Chapter: Obstetrics and Gynecology: Human Sexuality
Management of Human Sexuality
MANAGEMENT
A woman’s sexuality is influenced
by her health and emotional well-being; likewise, healthy sexual function-ing
promotes physical and emotional well-being. How-ever, studies suggest that
fewer than one-half of patients’ sexual concerns are recognized by their
physicians. The
obstetrician-gynecologist has a
paramount role in assessing sexual function and managing sexual dysfunc-tion to
ensure the well-being of his or her patients. Beginning with screening a
patient for sexual dysfunc-tion, taking her history, and assessing sexual
dysfunction risk factors, the physician establishes a diagnosis if dys-function
is present and treats the patient or refers her for treatment, as appropriate.
Screening for Sexual Dysfunction
Questioning patients about their sexual desire, especially about responsive desire and the components of arousal, can point to management options about which patients and their partners can be counseled.
Simply providing infor-mation, confirming that many women have the same
con-cerns, and explaining how one aspect of dysfunction leads to another can be
therapeutic.
Discussions of sexuality are accomplished
best in a confidential and supportive setting. Mutual trust and respect in the
patient–clinician relationship will allow appropriate discussion of questions
and concerns about sexuality. A nonjudgmental and respectful approach by the
clinician, as well as awareness by the clinician of his or her own biases, is
essential for effective care.
Patients are more likely to develop trusting rela-tionships with their healthcare practitioners when the issue of confidentiality has been addressed directly.
A confidential relationship, in
turn, can facilitate the open disclosure of health histories and behaviors. The
use of broad, open-ended questions in a routine history gath-ering can help
disclose problems that require further exploration. Inquiry about the partner’s
sexual function and level of satisfaction may elicit more specific infor-mation
and give an indication of the couple’s level of communication.
The following are examples of
basic questions, posed in a gender-neutral fashion:
“Are you sexually active?”
“Are you sexually satisfied?”
“Do you think your partner is
satisfied?”
“Do you have questions or concerns
about sexual func-tioning?”
The clinician should not make
assumptions about the woman’s choice of partner. Although most women report
that their sexual partners are men, some women only have sex with other women,
and others may have partners of both sexes. The use of terms such as partner instead of husband and sexual activity
instead of intercourse and an
understand-ing of nonheterosexual sexuality—including that of les-bians,
bisexual women, and transgendered individuals— will assist in open communication
and assessment of the patient’s problem.
History
The patient’s history is the
crucial part of an assessment for sexual dysfunction. The duration of the
dysfunction and how long it has evolved over months or years should be clar-ified.
Lifelong problems are particularly difficult to evaluate and manage, and a
concomitant in-depth psychological assessment may be needed. The context of the
patient’s life when the dysfunction began is needed, addressing psycho-logic,
biologic, and relationship factors. Her medical history and past sexual
experiences are recorded, including med-ications and any substance abuse. The
woman’s develop-mental history also may be needed, particularly if her
dysfunction is lifelong.
Deliberate inquiries should be
made to assess the quality of the interpersonal relationship between the
patient and her partner, including mutual satisfaction with their sexual
relationship. The perceived impor-tance of physical intimacy for a given couple
depends largely on whether or not they are satisfied with that aspect of their
relationship. Among couples who are not experiencing sexual dysfunctions, each
partner will esti-mate that the sexual component of their relationship accounts
for approximately 10% of their overall happi-ness. In couples experiencing
sexual difficulties, however, the sexual aspects are estimated as accounting
for approx-imately 60% of the overall relationship quality. This dra-matic
shift in perception underscores the importance that physical intimacy holds
within the context of the over-all relationship.
Risk Factors
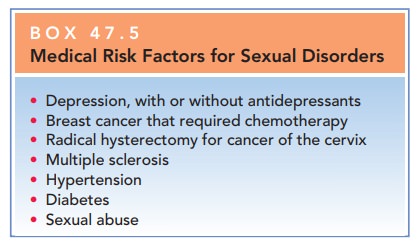
Sexual disorders often are
disclosed by women during vis-its for routine gynecologic care. Some patients
present with a complaint involving a sexual issue or of a specific sexual
dysfunction. Other patients neither express a sexu-ally related complaint nor
have a medical problem with a commonly associated sexual issue. Still other
patients have a medical problem or have or have had a medical or surgi-cal
therapy that is known to be associated with sexual issues or problems (Box
47.5).
