Chapter: Clinical Cases in Anesthesia : Neonatal Resuscitation
How is neonatal resuscitation managed in the delivery room?
How is neonatal resuscitation managed in the delivery room?
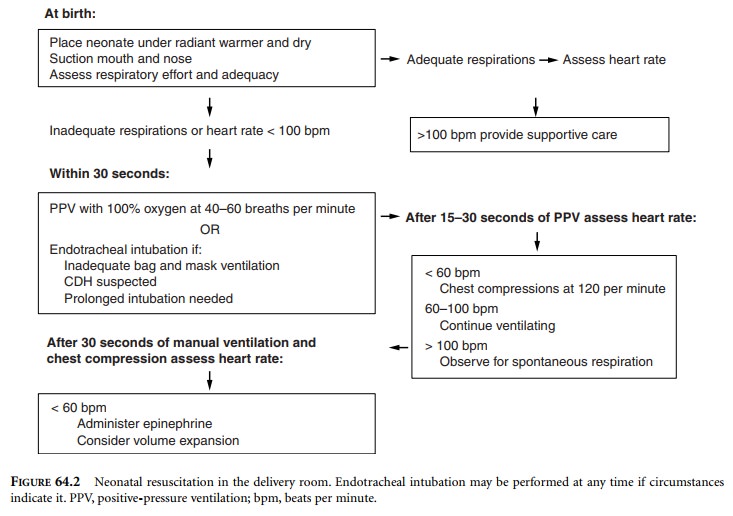
Within the first 20 seconds of birth, the
neonate should be placed under a radiant warmer and actively dried (Figure
64.2). The mouth and nose should be suctioned. Respiratory effort and adequacy
should be assessed within the first 30 seconds of birth. If there are adequate
sponta-neous respirations, the heart rate should then be assessed. If there is
no respiratory effort, inadequate respiratory effort (central cyanosis), or the
neonate is gasping, positive-pressure ventilation (PPV) with 100% oxygen should
be initiated at a rate of 40–60 breaths per minute with initial peak
inspiratory pressures of 30–40 cm H2O. Endotracheal intubation
should be performed if bag-and-mask ven-tilation is inadequate, a congenital
diaphragmatic hernia is suspected, or if there is a need for prolonged
intubation.
An endotracheal tube (3.0–3.5 mm ID) may also
be placed if a route for administration of resuscitative drugs is needed.
The heart rate should be checked after 15–30
seconds of PPV. If the heart rate is less than 60 beats per minute chest
compressions should be started at 120 compressions per minute. Chest
compressions can be accomplished in two ways:
·
Place
both thumbs on the lower sternum while the other fingers encircle the neonate
supporting the back.
·
Place
two fingers of one hand on the lower sternum while the other hand supports the
back.
The first method is preferred. Compressions
should be about one third of the depth of the chest. More impor-tantly,
compression depth should be sufficient to produce a palpable pulse. There
should be a 3:1 ratio of compres-sions to ventilations. Heart rate should be
reassessed every 30 seconds. Since cardiac depression is usually a result of
inadequate respirations, once oxygenation and ventilation is restored the heart
will in most cases resume normal function.
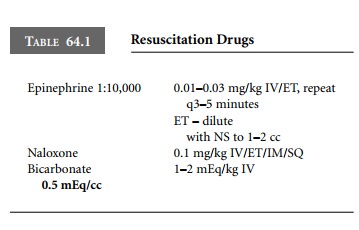
If after 30 seconds of manual ventilation and
chest com-pressions (90 seconds after birth) the heart rate remains below 60
beats per minute, epinephrine should be administered. Epinephrine 1:10,000 at a
dose of 0.01–0.03 mg/kg can be given either intravenously or endotracheally.
The epinephrine may be diluted to 1–2 cc with normal saline for endotracheal
administration. This should be repeated every 3–5 minutes as indicated (Table
64.1).
Additional resuscitative measures may include
volume expansion with an isotonic crystalloid solution or colloids for the
hypovolemic infant. Hypovolemia should be suspected in the infant who is not
responding to the usual resuscitative measures or whose physical examination is
consistent with shock. The initial dose of fluid is 10 cc/kg as a bolus.
