Chapter: Obstetrics and Gynecology: Hypertension in Pregnancy
Management of Hypertension in Pregnancy
MANAGEMENT
The goal
of management of hypertension in pregnancy is to bal-ance the management of
both fetus and mother and to optimize the outcome for each. Maternal
blood pressure should be mon-itored and the mother should be observed for the
sequelae of the hypertensive disease. Intervention for maternal indi-cations
should occur when the risk of permanent disability or death for the mother
without intervention outweighs the risks to the fetus caused by intervention.
For the fetus, there should be regular evaluation of fetal well-being and fetal
growth, with intervention becoming necessary if the intra-uterine environment
provides more risks to the fetus than delivery with subsequent care in the
newborn nursery.
Chronic Hypertension
The
management of patients with chronic hypertension in preg-nancy involves closely
monitoring maternal blood pressure and watching for the superimposition of
preeclampsia or eclampsia, and following the fetus for appropriate growth and
fetal well-being. Medical treatment of essential
hypertension has beendisappointing, in that no significant improvement in
preg-nancy outcome has been demonstrated with treatment.
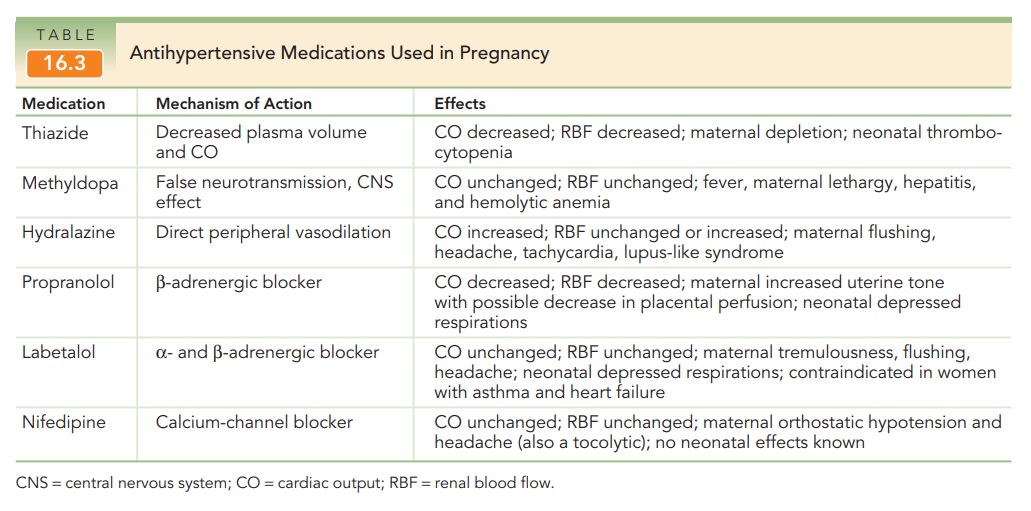
Antihypertensive
medication in women with chronic hyper-tension is generally not given unless
the systolic blood pressure is 150 to 160 mm Hg or the diastolic blood pressure
100 to
The purpose of such medications is to reducethe
likelihood of maternal stroke. Methyldopa is a com-monly used antihypertensive
medication for this purpose, although a combined alpha-and-beta-blocker (such
as la-betalol) and calcium-channel blockers (such as nifedipine) are also
commonly used. It was formerly taught that di-uretics were contraindicated
during pregnancy, but di-uretic therapy is no longer discontinued, and indeed
is usually continued, in the patient who already has been on such therapy
before becoming pregnant.
Preeclampsia
The severity of the preeclampsia
and the maturity of the fetus are the primary considerations in the management
of preeclampsia. Care must be individualized, but there are well-accepted
general guidelines.
The
mainstay of management for patients with mild preeclampsia is rest and frequent
monitoring of mother and fetus. Testing for suspected fetal growth restriction
or oligohydramnios and twice-weekly nonstress tests, biophysical profiles, or
both, are commonly employed and should be repeated as indicated, accord-ing to
maternal condition. Testing is recommended
twiceweekly for suspected fetal growth restriction or oligo-hydramnios.
Ultrasound examination for fetal growth and amniotic fluid assessment is
recommended every 3 weeks. Daily fetal movement assessment also may prove useful.
Hospitalization is often
initially recommended for women with new-onset preeclampsia. After maternal and
fetal conditions are serially assessed, subsequent manage-ment may be continued
in the hospital, at a day-care unit, or at home on the basis of the initial
assessment.
For the
patient with worsening preeclampsia or the patient who has severe preeclampsia,
management is often best accom-plished in a tertiary-care setting. Daily
laboratory tests andfetal surveillance may be indicated. Stabilization with
mag-nesium sulfate, antihypertensive therapy (as indicated), monitoring for
maternal and fetal well-being, and deliv-ery by either induction or cesarean
delivery are required.
