Chapter: Essentials of Anatomy and Physiology: Reproductive System
Menstrual Cycle
Menstrual Cycle
The term menstrual (men′ stroo-ăl) cycle refers to the series of changes that occur in sexually mature, nonpregnant females and that culminate in menses. Menses (men′ sēz; month) is a period of mild hemorrhage, during which part of the endometrium is sloughed and expelled from the uterus. Typically, the menstrual cycle is about 28 days long, although it can be as short as 18 days or as long as 40 days (figure 19.14 and table 19.3). The menstrual cycle results from the cyclical changes that occur in the endome-trium of the uterus. These changes, in turn, result from the cyclical changes that occur in the ovary and are controlled by the secretions of FSH and LH from the anterior pituitary gland.
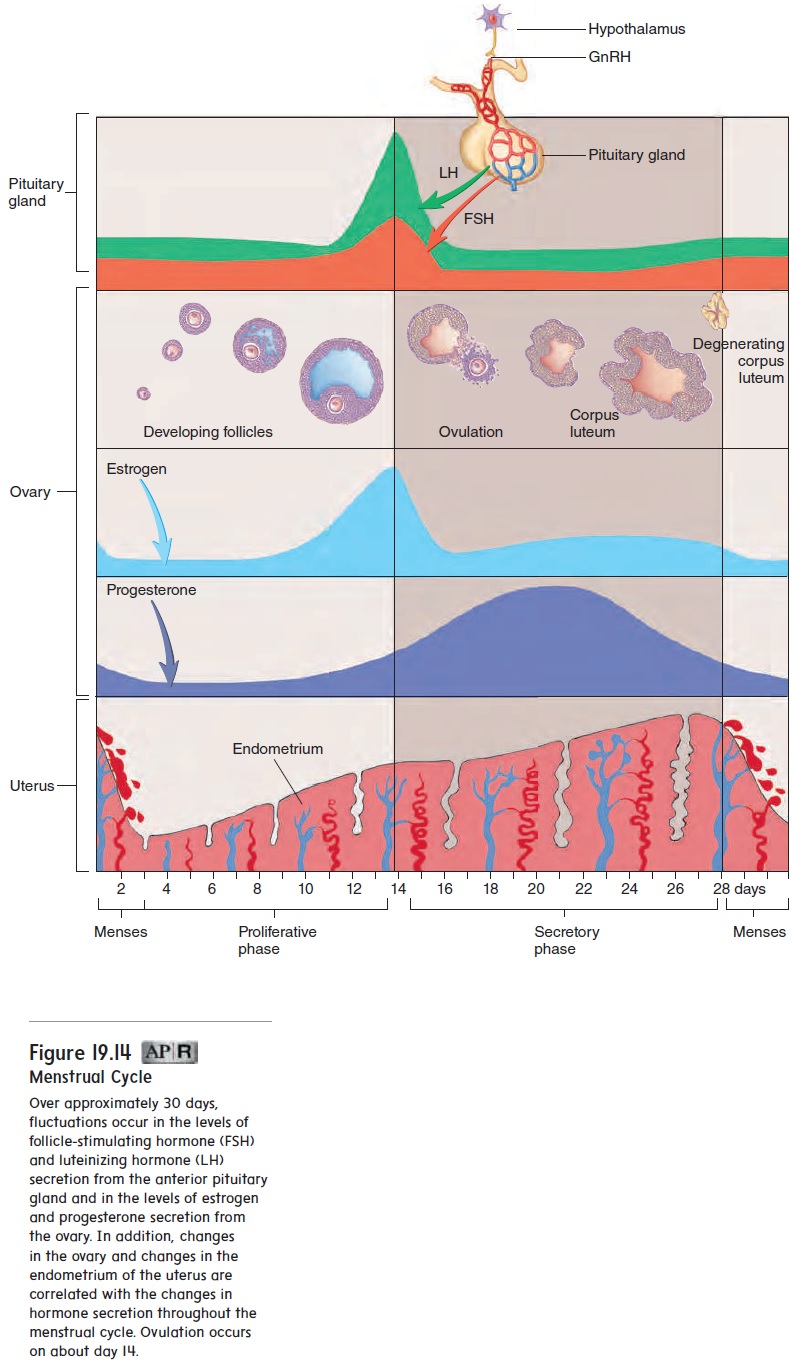
The first day of menstrual bleeding (menses), when the endo-metrium sloughs off, is considered day 1 of the menstrual cycle. Sloughing of the endometrium is inhibited by progesterone butstimulated by estrogen. Menses typically lasts 4 or 5 days and can be accompanied by strong uterine contractions, called men-strual cramps, that are extremely uncomfortable in some women. Menstrual cramps are the result of forceful myometrial contractions that occur before and during menstruation. The cramps can result from excessive secretion of prostaglandins. As the endometrium of the uterus sloughs off, it becomes inflamed, and prostaglandins are produced as part of the inflammation. Many women can alleviate painful cramps by taking medications, such as aspirin-like drugs, that inhibit prostaglandin biosynthesis just before the onset of menstruation. These medications, however, are not effective in treating all painful menstruation, especially when the cause of the pain, such as that experienced by women who have tumors of the myometrium, is not due to the inflammatory response.
