Chapter: Medicine and surgery: Endocrine system
Insulin therapy - Diabetes mellitus
Insulin therapy
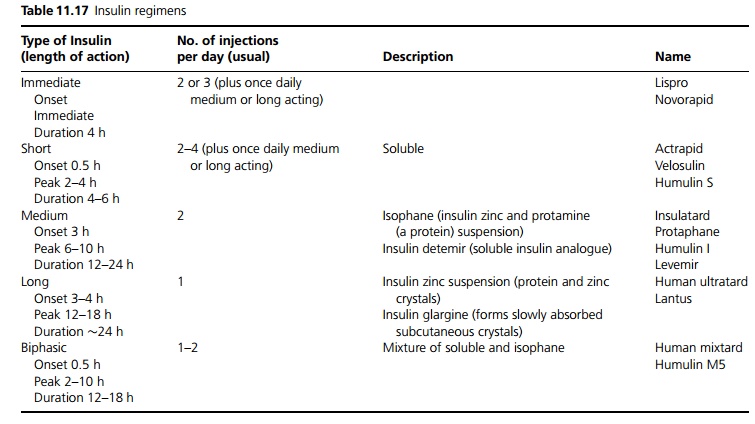
Synthetic insulin is administered subcutaneously in a variety of
regimens. Various insulins have been ‘designed’ with different pharmacokinetic
effects (see Table 11.17).
Two common regimens are used (see Fig. 11.15):
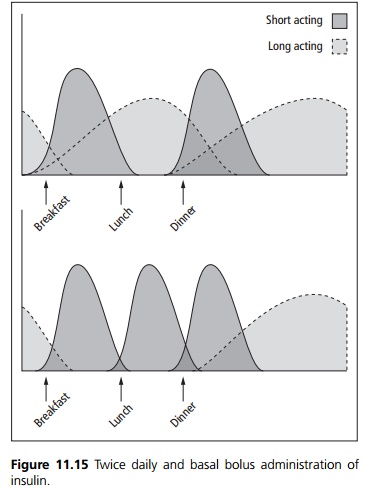
·
A twice daily adminstration of
biphasic insulin, with two thirds of the total daily dose given before
breakfast and one third given before the evening meal.
·
A bolus of short or immediate
acting insulin given three times a day at meal times and a medium or long-acting
insulin given at night. The advantage of this regimen is that meal times and
quantities can be varied. If immediate acting insulin is used it is taken at or
immediately after the meal, if short acting is used then this is administered
30 minutes before the meal.
A continuous subcutaneous insulin infusion or continuous intravenous
infusion via a tunelled line may also be used. An infusion pump controls the
rate and preprandial boosts can be given simply and easily. They are expensive
and if they fail, they can cause diabetic ketoacidosis, as there is no
longeracting reserve.
The site of injection also affects the absorption rate:
·
The abdominal wall is quickest
(use before meal-times).
·
The arms are intermediate.
·
The legs are the slowest (night-time).
Temperature and exercise affect absorption. Exercise also increases the
use of glucose and hence reduces the amount of insulin needed. Patients must be
educated about the problems with insulin therapy. For example, common sites of
injection may develop fat hypertrophy or fat atrophy. These sites then release
insulin poorly. Rotating the sites prevents these problems. Hypogly-caemia may
result from having too much insulin and not eating enough, or exercising. If a
patient is not eating, e.g. with vomiting due to gastroenteritis, then insulin
treatment should not be omitted, as the body still requires insulin to utilise
glucose. Instead, lower amounts should be used with careful monitoring, or the
patient will need to be admitted for intravenous glucose and insulin to avoid
either diabetic ketoacidosis or hyperos-molar non-ketotic coma.
Related Topics