Chapter: 11th Nutrition and Dietetics : Chapter 12 : Nutrition Intervention Programmes and Policies
Nutrition intervention programmes
NUTRITION INTERVENTION PROGRAMMES AND POLICIES
Nutrition is a major
factor in bringing out the maximum potential that one is endowed both
physically and mentally. Widespread malnutrition is largely a result of dietary
inadequacy and unhealthy lifestyles. The great advantages of looking at
malnutrition as a problem in human ecology is that it allows for variety of
approaches towards its prevention.
Nutrition intervention programmes
Integrated Child Development Services (ICDS)
ICDS was initiated in 1975 with the twin objectives of ensuring
nutrition of preschool children through supplementary feeding
and psychosocial development through early stimulation and education. The
objectives also include supplementary feeding for pregnant and lactating women
and nutrition education to ensure better child care and nutrition.
·
The nutrition components of ICDS aims to provide the following
services:
·
nutrition education to mothers for improving dietary intake and
dietary diversity.
·
nutrition education regarding appropriate infant and young child
feeding practices. growth monitoring and detection of growth faltering.
·
assist in providing massive doses of vitamin A, ORS and iron
tablets.
·
food supplementation to preschool children between the age of
six months and six years, pregnant and lactating mothers and selected
adolescent girls.
The Anganwadi workers are expected to survey all families in the community and identify all pregnant, lactating women and preschool children, monitor the growth of children and provide food supplement to the three groups for 300 days in a year. ICDS guidelines specify that monthly weighing of children should be done in the crucial 0-24 months age group.
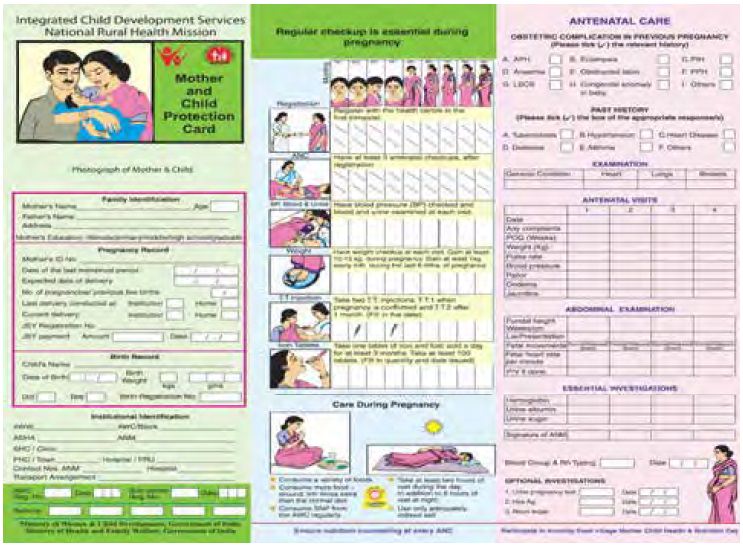
Mother and Child Protection card (MCP card) was introduced for functionaries of
National Rural Health Mission (NRHM) and ICDS from 1st April 2010 to
progressively replace the earlier JacchhaBacchha card. The new MCP card
is increasingly viewed as a critical tool for upkeeping maternal and child
health in the updated coverage of both ICDS and NRHM.
Midday meal programme (MDMP)
The midday meal
programme (MDMP) is also known as school lunch programme. This programme has
been in operation since 1961 throughout the country. In formulating midday
mealsforschoolchildren, thefollowing broad principles should be kept in mind:
·
The meal should be a supplement and not a substitute to the home
diet.
·
The meal should supply atleast one third of the total energy
requirement and half of the protein need.
·
cost of the meal should be reasonably low.
·
meal should be such that it can be prepared easily in
schools. No complicated cooking process should be involved.
·
As far as possible, locally available foods should be used. This
will reduce the cost of the meal.
·
meal should be frequently changed to avoid monotony.
Objectives
of
the
school
feeding programme are
to:
·
provide food for undernourished children and to improve the
nutritional status and monitor it.

·
increase school enrolment
and attendance of
children
·
reorient good eating habits.
·
incorporate nutrition education into curriculum.
·
improve literacy and educational performance of pupils.
·
encourage the use
of
local commodities.
·
encourage community participation in the feeding programme.
The Mid-Day Meal
Programme for school children comes under the Ministry of Human Development.
The Government of India pays 40 percent of the expenditure and 60 percent is
borne by the States. It covers all children upto the age of 15 years.
In Tamil Nadu, the
noon meal programme was launched on July 1st 1982 by the then Chief Minister
M.G.Ramachandran in rural areas and then extended to the urban areas. In this
programme, students from classes I to V in Corporation, Government and
Government aided schools are given free mid-day meal for 200 days in a year.
Under this programme, the Government of India provides 100 grams of rice, 15
gram of dhal, 1 grams of oil and 20 paise worth of vegetables per indiviual.
The meal given are based on a combination of cereals, pulses and leafy
vegetables. Eggs are given thrice a week. Such a diet would increase the amount
of vitamins and minerals and results in weight gain and clearance of deficiency
symptoms.
What do children eat
today in their midday meal :
·
Upto 5th standard, 100 grams of rice per child per
day
·
Upto 10th standard, 150 grams of rice per child per
day
·
Egg on all working days. Banana alternative for vegetarians.
