Chapter: Medicine Study Notes : Reproductive and Obstetrics
Other Complications of Later Pregnancy
Other Complications of Later Pregnancy
·
Key complications: preterm
labour, pre-eclampsia and small babies
Antepartum haemorrhage (APH)
·
Any bleeding from the genital
tract between 20th week and delivery
·
Differential diagnosis:
o Placenta praevia:
§ Implantation of the placenta in the lower uterine segment near or over
the internal os.
§ Graded 1 to 4 (worst)
§ Risk factors: prior c-section (uterine scar), grand multiparity (>5), multiple birth, maternal age >35, tobacco/cocaine use, fibroid uterus (ie anything that causes scarring or reduces places for embryo to attach)
o Placental abruption:
§ Premature separation of normally implanted placenta from the uterine wall
§ Risk factors: maternal age, multiparity, maternal shock, poor nutrition, gestational
diabetes, BP, smoking, anything that causes maternal vasoconstriction (trauma,
cocaine, etc)
o Onset of premature labour
o Bleeding from other parts of the genital tract (eg cervical polyps, vaginitis, vulval varicosities)
o Fetal: Vasa praevia. Bleeding from an abnormal fetal vessel attached to
the membranes over the internal os. Need ROM for this to occur. Mother will not
be shocked
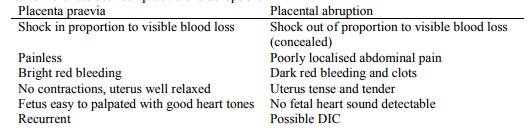
· Clinical differences between praevia and abruption:
o History: previous bleeds, initiating factors, eg trauma, colitis
o ALWAYS ultrasound: exclude placenta praevia (detects 95 – 98% of cases)
and major abruption with placental separation.
o NO vaginal exam until praevia excluded
o APT test to distinguish fetal from maternal blood
o Bloods to monitor hypovolaemic shock, DIC
o Fetal well-being, eg CTG
o If major blood loss, treat for shock ® transfuse, give O2
o Give steroids
o If fetus alive, consider c-section before labour
o If fetus dead, induce
·
Treatment:
o If Rhesus negative and no antibodies yet, give Anti-D within 72 hours
· Placenta praevia: If substantial, hospitalised till delivery, Caesar at 38 weeks
·
Placental abruption: Hospitalise.
Serious risk of PPH, also acute renal failure, pituitary necrosis, etc. Monitor
retro-placental clot by serial ultrasound
Rhesus haemolytic disease*
· Aetiology: if Rhesus –ive mother is „contaminated‟ by blood from a Rhesus +ive baby Þ anti-D IgG antibodies (isoimmunisation)
·
Later in the pregnancy, or in a
following pregnancy, IgG can cross the placenta causing Erythroblastosis
Fetalis (® stiff oedematous lungs and hydrops – widespread oedema)
·
Test for anti-D antibodies in all
Rhesus –ive mothers at booking and in 2nd trimester. If elevated then monitor carefully
· Anti-D immunoglobulin given prophylactically to Rh –ive mothers:
o Within 72 hours after incident (eg amnio, threatened miscarriage,
spontaneous abortion, any risk of trans-placental haemorrhage – TPH, etc)
o After birth if baby Rh +ive or group not known
o This prevents „iso-immunisation‟ – gobbles up antigen before mothers
immune system generates antibodies
o Don‟t give anti-D if mother already producing Anti-D
Premature labour
·
= Labour < 37 weeks
·
8% of babies, 85% of neonatal
deaths
·
Over-diagnosed – over 80%
diagnosed will deliver at term without treatment. Hard to diagnose – regular
uterine contractions are normal, cervical changes in labour can be subtle
·
Braxton-Hicks contractions are
usual from 30 weeks but are not painful
·
History: Is it true labour: check
nature of contractions, urinary frequency (?UTI), backache, spotting or a
change in vaginal discharge (normal in 3rd trimester – lots, white, non-smelling).
· Risks:
o Strongest association is previous preterm birth (4 times
risk)
o Previous mid-trimester abortions (2 or more) – not 1st trimester spontaneous abortions
·
Aetiology:
o Spontaneous: 40%
o Multiple pregnancy: 10%, 10 times risk
o Maternal or fetal conditions (25%)
o Premature, preterm rupture of membranes (PPROM = rupture of membranes before labour commences and preterm)
o APH
o > 28 weeks, 80 – 90% survival
o > 32 weeks, similar survival as term babies but complications
· Management:
o Investigations: temperature, BP, pulse, SFH, view cervix for clots etc
(do NOT view cervix if risk of praevia – do US first), ?infection screen, US,
MSU, fetal welfare
o Consider tocolysis (inhibiting labour):
§ Inhibit uterine contractions – allows time for steroids to work and for transfer to neonatal unit
§ b agonists – Ritodrine and Salbutamol (risk of pulmonary oedema) prolong labour for ~ 24 hours. Adverse effects: maternal and fetal tachycardia, vasodilation ® ¯BP. Contraindications: fetal distress, severe pre-eclampsia, APH, hypotension, tachycardia, asthma, etc
§ Oral Nifedipine (Ca channel blocker) is replacing Salbutamol – equal efficacy and ¯side effects.
§ If cervix is > 4cm then it should be allowed to progress – shouldn‟t
use tocolytics
§ ?Not if PROM (premature rupture of membranes). Can ® risk of infection
o Steroids: dexamethasone and betamethasone (crosses placenta, prednisone doesn‟t) - 2 shots 12 hours apart. Always give first even if close to delivery ® maturation of lungs if between 24 and 34 weeks (surfactant production ® ¯fetal distress syndrome) and neonatal better BP control post delivery
o Delivery. If < 26 weeks then vaginal delivery. C-section more likely
if multiple pregnancy or breech. Epidural analgesia preferable to narcotics (®
respiratory depression)
Premature Rupture of Membranes*
·
= Rupture of membranes before
labour is established. Normally rupture of membranes follows establishment of
labour
·
Check: have they really ruptured?
Look for pooled liquor in posterior fornix. Do US for liquor volume and fetal
well-being
·
Management:
o Admit and monitor
o Swabs for infection (a cause of PROM)
o Check for signs of infection: fever, maternal or fetal tachycardia, WBC
o After 24 hours (time varies) commence prophylactic antibiotics
o Low threshold for induction
Related Topics