Chapter: Medical Physiology: Insulin, Glucagon, and Diabetes Mellitus
Mechanisms of Insulin Secretion
Mechanisms of Insulin Secretion
Figure 78–7 shows the basic cellular mechanisms for insulin secretion by the pancreatic beta cells in response to increased blood glucose concentration, the primary controller of insulin secretion. The beta cells have a large number of glucose transporters (GLUT-2) that permit a rate of glucose influx that is propor-tional to the blood concentration in the physiologic range. Once inside the cells, glucose is phosphorylated to glucose-6-phosphate by glucokinase. This step appears to be the rate limiting for glucose metabolism in the beta cell and is considered the major mechanism for glucose sensing and adjustment of the amount of secreted insulin to the blood glucose levels.
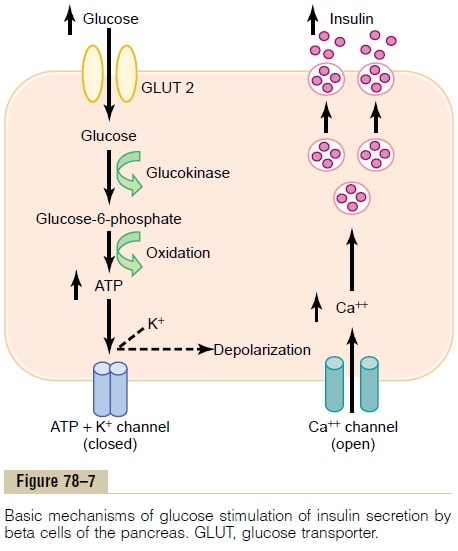
The glucose-6-phosphate is subsequently oxidized to form adenosine triphosphate (ATP), which inhibits the ATP-sensitive potassium channels of the cell. Closureof the potassium channels depolarizes the cell mem-brane, thereby opening voltage-gated calcium chan-nels, which are sensitive to changes in membranevoltage. This produces an influx of calcium that stimu-lates fusion of the docked insulin-containing vesicles with the cell membrane and secretion of insulin into the extracellular fluid by exocytosis.
Other nutrients, such as certain amino acids, can also be metabolized by the beta cells to increase intracel-lular ATP levels and stimulate insulin secretion. Some hormones, such as glucagon and gastric inhibitory peptide, as well as acetylcholine increase intracellular calcium levels through other signaling pathways and enhance the effect of glucose, although they do not have major effects on insulin secretion in the absence of glucose. Other hormones, including somatostatin and norepinephrine (by activating a-adrenergic recep-tors), inhibit exocytosis of insulin.
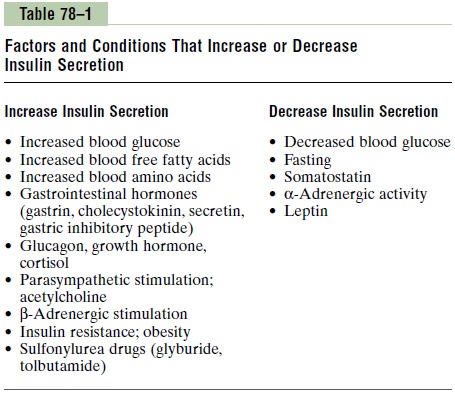
Sulfonylurea drugs stimulate insulin secretion by binding to the ATP-sensitive potassium channels and blocking their activity. This results in a depolarizing
Related Topics