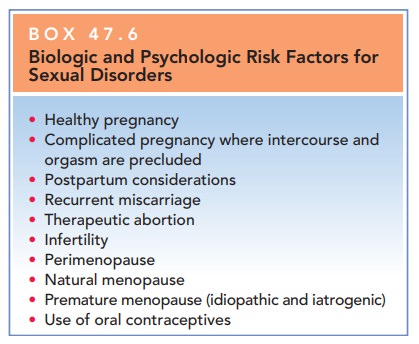
In addition, sexual function may
be affected by bio-logic and psychologic aspects of reproduction and the life
cycle (Box 47.6). The mechanisms governing the interplay
Box 47.5
Medical Risk Factors for Sexual Disorders
Depression, with or without antidepressants
Breast cancer that required chemotherapy
Radical hysterectomy for cancer of the cervix
Multiple sclerosis
Hypertension
Diabetes
Sexual
abuse
Box 47.6
Biologic and Psychologic Risk Factors for Sexual Disorders
Healthy pregnancy
Complicated pregnancy where intercourse and orgasm are precluded
Postpartum considerations
Recurrent miscarriage
Therapeutic abortion
Infertility
Perimenopause
Natural menopause
Premature menopause (idiopathic and iatrogenic)
Use of oral contraceptives
However, women’s past sexual experiences, self-image, support
from and attraction to their sexual partners, suffi-ciency of their knowledge
of sexuality, and sense of con-trol are all typically important factors.
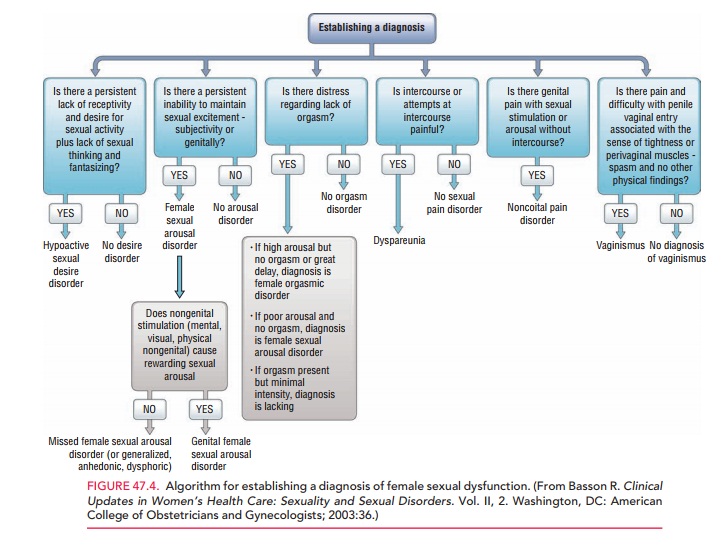
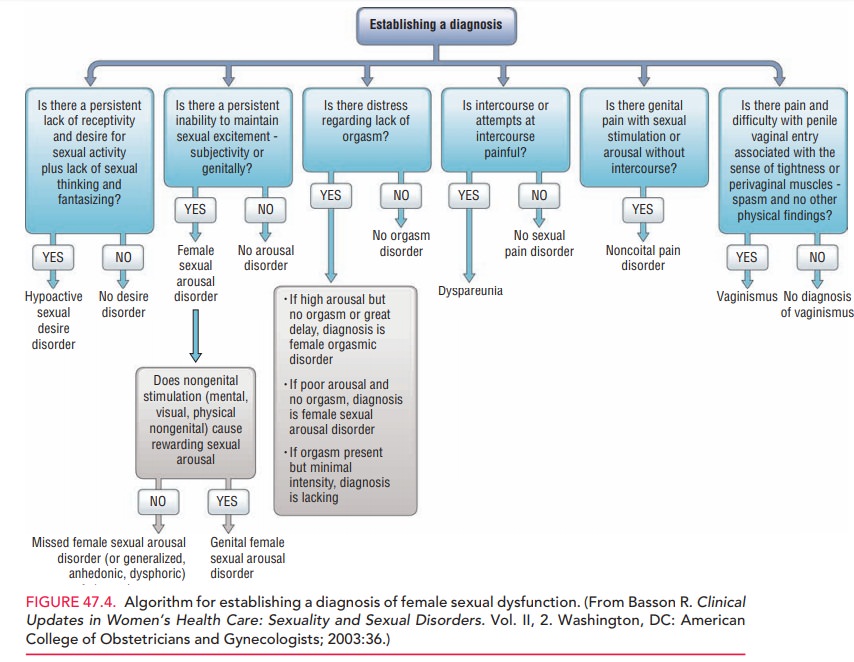
Establishing a Diagnosis
For all of the various
dysfunctions, it is important to estab-lish whether it is lifelong or acquired
and to distinguish between dysfunctions that are situational and those that are
global or generalized (Fig. 47.4). If the woman’s sex-ual response is healthy
in some circumstances, physical organic factors are not involved in a
dysfunction. It is therefore important to ask patients about their sexual
response with masturbation, with viewing or reading erot-ica, and with being
with individuals other than their regu-lar partners—even if this activity does
not involve physical sexual interaction.