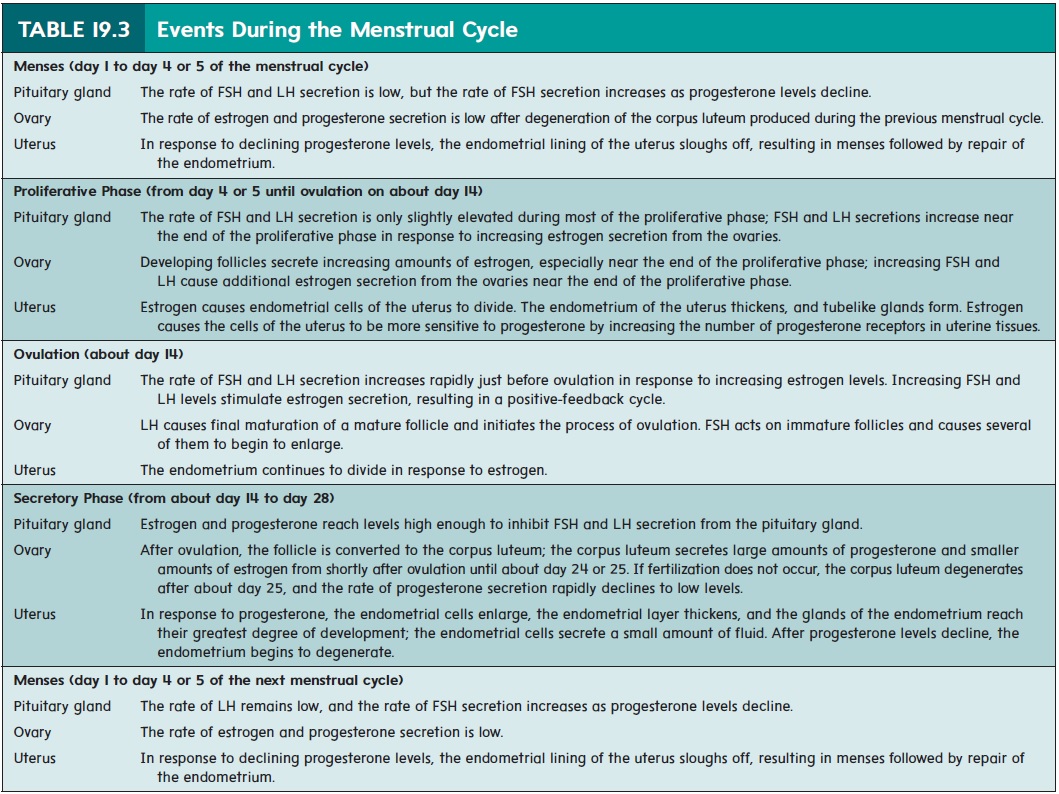
Ovulation occurs on about day 14 of the menstrual cycle, although the timing of ovulation varies from individual to individual and can vary within an individual from one menstrual cycle to the next. To avoid or optimize contraception, it is critical to predict ovulation; however, there is no single reliable method that can pre-dict its exact timing. The simplest method of predicting ovulation is looking for a drop in basal body temperature preceding ovulation, but it is the least reliable method.
Between the end of menses and ovulation is the proliferativephase, which refers to proliferation of the endometrium. During theproliferative phase, the secondary follicles in the ovary mature; as they do so, they secrete increasing amounts of estrogen. Estrogen acts on the uterus and causes the epithelial cells of the endometrium to divide rapidly. The endometrium thickens, and spiral glands form.
