Chapter: Medical Surgical Nursing: Management of Patients With Dermatologic Problems
Nursing Process: Care of the Patient With Malignant Melanoma
NURSING PROCESS:CARE OF THE PATIENT WITH MALIGNANT
MELANOMA
Assessment
Assessment
of the patient with malignant melanoma is based on the patient’s history and
symptoms. The patient is asked specifi-cally about pruritus, tenderness, and
pain, which are not features of a benign nevus. The patient is also questioned
about changes in preexisting moles or the development of new, pigmented
le-sions. People at risk are assessed carefully.
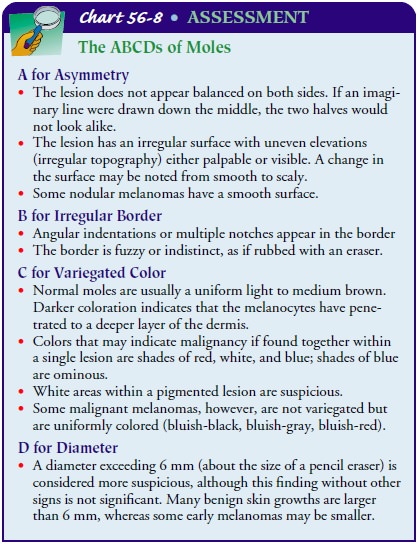
A
magnifying lens and good lighting are needed for inspect-ing the skin for
irregularity and changes in the mole. Signs that suggest malignant changes are
referred to as the ABCDs of moles (Chart 56-8).
Common
sites of melanomas are the skin of the back, the legs (especially in women),
between the toes, and on the feet, face, scalp, fingernails, and backs of
hands. In dark-skinned people, melanomas are most likely to occur in less
pigmented sites: palms, soles, subungual areas, and mucous membranes. Satellite
lesions (ie, those situated near the mole) are inspected.
Diagnosis
NURSING DIAGNOSES
Based on the nursing assessment data, the patient’s major nurs-ing diagnoses may include the following:
·
Acute pain related to surgical
excision and grafting
·
Anxiety and depression related
to possible life-threatening consequences of melanoma and disfigurement
·
Deficient knowledge about
early signs of melanoma
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based
on the assessment data, potential complications include the following:
·
Metastasis
·
Infection of the surgical site
Planning and Goals
The
major goals for the patient may include relief of pain and dis-comfort, reduced
anxiety and depression, knowledge of early signs of melanoma, and absence of
complications.
Nursing Interventions
RELIEVING PAIN AND DISCOMFORT
Surgical
removal of melanoma in different locations (eg, head, neck, eye, trunk,
abdomen, extremities, central nervous system) presents different challenges,
taking into consideration the re-moval of the primary melanoma, the intervening
lymphatic vessels, and the lymph nodes to which metastases may spread.
Nursing intervention after surgery for a malignant
melanoma centers on promoting comfort, because wide excision surgery may be
necessary. A split-thickness or full-thickness skin graft may be necessary when
large defects are created by surgical removal ofa melanoma. Anticipating the
need for and administering appro-priate analgesic medications are important.
REDUCING ANXIETY AND DEPRESSION
Psychological support is essential when disfiguring
surgery is per-formed. Support includes allowing patients to express feelings
about the seriousness of this cutaneous neoplasm, understanding their anger and
depression, and conveying understanding of these feelings. During the
diagnostic workup and staging of the depth, type, and extent of the tumor, the
nurse answers questions, clar-ifies information, and helps clarify
misconceptions. Learning that they have a melanoma can cause patients
considerable fear and anguish. Pointing out patients’ resources, past effective
coping mechanisms, and social support systems helps them to cope with the
problems associated with diagnosis, treatment, and continuing follow-up. The
patient’s family should be included in all discus-sions to clarify the
information presented, ask questions that the patient might be reluctant to
ask, and provide emotional support.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Metastasis
The
prognosis for malignant melanoma is related to metastasis: the deeper and
thicker (more than 4 mm) the melanoma, the greater is the likelihood of
metastasis. If the melanoma is grow-ing radially (ie, horizontally) and is
characterized by peripheral growth with minimal or no dermal invasion, the
prognosis is fa-vorable. When the melanoma progresses to the vertical growth
phase (ie, dermal invasion), the prognosis is poor. Lesions with ulceration
have a poor prognosis. Melanomas of the trunk appear to have a poorer prognosis
than those of other sites, perhaps be-cause the network of lymphatics in the
trunk permits metastasis to regional lymph nodes.
The
role of the nurse in caring for the patient with metastatic disease is
holistic. The nurse must be knowledgeable about the most effective current
therapies and must deliver supportive care, provide and clarify information
about the therapy and the ratio-nale for its use, identify potential side
effects of therapy and ways to manage them, and instruct the patient and family
about the expected outcomes of treatment. The nurse monitors and docu-ments
symptoms that may indicate metastasis: lung (eg, difficulty breathing,
shortness of breath, increasing cough), bone (eg, pain, decreased mobility and
function, pathologic fractures), and liver (eg, change in liver enzyme levels,
pain, jaundice). Nursing care is based on the patient’s symptoms.
