Chapter: Medical Surgical Nursing: Management of Patients With Cerebrovascular Disorders
Nursing Process: The Patient With a Hemorrhagic Stroke
NURSING PROCESS:THE PATIENT WITH AHEMORRHAGIC
STROKE
Assessment
A complete neurologic assessment is performed initially
and should include evaluation for the following:
·
Altered level of consciousness
·
Sluggish pupillary reaction
·
Motor and sensory dysfunction
·
Cranial nerve deficits
(extraocular eye movements, facial droop, presence of ptosis)
·
Speech difficulties and visual
disturbance
·
Headache and nuchal rigidity
or other neurologic deficits
All patients should be monitored in the intensive care
unit fol-lowing an intracerebral hemorrhage (Qureshi et al., 2001). Neu-rologic
assessment findings are documented and reported as indicated. The frequency of
these assessments varies depending on the patient’s condition. Any changes in
the patient’s condition require reassessment and thorough documentation;
changes should be reported immediately.
Alteration in level of consciousness often is the
earliest sign of deterioration in a patient with a hemorrhagic stroke. Because
nurses have the most frequent contact with patients, they are in the best
position to detect what may be subtle changes. Mild drowsiness and slight
slurring of speech may be early signs that the level of consciousness is
deteriorating. Frequent nursing as-sessment is crucial in the patient with
known or suspected cere-bral aneurysm.
Diagnosis
NURSING DIAGNOSES
Based on the assessment data, the patient’s major nursing
diag-noses may include the following:
·
Ineffective cerebral tissue
perfusion related to bleeding
·
Disturbed sensory perception
related to medically imposed restrictions (aneurysm precautions)
·
Anxiety related to illness
and/or medically imposed restric-tions (aneurysm precautions)
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based on the assessment data, potential complications
that may develop include the following:
·
Vasospasm
·
Seizures
·
Hydrocephalus
·
Rebleeding
Planning and Goals
The goals for the patient may include improved cerebral
tissue perfusion, relief of sensory and perceptual deprivation, relief of
anxiety, and the absence of complications.
Nursing Interventions
OPTIMIZING CEREBRAL TISSUE PERFUSION
The patient is closely
monitored for neurologic deterioration oc-curring from recurrent bleeding,
increasing ICP, or vasospasm. A neurologic flow record is maintained. The blood
pressure, pulse, level of responsiveness (an indicator of cerebral perfusion),
pupil-lary responses, and motor function are checked hourly. Respira-tory
status is monitored because a reduction in oxygen in areas of the brain with
impaired autoregulation increases the chances of a cerebral infarction. Any
changes are reported immediately.
Implementing Aneurysm Precautions
Cerebral aneurysm precautions are implemented for the
patient with a diagnosis of aneurysm to provide a nonstimulating envi-ronment,
prevent increases in ICP pressure, and prevent further bleeding. The patient is
placed on immediate and absolute bed rest in a quiet, nonstressful environment
because activity, pain, and anxiety elevate the blood pressure, which increases
the risk for bleeding. Visitors, except for family, are restricted.
The head of the bed is elevated 15 to 30 degrees to
promote venous drainage and decrease ICP. Some neurologists, however, prefer
that the patient remain flat to increase cerebral perfusion.
Any activity that suddenly increases the blood pressure
or ob-structs venous return is avoided. This includes the Valsalva ma-neuver, straining, forceful sneezing, pushing up
in bed, acute flexion or rotation of the head and neck (which compromises the
jugular veins), and cigarette smoking. Any activity requiring ex-ertion is
contraindicated. The patient is instructed to exhale through the mouth during
voiding or defecation to decrease strain. No enemas are permitted, but stool
softeners and mild lax-atives are prescribed. Both prevent constipation, which
would cause an increase in ICP, as would enemas. Dim lighting is help-ful
because photophobia (visual intolerance of light) is common. Coffee and tea,
unless decaffeinated, are usually eliminated.
Thigh-high elastic compression stockings or sequential
com-pression boots may be prescribed to decrease the incidence of deep vein
thrombosis resulting from immobility. The legs are ob-served for signs and
symptoms of deep vein thrombosis (tender-ness, swelling, warmth, discoloration,
positive Homans’ sign), and abnormal findings are reported.
The nurse administers all personal care. The patient is
fed and bathed to prevent any exertion that might raise the blood pres-sure.
External stimuli are kept to a minimum, including no tele-vision, no radio, and
no reading. Visitors are restricted in an effort to keep the patient as quiet
as possible. This precaution must be individualized based on the patient’s
condition and response to visitors. A sign indicating this restriction should
be placed on the door of the room, and the restrictions should be discussed
with both patient and family. The purpose of aneurysm precautions should be
thoroughly explained to both the patient (if possible) and family.
RELIEVING SENSORY DEPRIVATION AND ANXIETY
Sensory stimulation is kept to a minimum for patients on
aneurysm precautions. For patients who are awake, alert, and ori-ented, an
explanation of the restrictions helps reduce the patient’s sense of isolation.
Reality orientation is provided to help main-tain orientation.
Keeping the patient well informed of the plan of care
provides reassurance and helps minimize anxiety. Appropriate reassurance also
helps relieve the patient’s fears and anxiety. The family also requires
information and support.
MONITORING AND MANAGINGPOTENTIAL COMPLICATIONS
Vasospasm
The patient is assessed for signs of possible vasospasm:
intensified headaches, a decrease in level of responsiveness (confusion,
dis-orientation, lethargy), or evidence of aphasia or partial paralysis. These
signs may develop several days after surgery or on the ini-tiation of treatment
and must be reported immediately. If va-sospasm is diagnosed, calcium-channel blockers
or fluid volume expanders may be prescribed.
