Chapter: Medical Surgical Nursing: Intraoperative Nursing Management
Nursing Process: The Patient During Surgery
NURSING PROCESS: THE PATIENT DURING SURGERY
The
Perioperative Nursing Data Set (PNDS) is a helpful model used by nurses in the
intraoperative phase of care. Phenomena of concern to intraoperative nurses are
nursing diagnoses, interventions, and outcomes that surgical pa-tients and
their families experience. Additional areas of concern include collaborative
problems and expected goals.
Assessment
Nursing
assessment of the intraoperative patient involves obtain-ing data from the
patient and the patient’s record to identify vari-ables that can affect care
and serve as guidelines for developing an individualized plan of patient care.
The intraoperative nurse uses the focused preoperative nursing assessment
documented on the patient record. This includes assessment of physiologic
status (eg, health–illness level, level of consciousness), psychosocial sta-tus
(eg, anxiety level, verbal communication problems, coping mechanisms), physical
status (eg, surgical site, skin condition and effectiveness of preparation;
immobile joints), and ethical con-cerns (Chart 19-3).
Diagnosis
NURSING DIAGNOSES
Based on the assessment data, some major nursing diagnoses may include the following:
• Anxiety related to expressed concerns due to surgery or OR environment
• Risk for perioperative positioning injury related to envi-ronmental conditions in the OR
• Risk for injury related to anesthesia and surgery
• Disturbed sensory perception (global) related to general anesthesia or sedation
COLLABORATIVE PROBLEMS/ POTENTIAL COMPLICATIONS
Based on the assessment data, potential complications may in-clude the following:
• Nausea and vomiting
• Anaphylaxis
• Hypoxia
• Unintentional hypothermia
• Malignant hyperthermia
• Disseminated intravascular coagulopathy
• Infection
Planning and Goals
Goals
for care of the patient during surgery include reducing anx-iety, preventing
positioning injuries, maintaining safety, main-taining the patient’s dignity,
and avoiding complications.
Nursing Interventions
REDUCING ANXIETY
The
OR environment can seem cold, stark, and frightening to the patient, who may be
feeling isolated and apprehensive. Intro-ducing yourself, addressing the
patient by name warmly and frequently, verifying details, providing
explanations, and encour-aging and answering questions provide a sense of
professionalism and friendliness that can help the patient feel secure. When
dis-cussing what the patient can expect in surgery, the nurse uses common,
basic communication skills, such as touch and eye con-tact, to reduce anxiety.
Attention to physical comfort (warm blankets, position changes) helps the
patient feel more comfort-able. Telling the patient who else will be present in
the OR, how long the procedure is expected to take, and other details helps the
patient prepare for the experience and gain a sense of control.
PREVENTING INTRAOPERATIVE POSITIONING INJURY
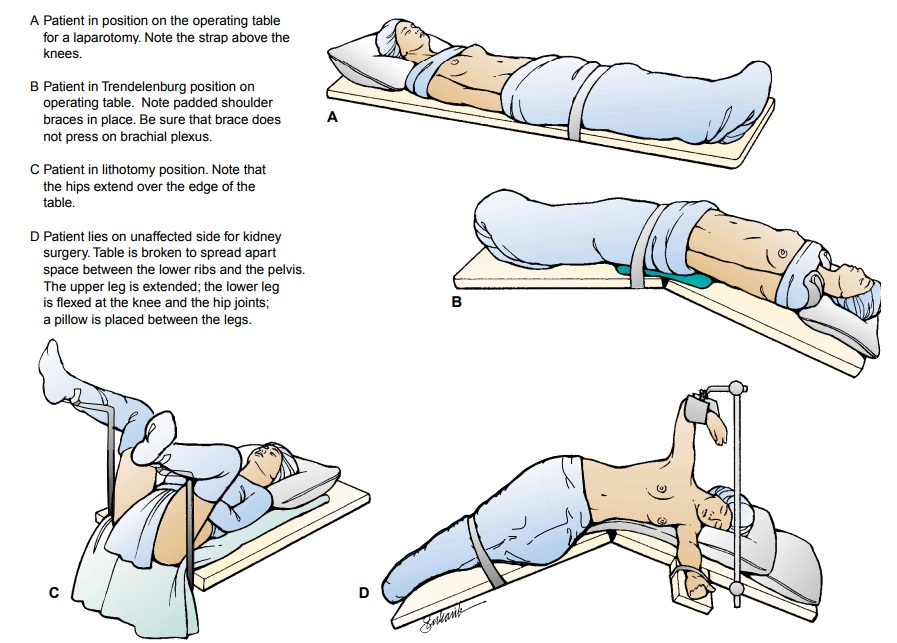
The
patient’s position on the operating table depends on the sur-gical procedure to
be performed as well as on his or her physical condition (Fig. 19-3). The
potential for transient discomfort or even permanent injury is clear because
many positions are awk-ward. Hyperextending joints, compressing arteries, or
pressing on nerves and bony prominences usually results in discomfort simply
because the position must be sustained for a long period (MeekerRothrock, 1999). Factors to consider
include the following:
The patient should be in as
comfortable a position as possi-ble, whether asleep or awake.
