Chapter: Essentials of Anatomy and Physiology: The Reproductive Systems
Male Reproductive System in Human
MALE REPRODUCTIVE SYSTEM
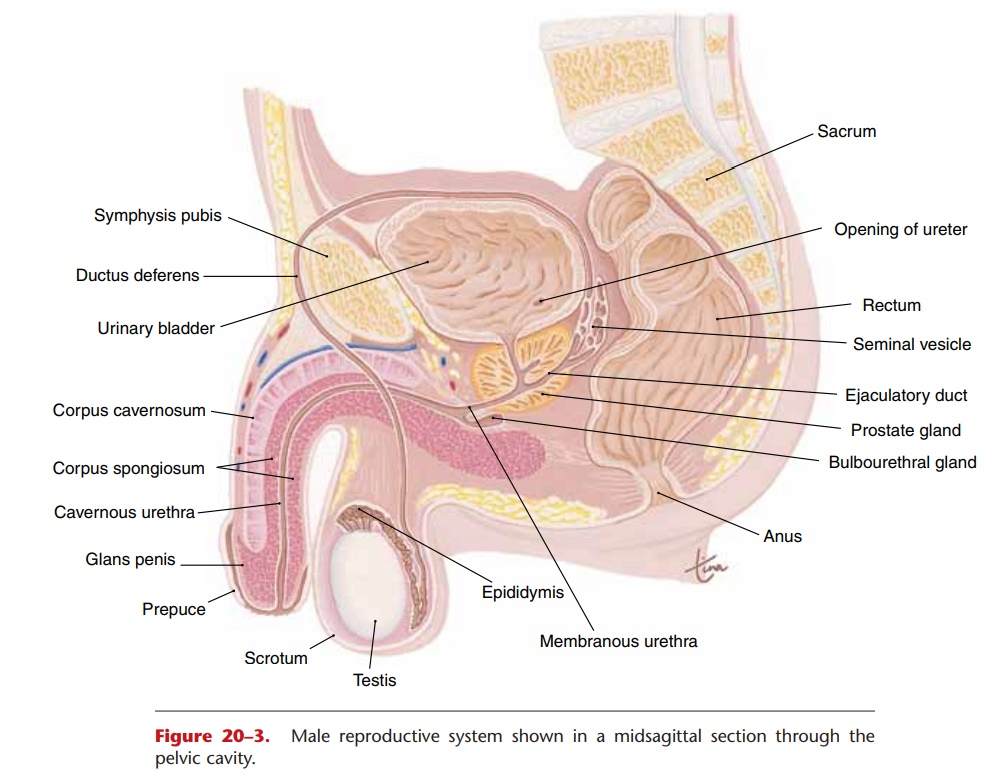
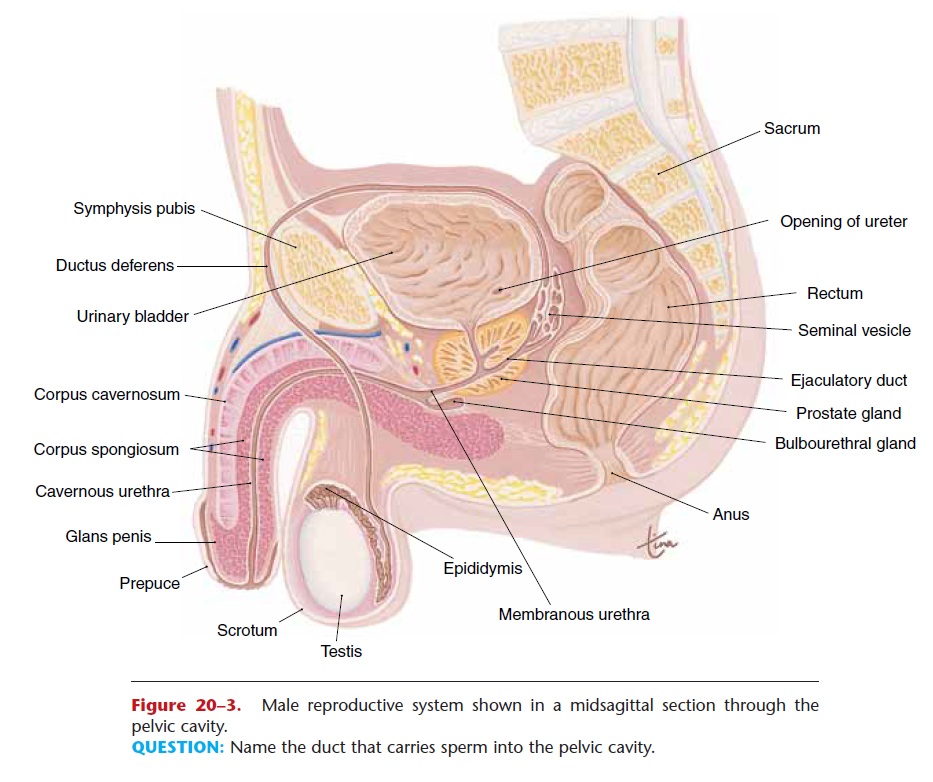
The male reproductive system consists of the testes and a series of ducts and glands. Sperm are produced in the testes and are transported through the repro-ductive ducts: epididymis, ductus deferens, ejaculatory duct, and urethra (Fig. 20–3). The reproductive glands produce secretions that become part of semen, the fluid that is ejaculated from the urethra. These glands are the seminal vesicles, prostate gland, and bul-bourethral glands.
