Chapter: Ophthalmology: Eye Optics and Refractive Errors
Eye Optics and Refractive Errors
Optics and Refractive Errors
Basic Knowledge
Uncorrected and Corrected Visual Acuity
Uncorrected visual acuity:
This refers to the resolving power of the eyewithout corrective
lenses.
Corrected visual acuity:
This refers to the resolving power of the eye with anoptimal
correction provided by corrective lenses (determined by visual acu-ity
testing).
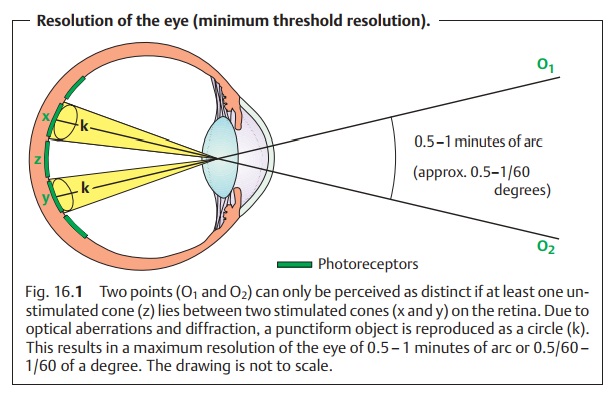
Both uncorrected visual acuity and corrected
visual acuity provide infor-mation on how far apart two objects must be for the
eye to perceive them as distinct objects (minimum threshold
resolution). For the eye to
perceive two objects as distinct, at least one unstimulated cone must lie
between two stimulated cones on the retina. The cone density is greatest in the
center of the retina and central visual acuity is highest. There the cones are spaced only
2.5 µm apart. This interval increases toward the periphery of the
retina, and both uncorrected visual acuity and corrected visual acuity decrease
accordingly. Cone spacing and physical effects such as diffraction and optical
aberrations limit the average minimum threshold resolution, the minimumvisual angle to one minute of arc (the individual maximum value is
approxi-mately 30 seconds of arc). One minute of arc is 1/60 of a degree or
approxi-mately 0.004 mm, which is somewhat more than the width of a cone. This
corresponds to the maximum resolving power of the retina (Fig. 16.1).
Refraction: Emmetropia and Ametropia
Refraction is defined as the ratio of the
refractive power of the lens and cornea (the refractive media) to the axial
length of the globe. Emmetropia is distin-guished from ametropia.
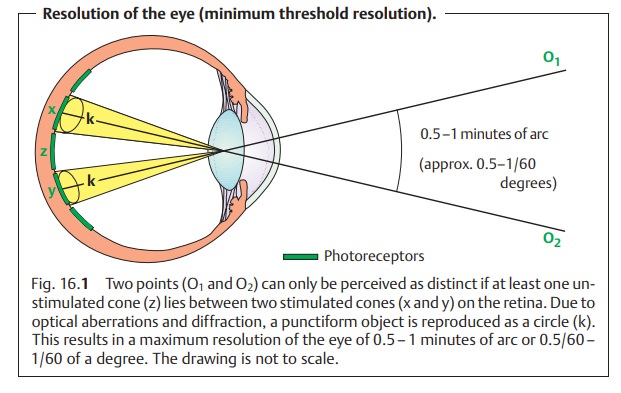
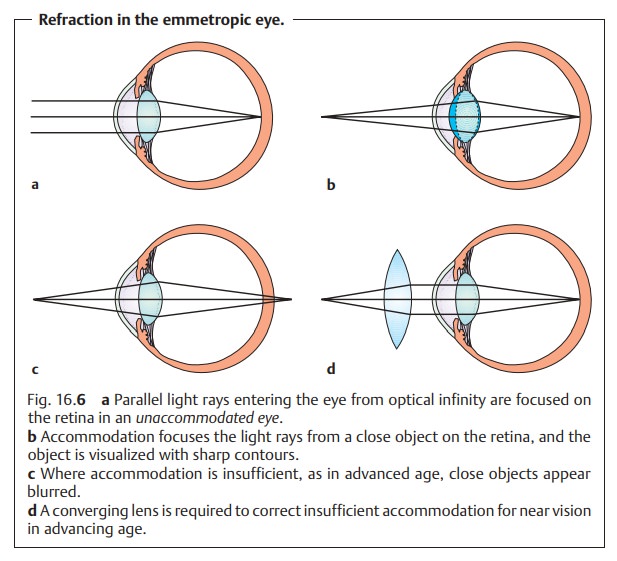
Emmetropia (normal sight):
The ratio of the axial length of the eye to therefractive power of the cornea and lens is balanced. Parallel light rays that enter the eye therefore meet at a focal point on the retina (Figs. 16.2 and 16.6a) and not anterior or posterior to it, as is the case in ametropia.
Ametropia (refractive error):
There is a mismatch between the axial lengthof the eye and the
refractive power of the lens and cornea. The ametropia is either axial, which is common, or refractive, which is less frequently
encoun-tered. The most common disorders are nearsightedness, farsightedness,
and astigmatism.
Very few people have refraction of exactly !0.0 diopters. Approximately 55% of persons between the ages of
20 and 30 have refraction between + 1 and –1 diopters.
Emmetropia is not necessarily identical to
good visual acuity. The eye may have other disorders that reduce visual acuity,
such as atrophy of the optic nerve or amblyopia.