·
The operative field must be
adequately exposed.
·
An awkward position, undue pressure
on a body part, or use of stirrups or traction should not obstruct the vascular
supply.
· Respiration should not be impeded by
pressure of arms on the chest or by a gown that constricts the neck or chest.
· Nerves must be protected from undue
pressure. Improper positioning of the arms, hands, legs, or feet may cause
seri-ous injury or paralysis. Shoulder braces must be well padded to prevent
irreparable nerve injury, especially when the Trendelenburg position is
necessary.
·
Precautions for patient safety must
be observed, particularly with thin, elderly, or obese patients, or those with
a physi-cal deformity (Curet, 2000).
·
The patient needs gentle restraint
before induction in case of excitement.
The
Trendelenburg position usually is used for surgery on the lower abdomen and
pelvis to obtain good exposure by displacing the intestines into the upper
abdomen. In this position, the head and body are lowered. The patient is held
in position by padded shoulder braces (see Fig. 19-3B).
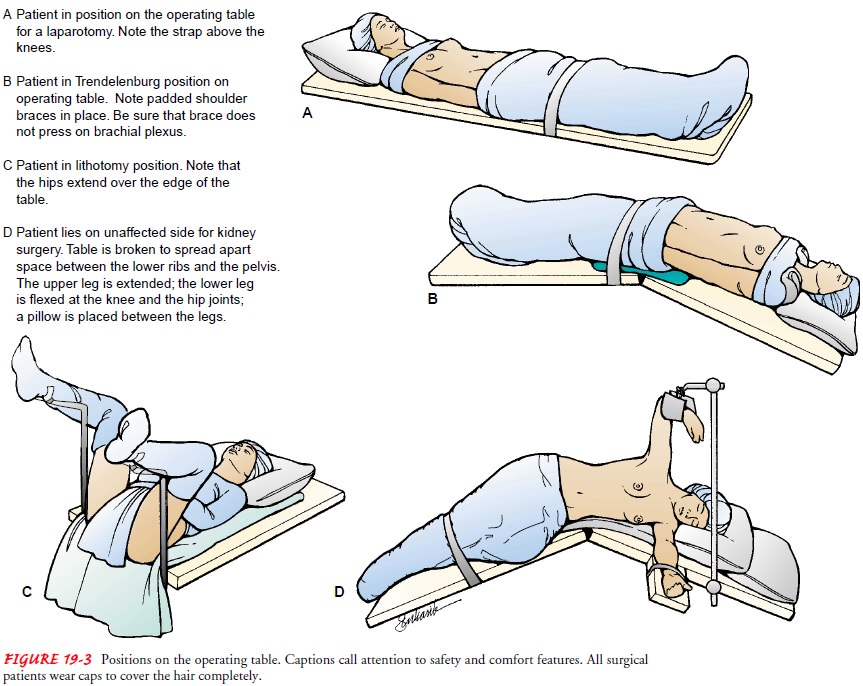
The
lithotomy position is used for nearly all perineal, rectal, and vaginal surgical
procedures (see Fig. 19-3C ). The
patient is positioned on the back with the legs and thighs flexed. The
posi-tion is maintained by placing the feet in stirrups.
The
Sims or lateral position is used for renal surgery. The pa-tient is placed on
the nonoperative side with an air pillow 12.5 to 15 cm (5 to 6 inches) thick
under the loin, or on a table with a kidney or back lift (see Fig. 19-3D).
Other
procedures, such as neurosurgery or abdominothoracic surgery, may require
unique positioning and supplemental appa-ratus, depending on the operative
approach.