Treatment
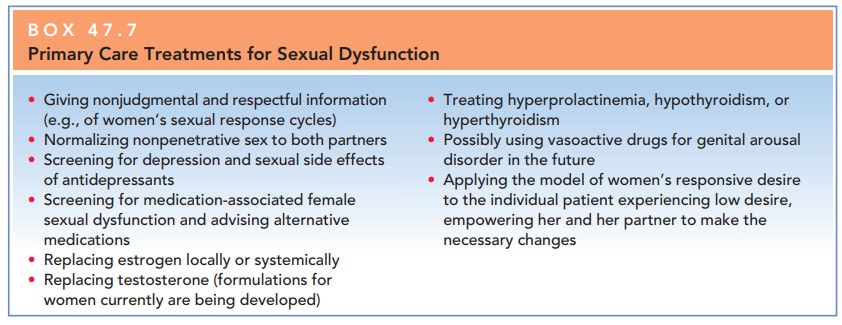
Some sexual problems can be managed by the primary physi-cian, whereas others are best referred to a sex therapist. Adetailed, sensitive, and respectful assessment will help establish a dialogue with the patient. It is difficult to dis-tinguish between assessment and treatment, because the physician often provides information during the assess-ment that is therapeutic. Treatment may be within the scope of the obstetrician-gynecologic practice, or a refer-ral may be appropriate, depending on the nature and the extent of the problem. Box 47.7 shows interventions that commonly occur in gynecologic offices.
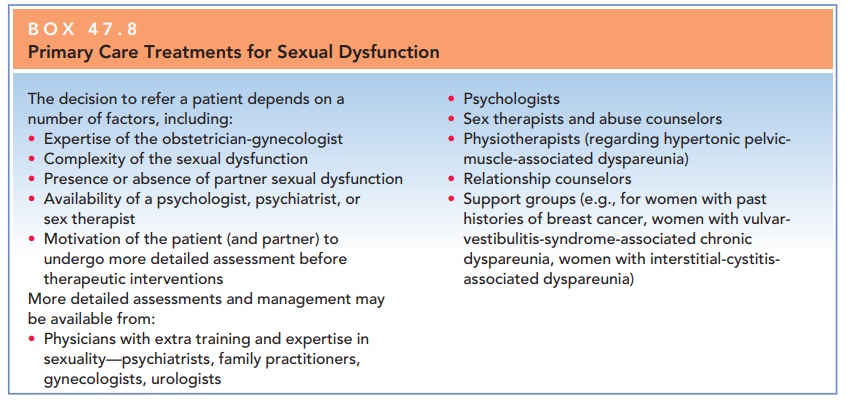
Largely, the decision should be based on whether or not the physician has adequate resources to
approach sexual dysfunction from an integrated perspective, rather than merely
a biological one. Psychology, pharmacology, partner inti-macy, and alternative
therapies are some of the other factors that must be addressed in treating
sexual dys-function. Referrals to mental health practitioners, marriage or
relationship counselors, or sex therapists may be appropriate. Box 47.8 shows
when and why to refer patients.
Related Topics