Chapter: Medical Surgical Nursing: Management of Patients With Coronary Vascular Disorders
Nursing Process: The Patient With Myocardial Infarction
NURSING PROCESS: THE PATIENT WITH MYOCARDIAL INFARCTION
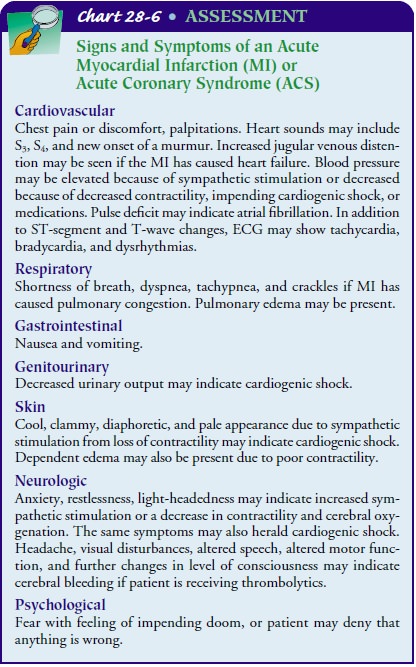
Assessment
One
of the most important aspects of care of the patient with an MI is the
assessment. It establishes the baseline for the patient so that any deviations
may be identified, systematically identifies the patient’s needs, and helps
determine the priority of those needs. Systematic assessment includes a careful
history, particularly as it relates to symptoms: chest pain or discomfort,
difficulty breathing (dyspnea), palpitations, unusual fatigue, faintness
(syncope), or sweating (diaphoresis). Each symptom must be evaluated with
re-gard to time, duration, the factors that precipitate the symptom and relieve
it, and comparison with previous symptoms. A precise and complete physical
assessment is critical to detect complica-tions and any change in patient
status. Chart 28-6 identifies im-portant assessments and possible findings.
Intravenous
sites are examined frequently. At least one and possibly two intravenous lines
are placed for any patient with ACS to ensure that access is available for
administering emergency med-ications. Medications are administered
intravenously to achieve rapid onset and to allow for timely adjustment.
Intramuscular medications are avoided because of unpredictable absorption,
de-layed effect, and the risk of causing elevated serum enzyme levels by
injuring muscle cells with an injection. After the patient’s con-dition
stabilizes, the intravenous line may be changed into a saline lock to maintain
intravenous access.
Diagnosis
NURSING DIAGNOSES
Based
on the clinical manifestations, history, and diagnostic assessment data, the
patient’s major nursing diagnoses may include:
·
Ineffective cardiopulmonary tissue
perfusion related to re-duced coronary blood flow from coronary thrombus and
atherosclerotic plaque
·
Potential impaired gas exchange
related to fluid overload from left ventricular dysfunction
·
Potential altered peripheral tissue
perfusion related to de-creased cardiac output from left ventricular
dysfunction
·
Anxiety related to fear of death
·
Deficient knowledge about post-MI
self-care
COLLABORATIVE PROBLEMS/ POTENTIAL COMPLICATIONS
Based
on the assessment data, potential complications that may develop include the
following:
·
Acute pulmonary edema
·
Heart failure
·
Cardiogenic shock
·
Dysrhythmias and cardiac arrest
·
Pericardial effusion and cardiac
tamponade
·
Myocardial rupture
Planning and Goals
The
major goals of the patient include relief of pain or ischemic signs and
symptoms (eg, ST-segment changes), prevention of further myocardial damage,
absence of respiratory dysfunction, maintenance or attainment of adequate
tissue perfusion by de-creasing the heart’s workload, reduced anxiety,
adherence to the self-care program, and absence or early recognition of
complica-tions.
Nursing Interventions
RELIEVING PAIN AND OTHER SIGNS AND SYMPTOMS OF ISCHEMIA
Balancing
the cardiac oxygen supply with its oxygen demand (eg, as evidenced by the
relief of chest pain) is the top priority for the patient with an acute MI.
Although medication therapy is re-quired to accomplish this goal, nursing
interventions are also im-portant. Collaboration among the patient, nurse, and
physician is critical in assessing the patient’s response to therapy and in
al-tering the interventions accordingly.
The
accepted method for relieving symptoms associated with MI is revascularization
with thrombolytic therapy or emergent PCI for patients who present to the
health care facility immedi-ately and who have no major contraindications.
These therapies are important because, in addition to relieving symptoms, they
aid in minimizing or avoiding permanent injury to the myo-cardium. With or
without revascularization, administration of as-pirin, intravenous
beta-blocker, and nitroglycerin is indicated. Use of a GPIIb/IIIa agent or
heparin may also be indicated. The nurse administers morphine for relief of pain
and other symp-toms, anxiety, and reduction of preload.
Oxygen
should be administered along with medication therapy to assist with relief of
symptoms. Administration of oxygen even in low doses raises the circulating
level of oxygen to reduce pain asso-ciated with low levels of myocardial
oxygen. The route of admin-istration, usually by nasal cannula, and the oxygen
flow rate are documented. A flow rate of 2 to 4 L/min is usually adequate to
maintain oxygen saturation levels of 96% to 100% if no other dis-ease is
present.