TESTES
The testes are located in the scrotum, a sac of skin between the upper thighs. The temperature within the scrotum is about 968F, slightly lower than body temperature, which is necessary for the production of viable sperm. In the male fetus, the testes develop near the kidneys, then descend into the scrotum just before birth. Cryptorchidism is the condition in which the testes fail to descend, and the result is sterility unless the testes are surgically placed in the scrotum.
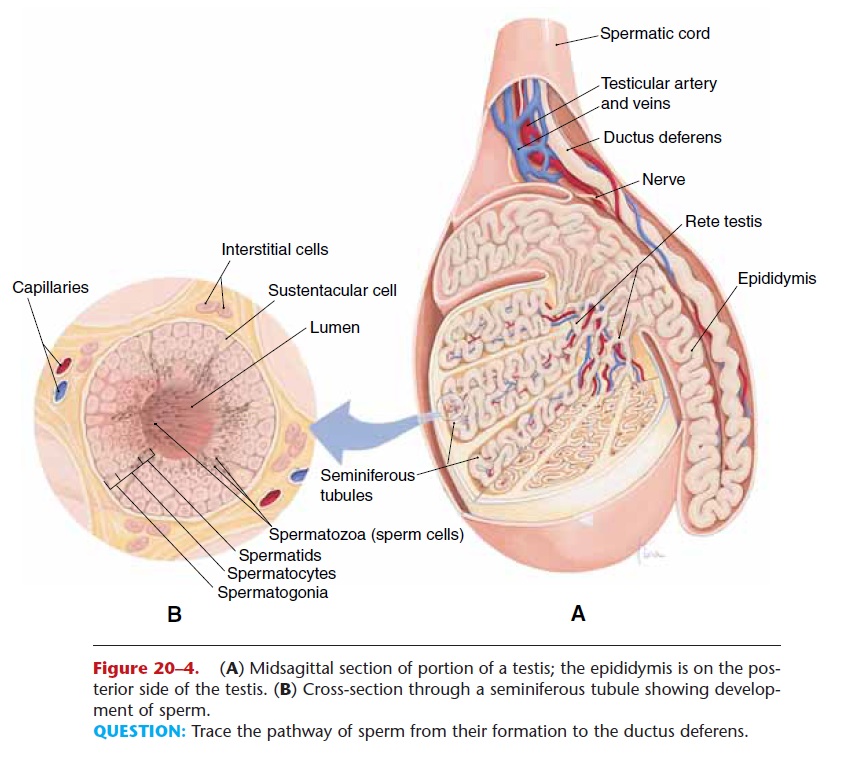
Figure 20–4. (A) Midsagittal section of portion of a testis; the epididymis is on the pos-terior side of the testis. (B) Cross-section through a seminiferous tubule showing develop-ment of sperm.
QUESTION: Trace the pathway of sperm from their formation to the ductus deferens.
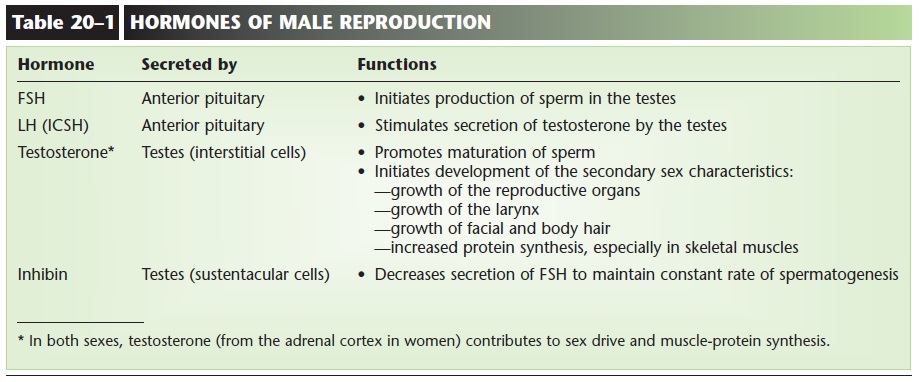
Each testis is about 1.5 inches long by 1 inch wide (4 cm by 2.5 cm) and is divided internally into lobes (Fig. 20–4). Each lobe contains several seminiferous tubules, in which spermatogenesis takes place. Among the spermatogonia of the seminiferous tubules are sustentacular (Sertoli) cells, which produce the hormone inhibin when stimulated by testosterone. Between the loops of the seminiferous tubules are interstitial cells, which produce testosterone when stimulated by luteinizing hormone (LH) from the anterior pituitary gland. Besides its role in the matu-ration of sperm, testosterone is also responsible for the male secondary sex characteristics, which begin to develop at puberty (Table 20–1).
