Chapter: Clinical Anesthesiology: Anesthetic Management: Respiratory Physiology& Anesthesia
Mechanisms of Breathing
MECHANISMS OF BREATHING
The periodic exchange of alveolar gas
with the fresh gas from the upper airway reoxy-genates desaturated blood and
eliminates CO2. This exchange is brought about by
small cyclic pressure gradients established within the airways. During
spontaneous ventilation, these gradients are second-ary to variations in
intrathoracic pressure; during mechanical ventilation, they are produced by
inter-mittent positive pressure in the upper airway.
Spontaneous Ventilation
Normal pressure variations during
spontaneous breathing are shown in Figure 23–3. The pressure within alveoli is
always greater than the surrounding (intrathoracic) pressure unless the alveoli
are col-lapsed. Alveolar pressure is normally atmospheric (zero for reference)
at end-inspiration and end-expiration. By convention in pulmonary physiology,
pleural pressure is used as a measure of intrathoracic pressure. Although it
may not be entirely correct to refer to the pressure in a potential space, the
concept allows the calculation of transpulmonary pressure.
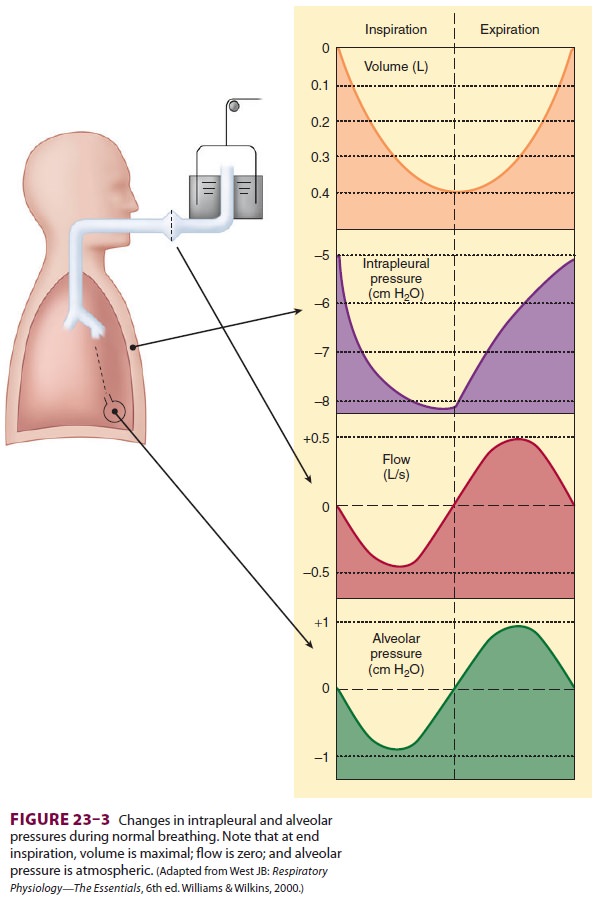
Transpulmonary
pressure, or Ptranspulmonary, is then defined as follows:
Ptranspulmonary
= Palveolar −Pintrapleural
At
end-expiration, intrapleural pressure nor-mally averages about –5 cm H2O,
and because alveo-lar pressure is 0 (no flow), transpulmonary pressure
is
+5
cm H2O.
Diaphragmatic
and intercostal muscle acti-vation during inspiration expands the chest and
decreases intrapleural pressure from –5 cm H 2O to –8 or –9 cm H2O.
As a result, alveolar
pressure also decreases (between –3 and –4 cm H 2O),
and an alveolar–upper airway gradient is established; gas flows from the upper
airway into alveoli. At end-inspiration (when gas inflow has ceased), alveolar
pressure returns to zero, but intrapleural pressure remains decreased; the new
transpulmonary pres-sure (5 cm H2O) sustains lung expansion.
During expiration, diaphragmatic
relaxation returns intrapleural pressure to –5 cm H2O. Now the transpulmonary pressure does not support
the new lung volume, and the elastic recoil of the lung causes a reversal of
the previous alveolar–upper airway gradient; gas flows out of alveoli, and
original lung volume is restored.
Mechanical Ventilation
Most forms of mechanical ventilation
intermittently apply positive airway pressure at the upper airway. During
inspiration, gas flows into alveoli until alveo-lar pressure reaches that in
the upper airway. During the expiratory phase of the ventilator, the positive
airway pressure is removed or decreased; the gradi-ent reverses, allowing gas
flow out of alveoli.
Related Topics