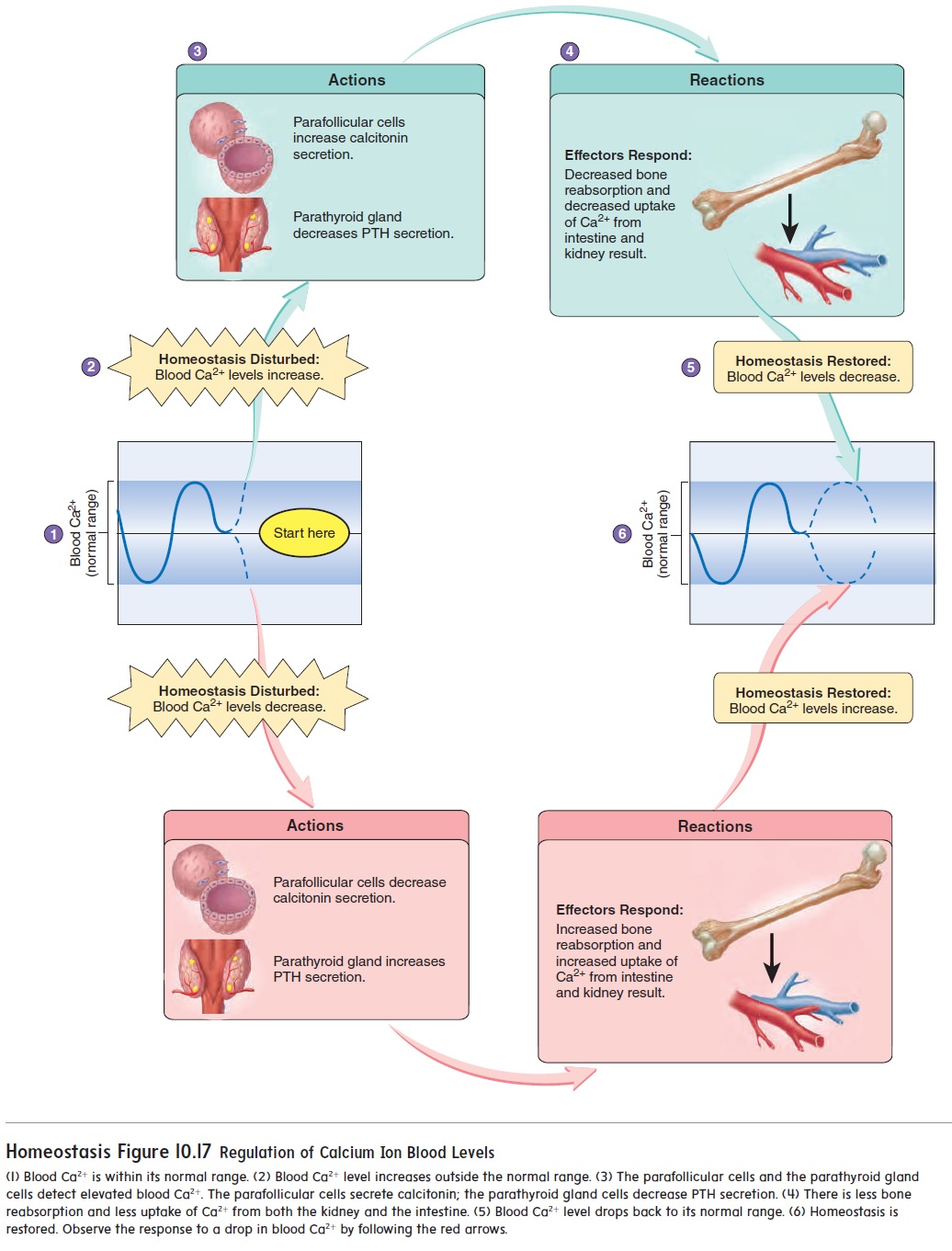
Increasing blood Ca2+ levels cause a decrease in PTH secretion (figure 10.17). The decreased PTH secretion leads to reduced blood Ca2+ levels. In addition, increasing blood Ca2+ levels stimulate cal-citonin secretion, which also causes blood Ca2+ levels to decline.
An abnormally high rate of PTH secretion is called hyper-parathyroidism. One cause is a tumor in a parathyroid gland. Theelevated blood levels of PTH increase bone reabsorption and elevate blood Ca2+levels. As a result, bones can become soft, deformed, and easily fractured. In addition, the elevated blood Ca2+ levels make nerve and muscle cells less excitable, resulting in fatigue and muscle weakness. The excess Ca2+ can be deposited in soft tissues of the body, causing inflammation. In addition, kidney stones can result
An abnormally low rate of PTH secretion, called hypopara-thyroidism, can result from injury to or the surgical removalof the thyroid and parathyroid glands. The low blood levels of PTH lead to reductions in the rate of bone reabsorption and the formation of vitamin D. As a result, blood Ca2+ levels decrease. In response to low blood Ca2+ levels, nerves and muscles become excitable and produce spontaneous action potentials that cause frequent muscle cramps or tetanus. Severe tetanus can affect the respiratory muscles; breathing stops, resulting in death.
Related Topics