Vital
signs are assessed frequently as long as the patient is expe-riencing pain and
other signs or symptoms of acute ischemia. Phys-ical rest in bed with the
backrest elevated or in a cardiac chair helps to decrease chest discomfort and
dyspnea. Elevation of the head is beneficial for the following reasons:
·
Tidal volume improves because of
reduced pressure from abdominal contents on the diaphragm and better lung
ex-pansion and gas exchange.
·
Drainage of the upper lung lobes
improves.
·
Venous return to the heart (preload)
decreases, which re-duces the work of the heart.
IMPROVING RESPIRATORY FUNCTION
Regular
and careful assessment of respiratory function can help the nurse detect early
signs of pulmonary complications. Scrupu-lous attention to fluid volume status
prevents overloading the heart and lungs. Encouraging the patient to breathe
deeply and change position frequently helps keep fluid from pooling in the
bases of the lungs.
PROMOTING ADEQUATE TISSUE PERFUSION
Limiting the patient to bed or chair
rest during the initial phase of treatment is particularly helpful in reducing
myocardial oxygen consumption (mVO2). This limitation should remain
until the patient is pain-free and hemodynamically stable. Checking skin
temperature and peripheral pulses frequently is important to ensure adequate
tissue perfusion. Oxygen may be administered to enrich the supply of
circulating oxygen.
REDUCING ANXIETY
Alleviating
anxiety and fears is an important nursing function to reduce the sympathetic
stress response. Decreased sympa-thetic stimulation decreases the workload of
the heart, which may relieve pain and other signs and symptoms of ischemia.
Developing
a trusting and caring relationship with the patient is critical in reducing
anxiety. Providing information to the pa-tient and family in an honest and
supportive manner invites the patient to be a partner in care and greatly
assists in developing a positive relationship. Ensuring a quiet environment,
preventing interruptions that disturb sleep, using a caring and appropriate
touch, teaching the patient the relaxation response, using humor and assisting
the patient to laugh, and providing the appropriate prayer book and assisting
the patient to pray if consistent with the patient’s beliefs are other nursing
interventions that can be used to reduce anxiety. Frequent opportunities are
provided for the pa-tient to privately share concerns and fears. An atmosphere
of ac-ceptance helps the patient to know that these concerns and fears are both
realistic and normal. Music therapy, in which the patient listens to selected
music for a predetermined duration and at a set time, has been found to be an
effective method for reducing anx-iety and managing stress (Chlan & Tracy,
1999; Evans, 2002). Pet therapy, in which animals are brought to the patient,
appears to provide emotional support and reduce anxiety. Administrative and
infectious control practitioners are usually involved in devel-oping standards
for the animals, animal handlers, and patients who are eligible for pet
therapy.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Complications that can occur after acute MI are caused by the
dam-age that occurs to the myocardium and to the conduction system as a result
of the reduced coronary blood flow. Because these com-plications can be lethal,
close monitoring for and early identifica-tion of the signs and symptoms is
critical.
The
nurse monitors the patient closely for changes in cardiac rate and rhythm,
heart sounds, blood pressure, chest pain, respi-ratory status, urinary output,
skin color and temperature, senso-rium, ECG changes, and laboratory values. Any
changes in the patient’s condition are reported promptly to the physician, and
emergency measures are instituted when necessary.
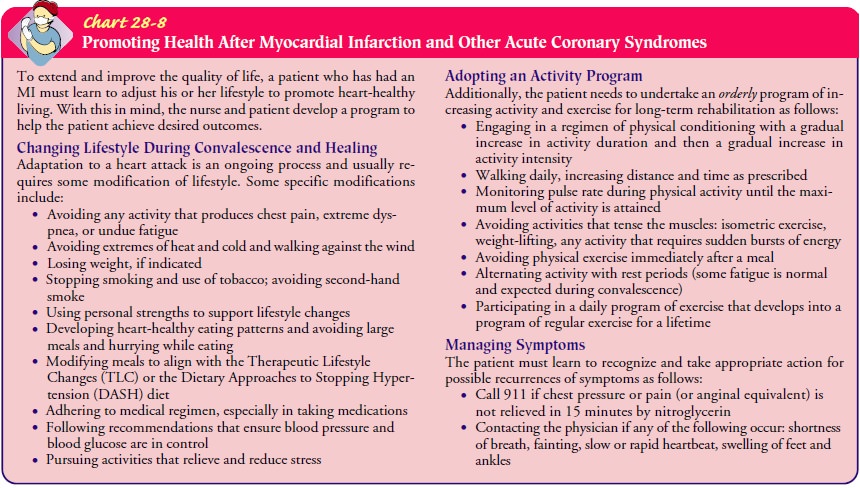
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
The most effective way to increase the probability the patient will implement a self-care regimen after discharge is to identify the priorities as perceived by the patient, provide adequate education about heart-healthy living, and facilitate the patient’s involve-ment in a cardiac rehabilitation program. Working with patients in developing plans to meet their specific needs further enhances the potential for an effective treatment plan (Chart 28-8).
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include the following:
·
Relief of angina
·
No signs of respiratory difficulties
·
Adequate tissue perfusion
·
Decreased anxiety
·
Adherence to a self-care program
·
Absence of complications
Related Topics