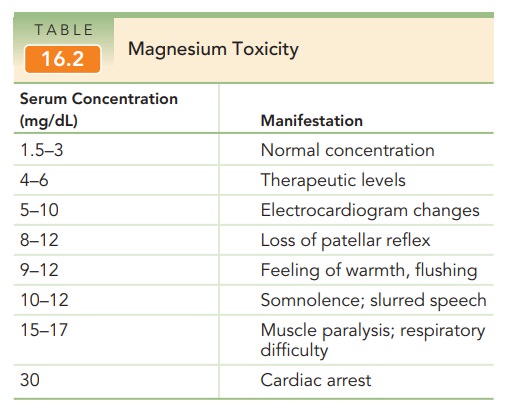
For almost a century, magnesium sulfate has been used to prevent and to treat eclamptic convulsions. Other anticonvulsants, such as diazepam and phenytoin, are rarely used because they are not as efficacious as magne-sium and because they have potential adverse effects on the fetus. Magnesium sulfate is administered by intramuscularor intravenous routes, although the latter is far more common. In 98% of cases, convulsions will be prevented. Therapeuticlevels are 4 to 6 mg/dL with toxic concentrations having pre-dictable consequences (Table 16.2). Frequent evaluations ofthe patient’s patellar reflex and respirations are necessary to monitor for manifestations of rising serum magnesium concentrations. In addition, because magnesium sulfate is excreted solely from the kidney, maintenance of urine output of at least 25 mL/hour will help avoid accumulation of the drug. Reversal of the effects of excessive magne-sium concentrations is accomplished by the slow intra-venous administration of 10% calcium gluconate, along with oxygen supplementation and cardiorespiratory sup-port, if needed.
Antihypertensive therapy is initiated if, on repeated measurements, the systolic blood pressure is >160 mm Hg or if diastolic blood pressure exceeds 105 to 110 mm Hg. Hydralazine is often the initial antihypertensive medica-tion of choice, given in 5- to 10-mg increments intra-venously until an acceptable blood pressure response is obtained. A 10- to 15-minute response time is usual. Thegoal of such therapy is to reduce the diastolic pressure to the 90-to 100-mm Hg range. Further reduction of the bloodpressure may impair uterine blood flow to rates that are dangerous to the fetus. Labetalol is another agent used to manage severe hypertension (Table 16.3).
Once
anticonvulsant and antihypertensive therapies are established in patients with
severe preeclampsia or eclampsia, attention is directed toward delivery. Induction
of labor isoften attempted, although cesarean delivery may be needed either if
induction is unsuccessful or not possible, or if the maternal or fetal status
is worsening. At delivery, blood loss must be closely monitored, because
patients with pre-eclampsia or eclampsia have significantly reduced blood
volumes. After delivery, patients remain in the labor and delivery area for 24
hours (longer if the clinical situation warrants) for close observation of
their clinical progress and further administration of magnesium sulfate to
pre-vent postpartum eclamptic seizures. Approximately 25% of eclamptic seizures
occur before labor, 50% occur during labor, and 25% occur in the first 24 hours
after delivery. Usually, the vasospastic process begins to reverse itself in
the first 24 to 48 hours after delivery, as manifested by a brisk diuresis.
Eclampsia
The eclamptic seizure is life-threatening for mother and fetus. Maternal risks include musculoskeletal
injury (includingbiting the tongue), hypoxia, and aspiration. Maternal
therapyconsists of inserting a padded tongue blade, restraining gently as
needed, providing oxygen, assuring maintenance of an adequate airway, and
gaining intravenous access. Eclamptic seizures are usually self-limited, so
medical ther-apy should be directed to the initiation of magnesium ther-apy (4
to 6 g slowly, intravenously) to prevent further seizures. If a patient receiving
magnesium sulfate experi-ences a seizure, additional magnesium sulfate (usually
2 g slowly) can be given, and a blood level obtained. Other anticonvulsant
therapy with diazepam or similar drugs is generally not warranted.
Transient uterine hyperactivity
for up to 15 minutes is associated with fetal heart rate changes, including
brady-cardia or compensatory tachycardia, decreased variability, and late
decelerations. These are self-limited and are not dangerous to the fetus unless
they continue for 20 minutes or more. Delivery
during this time imposes unnecessary risk formother and fetus and should be
avoided. Arterial blood gasesare often obtained, any metabolic disturbance
should be corrected, and a Foley catheter should be placed to mon-itor urinary
output. If the maternal blood pressure is high, if maternal urinary output is
low, or if there is evidence of cardiac disturbance, consideration of a central
venous catheter and, perhaps, continuous electrocardiogram mon-itoring is
appropriate.
HELLP Syndrome
Patients with HELLP syndrome are
often multiparous and have blood pressure recordings lower than those of many
preeclamptic patients. The liver dysfunction may be man-ifest as right-upper-quadrant
pain, and is all too commonly misdiagnosed as gallbladder disease or
indigestion. Major morbidity and mortality with unrecognized HELLP make
accurate diagnosis imperative. The first symptoms are often vague, including
nausea and emesis and a nonspecific viral-like syndrome. Treatment of these gravely ill patients is bestdone in a high-risk
obstetric center and consists of cardiovascu-lar stabilization, correction of
coagulation abnormalities, and delivery. Platelet transfusion before or
after delivery isindicated if the platelet count is <20,000/mm3, and it may be advisable to
transfuse patients with a platelet count <50,000/mm3 before proceeding with a
cesarean birth. Management of cases of HELLP syndrome should be individualized
based on gestational age at presentation, maternal symptoms, physical
examination, laboratory find-ings, and fetal status.
Related Topics