PROTECTING THE PATIENT FROM INJURY
One
way the nurse protects the patient from injury is by provid-ing a safe
environment. A variety of activities are used to address the diverse patient
safety issues that arise in the OR. Verifying in-formation, checking the chart
for completeness, and maintaining surgical asepsis and an optimal environment
are critical nursing responsibilities. Verifying that all required
documentation is completed is one of the first functions of the intraoperative
nurse. The patient is identified, and the planned surgical procedure and type
of anesthesia are verified. It is important to review the pa-tient’s record for
the following:
·
Correct informed surgical consent,
with patient’s signature
·
Completed records for health history
and physical exami-nation
·
Results of diagnostic studies
·
Allergies (including latex)
In
addition to checking that all necessary patient data are complete, the
perioperative nurse obtains the necessary equip-ment specific to the procedure.
The need for nonroutine med-ications, blood components, instruments, and other
equipment and supplies is assessed, and the readiness of the room,
com-pleteness of physical setup, and completeness of instrument, su-ture, and dressing
setups are determined. Any aspects of the OR environment that may negatively
affect the patient are identified. These include physical features, such as
room temperature and humidity; electrical hazards; potential contaminants
(dust, blood, and discharge on floor or surfaces, uncovered hair, faulty attire
of personnel, jewelry worn by personnel); and unnecessary traffic. The
circulating nurse also sets up and maintains suction equip-ment in working
order, sets up invasive monitoring equipment, assists with insertion of
vascular access and monitoring devices (arterial, Swan-Ganz, central venous
pressure, intravenous lines), and initiates appropriate physical comfort
measures for the patient.
Preventing
physical injury includes using safety straps and bed rails and not leaving the
sedated patient unattended. Transferring the patient from the stretcher to the
OR table requires safe trans-ferring practices. Other safety measures include
properly posi-tioning the grounding pad under the patient to prevent electrical
burns and shock, removing excess povidone-iodine (Betadine) or other surgical
germicide from the patient’s skin, and promptly and completely draping exposed
areas after the sterile field has been created to decrease the risk for
hypothermia.
Nursing
measures to prevent injury from excessive blood loss include blood conservation
using equipment such a cell-saver (a device for recirculating the patient’s own
blood cells) or the ad-ministration of blood products (Finkelmeier, 2000). Few
patients undergoing an elective procedure require blood transfusion, but those
undergoing higher-risk procedures (such as orthopedic or cardiac surgeries) may
require an intraoperative transfusion. The circulating nurse should anticipate
this need, check that blood has been cross-matched and held in reserve, and be
prepared to administer blood (Meeker & Rothrock, 1999).
SERVING AS PATIENT ADVOCATE
Because
the patient undergoing general anesthesia or moderate sedation experiences
temporary sensory/perceptual alteration or loss, he or she has an increased
need for protection and advo-cacy. Patient advocacy in the OR entails
maintaining the pa-tient’s physical and emotional comfort, privacy, rights, and
dignity. Patients, whether conscious or not, should not be sub-jected to excess
noise, inappropriate conversation, or, most of all, derogatory comments. As
surprising as this sounds, banter in the OR occasionally includes jokes about
the patient’s phys-ical appearance, job, personal history, and so forth. Cases
have been reported in which seemingly deeply anesthetized patients recalled the
entire surgical experience, including disparaging personal remarks made by OR
personnel. As an advocate, the nurse never engages in this conversation and
discourages others from doing so. Other advocacy activities include correcting
for the clinical, dehumanizing aspects of being a surgical patient by making
sure the patient is treated as a person, respecting cultural and spiritual
values, providing physical privacy, and maintaining confidentiality.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
It
is the responsibility of the surgeon and the anesthetist or anes-thesiologist
to monitor and manage complications. However, in-traoperative nurses also play
an important role. Being alert to and reporting changes in vital signs and
symptoms of nausea and vomiting, anaphylaxis, hypoxia, hypothermia, malignant
hyper-thermia, or disseminated vascular coagulation and assisting with their
management are important nursing functions (Dice, 2000; Fortunato-Phillips,
2000). Each of these complications was dis-cussed earlier. Maintaining asepsis
and preventing infection is the responsibility of all members of the surgical
team.
Evaluation
EXPECTED PATIENT OUTCOMES
·
Exhibits low level of anxiety
·
Remains free of perioperative
positioning injury
·
Experiences no unexpected threats to
safety
·
Has dignity preserved throughout OR
experience
Related Topics