The sustained increase of estrogen secreted by the developing follicles stimulates GnRH secretion from the hypothalamus. GnRH, in turn, triggers FSH and LH secretion from the anterior pituitary gland. FSH stimulates estrogen secretion at an increasing rate from the developing follicles. This positive-feedback loop produces a series of larger and larger surges of FSH and LH secretion. Ovulation occurs in response to the large increases in LH levels that normally occur on about day 14 of the menstrual cycle. This large increase in LH is also responsible for the development of the corpus luteum.
Following ovulation, the corpus luteum begins to secrete pro-gesterone and smaller amounts of estrogen. Progesterone acts on the uterus, causing the cells of the endometrium to become larger and to secrete a small amount of fluid. Together, progesterone and estrogen act on the hypothalamus and anterior pituitary gland to inhibit GnRH, LH, and FSH secretion. Thus, LH and FSH levels decline after ovulation.
Between ovulation and the next menses is the secretoryphase of the menstrual cycle, called this because of the smallamount of fluid secreted by the cells of the endometrium. During the secretory phase, the lining of the uterus reaches its greatest degree of development.
By day 28, the declining pro-gesterone causes the endometrium to slough away to begin menses and the next menstrual cycle. The declining progesterone secretion results in a small increase in FSH secretion at the beginning of the next menses, which triggers more follicles to mature.
An ectopic pregnancy results if implantation occurs anywhere other than in the uterine cavity. The most common site of ectopic pregnancy is the uterine tube. Implantation in the uterine tube is even-tually fatal to the fetus and can cause the tube to rupture. In some rare cases, implantation occurs in the mesenteries of the abdominal cav-ity; the fetus can develop normally but must be delivered by caesarean section. However, maternal mortality rates for abdominal pregnancies are significantly higher than for fallopian tube ectopic pregnancies.
Menopause
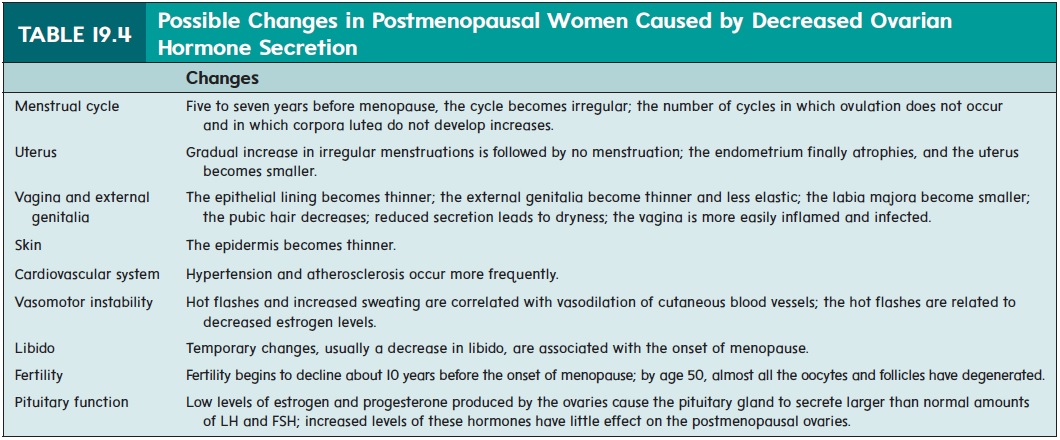
When a woman is 40–50 years old, the menstrual cycles become less regular, and ovulation does not occur consistently during each cycle. Eventually, the cycles stop completely. The cessation of menstrual cycles is called menopause (men′ ō -pawz; me¯n, month + pausis, cessation), and the whole time period from the onset of irregular cycles to their complete cessation is called the female climacteric (klı̄-mak′ter-ik).
The major cause of menopause is age-related changes in the ovaries. The number of follicles remaining in the ovaries of menopausal women is small. In addition, the follicles that remain become less sensitive to stimulation by FSH and LH, and therefore fewer mature follicles and corpora lutea are produced.
Older women experience gradual changes in response to the reduced amount of estrogen and progesterone produced by the ovaries (table 19.4). For example, during the climacteric, some women experience sudden episodes of uncomfortable sweating (hot flashes), fatigue, anxiety, temporary decrease in libido, and occasionally emotional disturbances. Many of these symptoms can be treated successfully with hormone replacement therapy (HRT), which usually consists of small amounts of estrogen and progester-one. HRT has been linked to a slightly increased risk of developing breast cancer, uterine cancer, heart attack, stroke, or blood clots. On the positive side, HRT slows the decrease in bone density that can become severe in some women after menopause, and it decreases the risk of developing colorectal cancer.
Related Topics