A sperm cell consists of several parts, which are shown in Fig. 20–1. The head contains the 23 chro- mosomes. On the tip of the head is the acrosome, which is similar to a lysosome and contains enzymes to digest the membrane of an egg cell. Within the mid-dle piece are mitochondria that produce ATP. The fla-gellum provides motility, the capability of the sperm cell to move. It is the beating of the flagellum that requires energy from ATP.
Sperm from the seminiferous tubules enter a tubu-lar network called the rete testis, then enter the epi-didymis, the first of the reproductive ducts.
EPIDIDYMIS
The epididymis (plural: epididymides) is a tube about 20 feet (6 m) long that is coiled on the posterior sur-face of each testis (see Fig. 20–4). Within the epididymis the sperm complete their maturation, and their flagella become functional. Smooth muscle in the wall of the epididymis propels the sperm into the ductus deferens.
DUCTUS DEFERENS
Also called the vas deferens, the ductus deferens extends from the epididymis in the scrotum on its own side into the abdominal cavity through the inguinal canal. This canal is an opening in the abdominal wall for the spermatic cord, a connective tissue sheath that contains the ductus deferens, testicular blood vessels, and nerves. Because the inguinal canal is an opening in a muscular wall, it is a natural “weak spot,” and it is the most common site of hernia formation in men.
Once inside the abdominal cavity, the ductus defer-ens extends upward over the urinary bladder, then down the posterior side to join the ejaculatory duct on its own side (see Fig. 20–3). The smooth muscle layer of the ductus deferens contracts in waves of peristalsis as part of ejaculation.
EJACULATORY DUCTS
Each of the two ejaculatory ducts receives sperm from the ductus deferens and the secretion of the sem-inal vesicle on its own side. Both ejaculatory ducts empty into the single urethra (see Fig. 20–3).
SEMINAL VESICLES
The paired seminal vesicles are posterior to the uri-nary bladder (see Fig. 20–3). Their secretion contains fructose to provide an energy source for sperm and is alkaline to enhance sperm motility. The duct of each seminal vesicle joins the ductus deferens on that side to form the ejaculatory duct.
PROSTATE GLAND
A muscular gland just below the urinary bladder, the prostate gland is about 1.2 inches high by 1.6 inches wide by 0.8 inch deep (3 cm by 4 cm by 2 cm, about the size of a walnut). It surrounds the first inch of the ure-thra as it emerges from the bladder (see Fig. 20–3). The glandular tissue of the prostate secretes an alkaline
fluid that helps maintain sperm motility. The smooth muscle of the prostate gland contracts during ejacula-tion to contribute to the expulsion of semen from the urethra.
BULBOURETHRAL GLANDS
Also called Cowper’s glands, the bulbourethral glands are about the size of peas and are located below the prostate gland; they empty into the urethra. Their alkaline secretion coats the interior of the urethra just before ejaculation, which neutralizes any acidic urine that might be present.
You have probably noticed that the secretions of the male reproductive glands are alkaline. This is important because the cavity of the female vagina has an acidic pH created by the normal flora, the natural bacterial population of the vagina. The alkalinity of seminal fluid helps neutralize the acidic vaginal pH and permits sperm motility in what might otherwise be an unfavorable environment.
URETHRA—PENIS
The urethra is the last of the ducts through which semen travels, and its longest portion is enclosed within the penis. The penis is an external genital organ; its distal end is called the glans penis and is cov-ered with a fold of skin called the prepuce or foreskin.Circumcision is the surgical removal of the foreskin This is a common procedure performed on male infants, and though there is considerable medical debate as to whether circumcision has a useful pur-pose, some research studies have found fewer cases of HIV infection among circumcised men, compared with men who are uncircumcised.
Within the penis are three masses of cavernous (erectile) tissue (see Fig. 20–3). Each consists of a framework of smooth muscle and connective tissue that contains blood sinuses, which are large, irregular vascular channels.
When blood flow through these sinuses is minimal, the penis is flaccid. During sexual stimulation, the arteries to the penis dilate, the sinuses fill with blood, and the penis becomes erect and firm. The dilation of penile arteries and the resulting erection are brought about by the localized release of nitric oxide (NO) and by parasympathetic impulses. The erect penis is capa-ble of penetrating the female vagina to deposit sperm. The culmination of sexual stimulation is ejaculation, a sympathetic response that is brought about by peristal-sis of all of the reproductive ducts and contraction of the prostate gland and the muscles of the pelvic floor.
SEMEN
Semen consists of sperm and the secretions of the seminal vesicles, prostate gland, and bulbourethral glands; its average pH is about 7.4. During ejacula-tion, approximately 2 to 4 mL of semen is expelled. Each milliliter of semen contains about 100 million sperm cells.
Related Topics