·
First and third week of month, pulav made of black Bengal gram
given for protein
·
Second and fourth week, green gram sundal
·
Fridays, chilli fried
potato
for carbohydrates
·
Use of double fortified salt
·
Sweet pongal is served on occasions
Mid-Day meal programme
has resulted in the following:
·
Reduction in severe malnutrition in children.
·
Increased enrolment rate at primary level.
·
Reduction in drop-out rate at school level.
·
Developed attentiveness in them and thereby improved their power
of comprehension.
·
Improved their performance in examinations.
·
Decreased the incidence of various diseases and physical
disorders caused by starvation or intake of less nutritious food.
·
Enabled parents to attend to their routine bread earning tasks.
·
The gender difference in feeding the children reduced at home.
·
A favourable attitude in parents in educating the children,
specifically female children.
Prevention and control of anaemia
Prevention of anaemia
requires approaches that address all the potential causative factors. These
include:
1. Dietary approach: The following points
need to be considered for the promotion of this strategy:
·
Promotion of consumption of pulses, green leafy vegetables,
other vegetables which are rich in iron and folic acid and meat products rich
in iron particularly for pregnant and lactating mothers and preschool children.
Media can also be involved for creation of awareness.
·
Creation of awareness in mothers attending antenatal clinics,
immunization sessions, anganwadi centres and crèches about the prevalence of
anaemia, ill effects of anaemia and that it is preventable.
·
Addition of iron rich foods to the weaning foods of infants.
·
Regular consumption of foods rich in vitamin C to promote iron
absorption such as orange, guava, amla, etc.
·
Promotion of home gardening to increase the availability of
common iron rich foods such as green leafy vegetables.
·
Discouraging the consumption of foods and beverages like tea and
tamarind that inhibit iron absorption, immediately after food especially by the
vulnerable groups like pregnant women and children.
·
Promotion of iron fortified iodised salt.
2. Supplementation: Food based
approachesthroughfoodfortification and dietary diversification are sustainable
strategies for preventing iron deficiency and (Iodine Deficiency Disorder(IDD).
As availability is low and dietary animal sources (haem -iron) are expensive,
the key step towards addressing iron deficiency and IDD would be the
implementation and scaling up of the IFA supplementation programme.
For preventing
anaemia, low dosage iron is adequate. The National Anaemia Prophylaxis
Programme (NAPP) in India, pregnant and lactating women receive 60 mg elemental
iron+ 500 mcg folic acid (IFA tablet) daily for atleast 100 days
during pregnancy and preschool children receive 20 mg
elemental iron+ 100 mcg folic acid daily. To improve compliance,
ensuring availability to all beneficiaries, follow up of pregnant women through
ante natal care (ANC) for completion of therapy, counseling on common side
effects, risks associated with anaemia, provision of incentives to frontline
workforce, frequent evaluation to assess the programme, weekly or biweekly
administration of iron and folate and inclusion of adolescent as beneficiaries
are needed.
3. National Iron+
Initiative: Taking cognizance of ground realities in the operation of the
programme, Ministry of Health and Family Welfare took a policy decision to develop the National Iron+
Initiative. This initiative will bring together existing programmes (IFA
supplementation for pregnant and lactating women and children in
·
Biweekly iron supplementation for preschool children of 6 months
to 5 years.
·
Weekly supplementation for children from 1st to 5th grade in
Government and Government aided schools.
·
Weekly supplementation for out of school children (5-10 years)
at anganwadi centres.
·
Pregnant and lactating women, daily for 100 days.
·
Weekly supplementation for women in reproductive age group.

In addition to
increased iron and folate intake, improvement in environmental sanitation and
personal hygiene are also needed to control worm infestations and infections.
Deworming done regularly would help in reducing the incidence of anaemia and
improve the efficacy of iron supplements. An improvement in food intake results
in improvement in haemoglobin levels
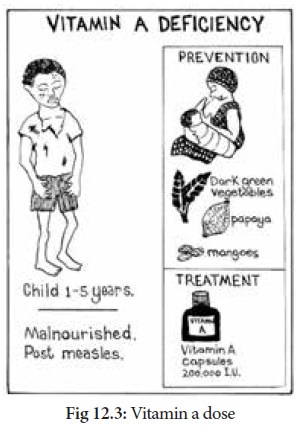
Prevention and control of vitamin A deficiency
1. Nutrition education
2. Dietary modification:
The most rational and sustainable long term solution to control of vitamin A
deficiency is to ensure that the community includes regularly, in their daily
diets, foods rich in vitamin A or its precursor.
3. Periodic
supplementation or dosing of vitamin A: Currently the massive dose of vitamin A
supplementation programme aims at providing the first dose of 1,00,000 IU at 9
months (at the time of measles immunization) to be followed by bi annual
administration of 2,00,000 IU for children between the ages of 18 months and 59
months. The coverage under massive dose vitamin A administration has improved
substantially
4. Fortification of
commonly and widely consumed foods with vitamin A: Fortification or enrichment
of widely consumed foods with vitamin A is another strategy toprevent and
control vitamin A deficiency. Foods which are consumed daily by all sections of
the community with little variation in the intake are generally utilized for
the fortification. Fortified foods are integrated into the conventional food
system as value added products to reach a large segment of population.
Related Topics