Additional fluid management should be based on clinical assessment.
Naloxone, a narcotic antagonist, is indicated
for the respiratory-depressed neonate born within 4 hours of the mother
receiving opioids. The recommended dose is 0.1 mg/kg and may be given by the
intravenous, endotra-cheal, intramuscular, or subcutaneous route. Naloxone is
not given to a neonate of a mother who is narcotic-addicted because it may
precipitate withdrawal in the neonate. Once naloxone is given, the neonate must
be observed for recur-rence of apnea because the duration of action of the
opioid may exceed the effect of the naloxone.
Sodium bicarbonate should not be used routinely
during resuscitation of the neonate. It is indicated only after prolonged
resuscitation and documented metabolic acidosis on arterial blood gas. Adequate
ventilation and circulation should be established prior to its administra-tion.
The recommended dose is 1–2 mEq/kg of a 0.5
mEq solution.
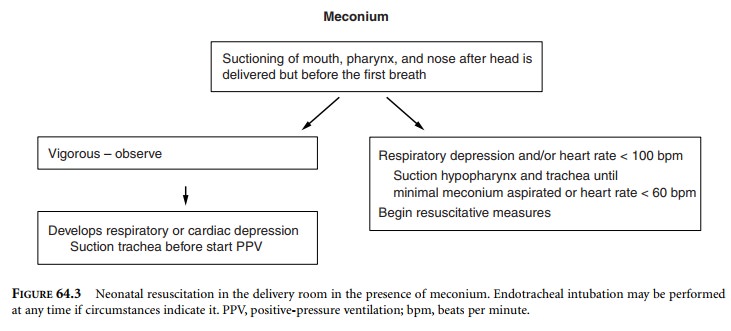
When meconium is present in the amniotic fluid,
specific steps should be taken to limit the risk of meconium aspiration (Figure
64.3). When the head of the neonate is delivered and prior to the neonate’s
first breath, suctioning of the mouth, pharynx, and nose should be done.
Despite this suctioning, there is a subset of neonates who will have meconium
in the trachea despite the absence of sponta-neous respirations. It is presumed
that this occurred in utero. If there is meconium-stained amniotic fluid and the
neonate is vigorous after delivery, there is no need to per-form tracheal
suctioning because it does not improve out-come. In fact, there may be
complications associated with tracheal suctioning such as laryngeal trauma.
However, if the neonate should develop respiratory or cardiac depres-sion
subsequently, suctioning of the trachea should pre-cede PPV. In the neonate who
has respiratory and/or cardiac depression (heart rate 60–100 beats per minute)
at birth, direct laryngoscopy should be performed to suction the hypopharynx
and to intubate the trachea for suctioning of any residual meconium that may be
present.
Repeated intubations and suctioning should be
performed until there is minimal meconium recovered or the heart rate is less
than 60 beats per minute. During this maneuver, an assistant should be
monitoring the heart rate continu-ously. Even if there is still meconium, once
the heart rate is less than 60 beats per minute, resuscitative measures should
be initiated immediately.
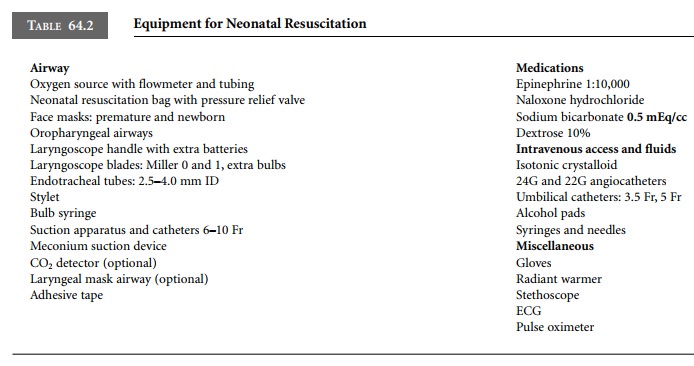
It is important that all the equipment and
pharmaco-logic agents necessary for resuscitation efforts are available and of
the appropriate size (Table 64.2).
Related Topics