Although the chance of a cure for malignant
melanoma that has metastasized is poor, the nurse encourages the patient to
have hope in the therapy employed while maintaining a realistic per-spective
about the disease and ultimate outcome. Moreover, the nurse provides time for
the patient to express fears and concerns regarding future activities and
relationships, offers information about support groups and contact people, and
arranges palliative and hospice care if appropriate.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
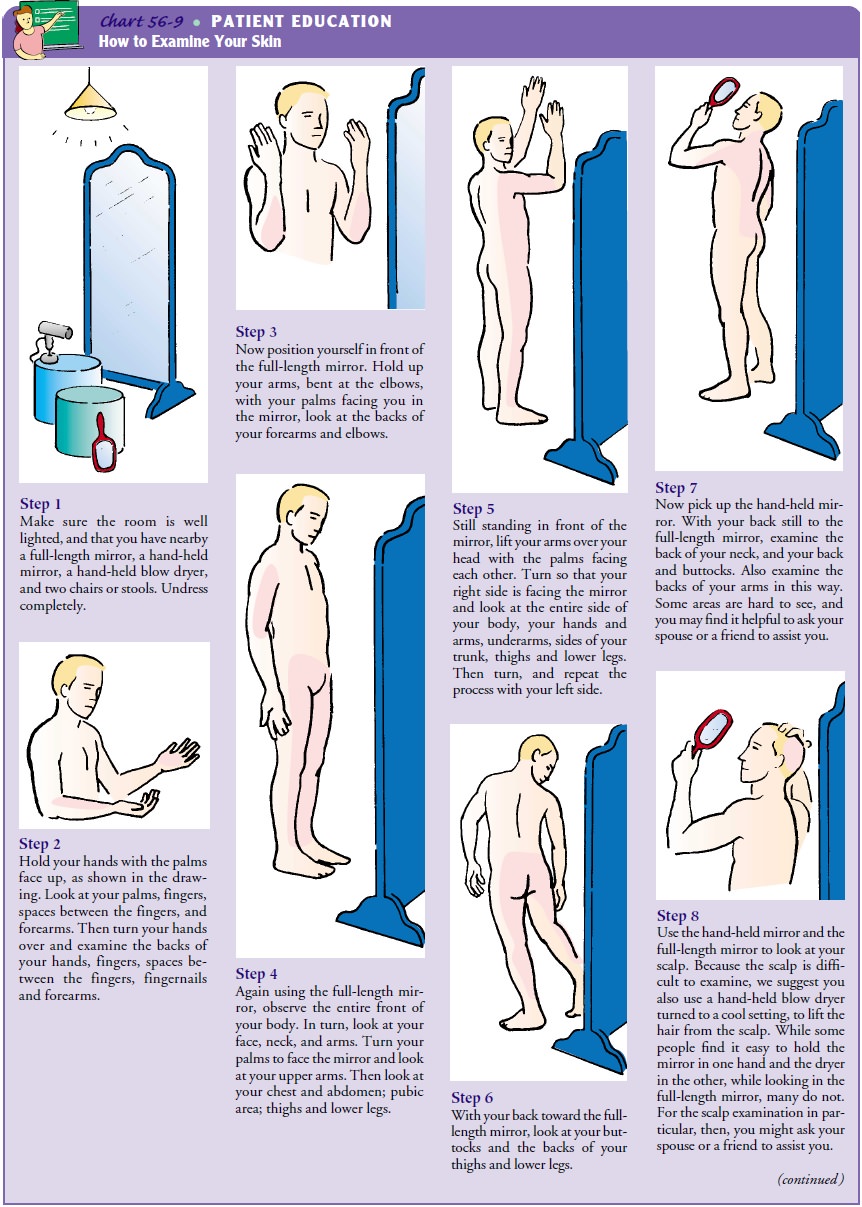
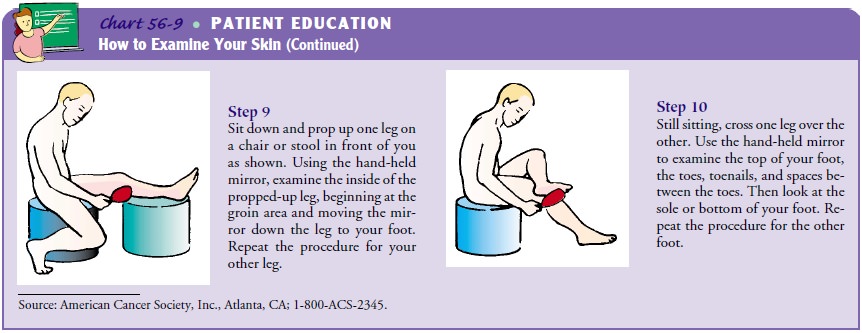
The best hope of controlling the disease lies in educating patients about the early signs of melanoma. Patients at risk are taught to examine their skin and scalp monthly in a systematic manner (Chart 56-9). The nurse also points out that a key factor in the development of malignant melanoma is exposure to sunlight. Be-cause melanoma is thought to be genetically linked, the family and the patient should be taught sun-avoiding measures.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include the following:
1) Experiences
relief of pain and discomfort
a) States
pain is diminishing
b) Exhibits
healing of surgical scar without heat, redness, or swelling
2) Is
less anxious
a) Expresses
fears and fantasies
b) Asks
questions about medical condition
c) Requests
repetition of facts about melanoma
d) Identifies
support and comfort provided by family member or significant other
3) Demonstrates
understanding of the means for detecting and preventing melanoma
a) Demonstrates
how to conduct self-examination of skin on a monthly basis
b) Verbalizes
the following danger signals of melanoma: change in size, color, shape, or
outline of mole, mole surface, or skin around mole
c) Identifies
measures to protect self from exposure to sun-light
4) Experiences
absence of complications
a) Recognizes
abnormal signs and symptoms that should be reported to physician
b) Complies
with recommended follow-up procedures and prevention strategies
Related Topics