Chapter: Medical Surgical Nursing: Assessment of Integumentary Function
Functions of the Skin
FUNCTIONS OF THE SKIN
Protection
The
skin covering most of the body is no more than 1 mm thick, but it provides very
effective protection against invasion by bac-teria and other foreign matter.
The thickened skin of the palms and soles protects against the effects of the
constant trauma that occurs in these areas.
The epidermis is the outermost layer of the skin
and is com-posed of several layers of keratinocytes that change character as
they migrate to the surface. The stratum corneum, the outer layer of the
epidermis, provides the most effective barrier to epidermal water loss and
penetration of environmental factors such as chem-icals, microbes, and insect
bites.
Various
lipids are synthesized in the stratum corneum and are the basis for the barrier
function of this layer. These are long-chain lipids that are better suited than
phospholipids for water re-sistance. The presence of these lipids in the
stratum corneum creates a relatively impermeable barrier for water egress and
for the entry of toxins, microbes, and other substances that come in contact
with the surface of the skin.
Some
substances do penetrate the skin but meet resistance in trying to move through
the channels between the cell layers of the stratum corneum. Microbes and
fungi, which are part of the body’s normal flora, cannot penetrate unless there
is a break in the skin barrier.
The
dermis–epidermis junction is the basal layer, which is composed of collagen.
The basal layer serves four functions. It acts as a scaffold for tissue
organization and a template for regen-eration; it provides selective
permeability for filtration of serum; it is a physical barrier between
different types of cells; and it ad-heres the epithelium to underlying cell
layers.
Sensation
The
receptor endings of nerves in the skin allow the body to con-stantly monitor
the conditions of the immediate environment. The primary functions of the
receptors in the skin are to sense temperature, pain, light touch, and pressure
(or heavy touch). Different nerve endings respond to each of the different
stimuli. Although the nerve endings are distributed over the entire body, they
are more concentrated in some areas than in others. For ex-ample, the
fingertips are more densely innervated than the skin on the back.
Fluid Balance
The
stratum corneum (ie, outermost layer of the epidermis) has the capacity to
absorb water, thereby preventing an excessive loss of water and electrolytes
from the internal body and retaining moisture in the subcutaneous tissues. When
skin is damaged, as occurs with a severe burn, large quantities of fluids and
electro-lytes may be lost rapidly, possibly leading to circulatory collapse,
shock, and death.
The skin is not completely impermeable to water.
Small amounts of water continuously evaporate from the skin surface. This
evap-oration, called insensible
perspiration, amounts to approximately 600 mL daily in a normal adult.
Insensible water loss varies with the body and ambient temperature. In a person
with a fever, the loss can increase. During immersion in water, the skin can
accu-mulate water up to three or four times its normal weight, such as swelling
of the skin that occurs after prolonged bathing.
Temperature Regulation
The body continuously produces heat as a result of
the metabo-lism of food, which produces energy. This heat is dissipated
pri-marily through the skin. Three major physical processes are involved in
loss of heat from the body to the environment. The first process, radiation, is
the transfer of heat to another object of lower temperature situated at a
distance. The second process, conduction, is the transfer of heat from the body
to a cooler object in contact with it. Heat transferred by conduction to the
air surrounding the body is removed by the third process, con-vection, which
consists of movement of warm air molecules away
from the body.
Evaporation from the skin aids heat loss by
conduction. Heat is conducted through the skin into water molecules on its
surface, causing the water to evaporate. The water on the skin surface may be
from insensible perspiration, sweat, or the environment.
Normally,
all of these mechanisms for heat loss are used. When the ambient temperature is
very high, however, radiation and convection are ineffective, and evaporation
becomes the only means for heat loss.
Under
normal conditions, metabolic heat production is bal-anced by heat loss, and the
internal temperature of the body is maintained constant at approximately 37°C (98.6°F). The rate of heat
loss depends primarily on the surface temperature of the skin, which is a
function of the skin blood flow. Under normal conditions, the total blood
circulated through the skin is approx-imately 450 mL per minute, or 10 to 20
times the amount of blood required to provide necessary metabolites and oxygen.
Blood flow through these skin vessels is controlled primarily by the
sympathetic nervous system. Increased blood flow to the skin results in more
heat delivered to the skin and a greater rate of heat loss from the body. In
contrast, decreased skin blood flow de-creases the skin temperature and helps
conserve heat for the body. When the temperature of the body begins to fall, as
occurs on a cold day, the blood vessels of the skin constrict, thereby reducing
heat loss from the body.
Sweating
is another process by which the body can regulate the rate of heat loss.
