Chapter: Medicine Study Notes : Endocrine and Electrolytes
Hyponatraemia
Hyponatraemia
Key Points
·
Normal value of Na: 135 – 145
mmol/L
·
Hyponatraemia is not a diagnosis
– it is found in diverse conditions. Body Na may be low, normal or high.
Relative water retention is a common factor
·
Condition and treatment can be
hazardous. If correct too fast then
pontine demyelination
·
Treatment must be slow and
monitored closely. Treatment can range from water restriction or diuresis to
sodium restriction or normal saline. Need to know underlying cause
·
Don‟t use hypotonic fluids
post-op unless Na is high. Eg dextrose saline – glucose absorbed very quickly
post surgery ® hypotonic
Symptoms
·
The big boogie is underlying
cerebral oedema. Bigger problem if abrupt onset. Rapid correction can cause
central pontine melanosis
·
Symptoms don‟t correlate well
with [Na]
·
Early: anorexia, headache,
nausea, vomiting, muscle cramps, weakness
·
Advanced: mutism, dysarthria, impaired response to
verbal or painful stimuli, bizarre behaviour, hallucinations, asterixis,
incontinence, respiratory insufficiency, spastic quadriparesis in 90%
·
Far advanced: (too late to do much) decorticate or
decerebrate posturing, bradycardia, hypo or hypertension, dilated pupils,
seizures, respiratory arrest, coma, polyuria (central diabetes insipidous)
·
Should always be a differential
in post-operative coma
Aetiology
·
Either Na depletion or water gain
(usually water gain)
·
Inappropriate water retention: eg
drugs (most common – eg antiepileptics), ÂADH, kidney or thyroid problems
·
May be borderline hyponatraemic
before (eg long term use of diuretics)
·
Normal ADH will  if Âosmolality
or ÂŻblood volume
·
Operative stress or serious
illness ® syndrome of inappropriate ADH (in most people) ® water
retention (especially in women, smaller starting fluid volume). NB it‟s not
really inappropriate – the body is making a justifiable physiological response:
I‟m stressed so conserve water rather than throwing it out.
·
Ageing impairs fluid homeostasis ® wider
swings happen easily
Assessment
·
History: fluid losses, diuretics, other medications
·
Clinical findings: pulse, blood
pressure, volume assessment, oedema, thirst, skin, input/output
·
Laboratory:
o Creatinine, urea, glucose, HCO3, K, plasma osmolarity, urine
Na and Osmolarity
o Severe hyponatraemia is < 125 mmol/l: nausea, malaise, headache
o < 115 mmol/l: convulsions
·
Look for:
o Low Na and ÂŻ serum osmolality
o Urine osmolality higher than expected (>200 and usually > serum
osmolality)
o Urinary sodium higher than expected (> 30)
o Normal pituitary, adrenal, cardiac, and renal function
·
Clinically useful grouping (Ăž volume
assessment critical):
o Hyponatraemia with oedema: heart failure + diuretic, cirrhosis,
nephrosis (impairment of water loss via increased ADH +/- Na loss)
o Hyponatraemia with dehydration:
§ Urine [Na] > 20 mmol/l: Diuretics, Addison‟s Disease, Salt losing
nephritis
§ Urine [Na] < 20 mmol/l: Vomiting, Diarrhoea, Skin loss
§ Usually rehydrate slowly with normal saline
o Hyponatraemia with euvolaemia and reduced plasma osmolality:
§ Urine [Na] > 20 mmol/l: Chronic water overload (eg primary
polydypsia, chronic SIADH – central or malignancy, etc)
§ Urine [Na] < 20 mmol/l: Acute water overload (eg acute SIADH,
oxytocin for induced labour, etc)
·
Treat with fluid restriction <
1000 ml/day, and treat underlying cause
·
Complicating factors:
o If plasma osmolarity is high then measure glucose. Hyperglycaemia ® shift of
water out of muscle cells: Na ÂŻ 1 mmol/L for every 4 mmol/L Â in glucose
o If osmolarity is normal then pseudo-hyponatraemia (eg hyperlipidaemia,
hyperprotinaemia). An artefact: Na has been incorrectly measured in plasma
volume rather than plasma water
Syndrome of Inappropriate ADH secretion
·
= SIADH
· See Diabetes Insipidous
·
Ectopic ADH Production
(relatively rare): malignancies of lung, bronchus, brain, kidney, duodenum,
pancreas
·
Central production:
o Cerebral infections, trauma, tumours, haemorrhage
o Lung disease, eg pneumonia
o Drugs, eg morphine, carbamazepine (anti-epileptic)
o Can be seen in AIDS patients (?combination of above factors)
Common Scenarios
·
Prolonged vomiting and rehydration with Gastrolyte – only
contains 60 mmol/L Na
·
If dehydrated (eg vomiting) and
on diuretic, ADH still conserves water, but ÂŻNa retention so ÂŻ[Na]. We
preserve volume at the expense of osmolarity
·
Serious post-operative problem.
Especially women after elective surgery (eg gynaecology wards). Hypothesis:
surgery ® ÂADH (eg due to pain), dextrose also given in belief that it slows
catabolism and promotes healing – but together they lead to ¯[Na]
·
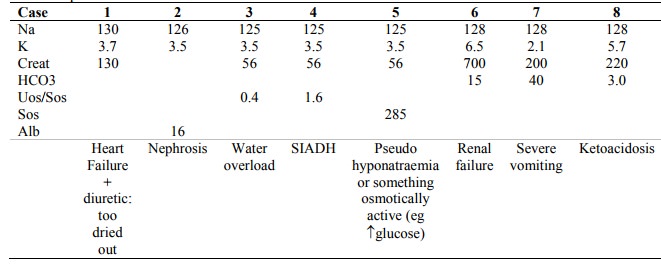
Sample cases:
· 
Treatment
·
Principles:
o Raise the sodium at a safe rate
o Treat the cause
·
Basic regimes:
o If volume depleted (Renal/GI losses, diuretics, adrenal insufficiency): saline isotonic to the patient or normal saline. Extra Na will have a small effect but Âvolume ® ÂŻADH ® excess water excreted
o Normovolaemic or oedematous (SIADH, renal failure, polydypsia, oedema): Water restriction
o If severe symptoms or if sodium < 110 then ?hypertonic saline. ÂNa by no
more than 12 mmol per 24 hours: keep rate smooth. Key judgement is speed of
infusion. No front loading. Animal studies show correction by > 14/mmol/24
hours ® lesions in 71% of dogs. If no symptoms – maybe go slower
·
Monitor 2 hourly. Manage in high dependency unit. Detect and treat hypoxia
·
Adverse neurological consequences
of rapid correction: myelin breakdown in the pons, patchy symmetrical lesions
elsewhere in the brain. But risk of not treating acute cerebral oedema far
exceeds the small risk of osmotic demyelination
·
Maybe frusemide to Âfree
water excretion
Dehydration or Volume Depletion
·
Dehydration:
o Often used loosely to describe a volume depleted patient
o Correctly it refers to ÂŻintracellular water, following fluid shifts from ICF to ECF
o Water is lost (either as pure water or as hypotonic fluid) ® Âosmolality
and thirst
o Treatment is water replacement (dextrose)
·
Volume depletion:
o Losses from the ECF (isotonic sodium) ® ¯circulating
volume
o ÂŻBP, Âtachycardia,
ÂŻtissue turgor
o Treatment is replacement of NaCl
·
Dehydration and volume depletion
can co-exist
Related Topics