Seizures
Seizure precautions are
maintained for every patient who may be at risk for seizure activity. Should a
seizure occur, maintaining the airway and preventing injury are the primary
goals. Medicationtherapy is initiated at this time if not already prescribed.
The medication of choice is phenytoin (Dilantin) because this agent usually
provides adequate antiseizure action while causing no drowsiness at therapeutic
levels.
Hydrocephalus
Blood in the subarachnoid space impedes the circulation
of CSF, resulting in hydrocephalus. A CT scan that indicates dilated
ven-tricles confirms the diagnosis. Hydrocephalus can occur within the first 24
hours (acute) after subarachnoid hemorrhage or days (subacute) to several weeks
(delayed) later. Symptoms vary ac-cording to the time of onset and may be
nonspecific. Acute hydro-cephalus is characterized by sudden onset of stupor or
coma and is managed with a ventriculostomy drain to decrease ICP. Symptoms of
subacute and delayed hydrocephalus include gradual onset of drowsiness,
behavioral changes, and ataxic gait. A ventriculoperitoneal shunt is surgically
placed to treat chronic hydrocephalus. Changes in patient responsiveness are
reported immediately.
Rebleeding
The rate of recurrent hemorrhage is approximately 2%
following a primary intracerebral hemorrhage. Hypertension is the most se-rious
risk factor, suggesting the importance of appropriate anti-hypertensive
treatment (Qureshi et al., 2001).
Aneurysm rebleeding
occurs most frequently in the first 2 weeks after the initial hemorrhage and is
considered a major complica-tion. Symptoms of rebleeding include sudden severe
headache, nausea, vomiting, decreased level of consciousness, and neuro-logic
deficit. A CT scan is performed to confirm rebleeding. Blood pressure is
carefully maintained with medications. Antifibri-nolytic medications
(epsilon-aminocaproic acid) may be admin-istered to delay the lysis of the clot
surrounding the rupture. The most effective preventive treatment is early
clipping of the aneurysm if the patient is a candidate for surgery.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
The patient and family
are provided with information that will enable them to cooperate with the care
and restrictions required during the acute phase of hemorrhagic stroke and to
prepare them to return home. Patient and family teaching includes informa-tion
about the causes of hemorrhagic stroke and its possible con-sequences. In
addition, the patient and family are informed about the medical treatments that
are implemented, including surgical intervention if warranted, and the
importance of interventions taken to prevent and detect complications (ie,
aneurysm precau-tions, close monitoring of the patient). Depending on the
presence and severity of neurologic impairment and other complications
resulting from the stroke, the patient may be transferred to a re-habilitation
unit or center, where additional patient and family teaching will focus on strategies
to regain ability to manage self-care. Teaching may also address the use of
assistive devices or modification of the home environment to help the patient
live with a disability. Modifications of the home may be required to provide a
safe environment (Olson, 2001). (See Nursing Research Profile 62-2.)
Continuing Care
During the acute and rehabilitation phase of care for the patient with a hemorrhagic stroke, the focus is on obvious needs, issues, and deficits. The patient and family are reminded of the importance of following recommendations to prevent further hemor-rhagic stroke and keeping follow-up appointments with health care providers for monitoring.
Referral for home care
may be warranted to assess the home environment and the ability of the patient
and to ensure that the patient and family are able to manage at home. The
physical and psychological status of the patient and ability of the family to
cope with any alterations in the patient’s status are monitored during home
visits. In addition, the nurse involved in home and continuing care needs to
remind patients and family members of the need for continuing health promotion
and screen-ing practices. Patients who have not been involved in these
practices in the past are educated about their importance and are referred to
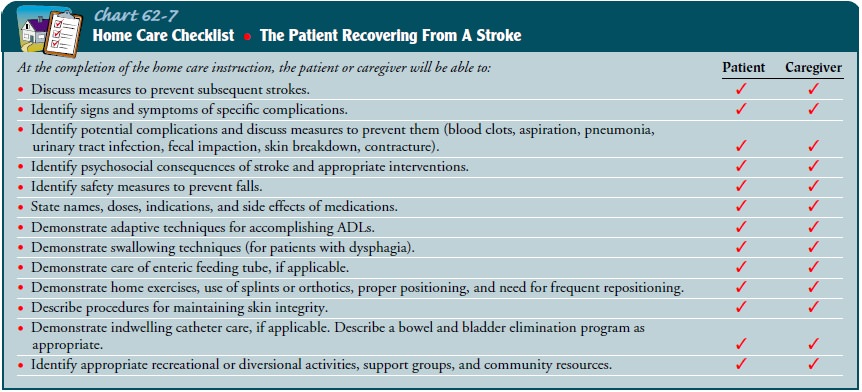
appropriate health care providers, if indicated. Chart 62-7 lists teaching
points for the patient recovering from a stroke.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected patient outcomes may include:
1) Demonstrates intact neurologic status and normal vital signs and respiratory patterns
a) Is
alert and oriented to time, place, and person
b) Demonstrates
normal speech patterns and intact cogni-tive processes
c) Demonstrates
normal and equal strength, movement, and sensation of all four extremities
d) Exhibits
normal deep tendon reflexes and pupillary re-sponses
2) Demonstrates
normal sensory perceptions
a) States
rationale for aneurysm precautions
b) Exhibits
clear thought processes
3) Exhibits
reduced anxiety level
a) Is
less restless
b) Exhibits
absence of physiologic indicators of anxiety (eg, normal vital signs; normal
respiratory rate; absence of excessive, fast speech)
4) Is
free of complications
a) Exhibits
absence of vasospasm
b) Exhibits
normal vital signs and neuromuscular activity without seizures
c) Verbalizes
understanding of seizure precautions
d) Exhibits
normal mental status and normal motor and sensory status
5) Reports
no visual changes
Related Topics