Sweating does not occur until the core body temperature exceeds 37°C, regardless of skin
temperature. In ex-tremely hot environments, the rate of sweat production may
be as high as 1 L per hour. Under some circumstances (eg, emotional stress),
sweating may occur as a reflex and may be unrelated to the need to lose heat
from the body.
Vitamin Production
Skin
exposed to ultraviolet light can convert substances necessary for synthesizing
vitamin D (cholecalciferol). Vitamin D is essen-tial for preventing rickets, a
condition that causes bone deformi-ties and results from a deficiency of
vitamin D, calcium, and phosphorus.
Immune Response Function
Research
findings (Demis, 1998) indicate that several dermal cells (ie, Langerhans
cells, interleukin-1–producing keratinocytes, and subsets of T lymphocytes) and
three varieties of human leukocyte antigen (ie, protein marker on white blood
cells indicating the type of cell) are important components of the immune
system. Ongoing research is expected to more clearly define the role of these
dermal cells in immune function.
Gerontologic Considerations
The skin undergoes many physiologic changes
associated with normal aging. A lifetime of excessive sun exposure, systemic
dis-eases, poor nutrition, and certain medications (eg, antihista-mines,
diuretics) can enhance the range of skin problems and the rapidity with which
they appear. The outcome is an increasing vulnerability to injury and to
certain diseases. Skin problems are common among
older people.
Before
conducting a skin assessment, the nurse needs to be aware of significant
changes that occur with aging. The major changes in the skin of older people
include dryness, wrinkling, uneven pigmentation, and various proliferative
lesions. Cellular changes associated with aging include a thinning at the
junction of the dermis and epidermis. This results in fewer anchoring sites
between the two skin layers, so that even minor injury or stress to the
epidermis can cause it to shear away from the dermis. This phenomenon of aging
may account for the increased vulnerabil-ity of aged skin to trauma. With
increasing age, the epidermis and dermis thin and flatten, causing wrinkles,
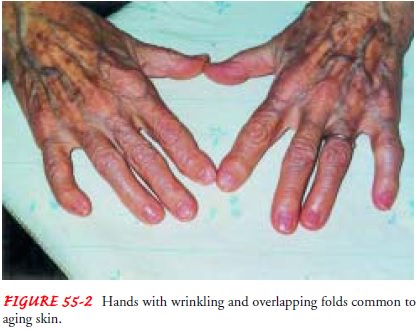
sags, and overlapping skin folds (Fig. 55-2).
Loss
of the subcutaneous tissue substances of elastin, collagen, and subcutaneous
fat diminishes the protection and cushioning of underlying tissues and organs,
decreases muscle tone, and re-sults in the loss of the insulating properties of
fat.
Cellular
replacement slows as a result of aging. As the dermal layers thin, the skin
becomes fragile and transparent. The blood supply to the skin also changes with
age. Vessels, especially the cap-illary loops, decrease in number and size.
These vascular changes contribute to the delayed wound healing commonly seen in
the elderly patient. Sweat and sebaceous glands decrease in number and
functional capacity, leading to dry and scaly skin. Reduced hormonal levels of
androgens are thought to contribute to declin-ing sebaceous gland function.
Hair
growth gradually diminishes, especially over the lower legs and dorsum of the
feet. Thinning is common in the scalp, ax-illa, and pubic areas. Other
functions affected with normal aging include the barrier function of skin,
sensory perception, and ther-moregulation.
Photoaging, or damage from excessive sun exposure,
has detri-mental effects on the normal aging of skin. A lifetime of outdoor
work or outdoor activities (eg, construction work, lifeguarding, sunbathing)
without prudent use of sunscreens can lead to pro-found wrinkling; increased
loss of elasticity; mottled, pigmented areas; cutaneous atrophy; and benign or
malignant lesions.
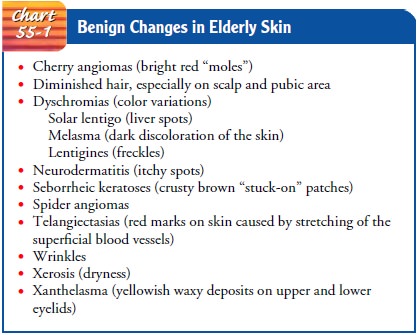
Many skin lesions are part of normal aging. Recognizing these lesions enables the examiner to assist the patient to feel less anx ious about changes in skin. Chart 55-1 summarizes some skin le-sions that are expected to appear as the skin ages. These are normal and require no special attention unless the skin becomes infected or irritated.
Related Topics