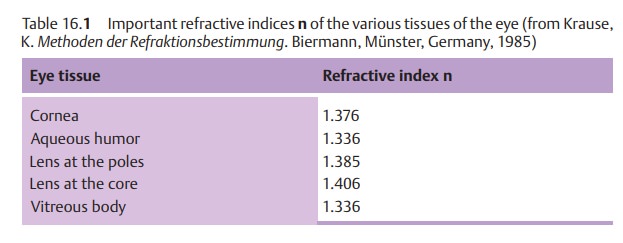
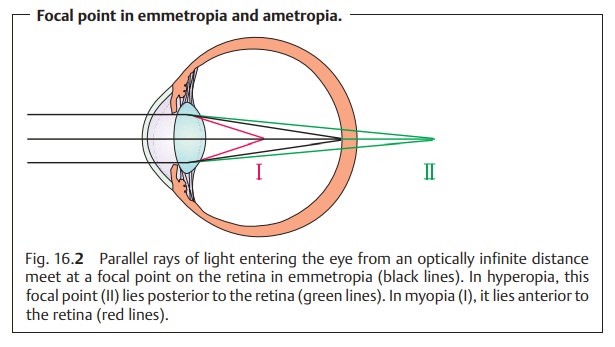
The refractive power of an optical lens system
is specified in diopters, which are
the international units of measure. Refractive power is calculated accord-ing
to the laws of geometric optics. According to Snell’s law, the refraction of the incident light ray is
determined by the angle of incidence and difference in the refractive indices n of the two media
(Table 16.1).
The maximum total refractive power of
an emmetropic eye is 63 diopters with an axial length of the globe measuring 23.5
mm. The cornea accounts for 43 diopters and the lens for 10 – 20 diopters,
depending on accommodation. However, the refractive power of the eye is not
simply the sum of these two values. The optic media that surround the eye’s
lens system and the distance between the lens and cornea render the total
system more complex.
The refractive power D (specified in diopters)
of an optical system is the reciprocal of the focal length of a lens f
(specified in meters). This yields the equation: D = 1/f.
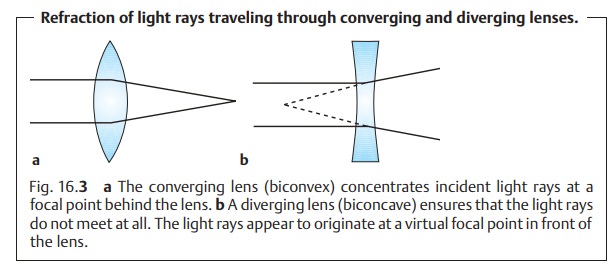
Example: Where a lens focuses parallel incident light rays 0.5 mbehindthelens, the refractive power is
1/0.5 m = + 2 diopters. This is a converging lens. Where the virtual focal
point is in front of the lens, the
refractive power is 1/–0.5 m = –2 diopters. This is a diverging lens (Fig. 16.3).
Accommodation
The refractive power of the eye described in the previous section is not a con-stant value. The eye’s refractive power must alter to allow visualization of both near and distant objects with sharp contours. This accommodation is made possible by the elasticity of the lens.
Accommodation mechanisms:
Accommodation involves the lens, zonulefibers, and ciliary
muscle.
❖ Lens: The soluble proteins of the lens are surrounded by a thin
elastic cap-sule. The curvature of the posterior capsule of the lens is greater
than its anterior curvature, with a posterior radius of 6.0 mm as opposed to an
anterior radius of 10.0 mm. The intrinsic
elasticity of the lens capsule tends to make the lens assume a spherical
shape. However, in the unaccommo-dated state this is prevented by the pull of
the zonule fibers. The elasticity of the inner tissue of the lens progressively
decreases with age due to deposits of insoluble proteins.
❖ Zonule fibers: The radiating zonule fibers insert into the equator of thelens
and connect it to the ciliary body. They hold the lens securely in posi-tion
and transmit the pull of the ciliary muscle to the lens.
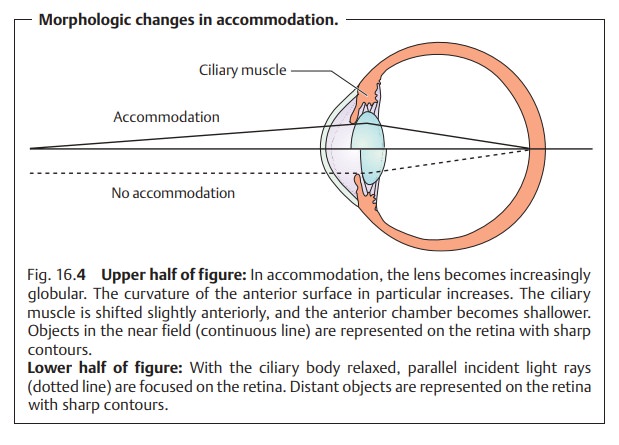
❖Ciliary muscle: Contraction of the ring-shaped ciliary muscledecreases thetension in the zonule fibers. The
lens can then approach the spherical shape (with a radius of curvature of 5.3
mm) that its physical configuration and chemical composition would otherwise
dictate. This change in the curvature of the lens is especially pronounced in
its anterior surface. The deformation increases
the refractive power; the focus of the eye shifts to the near field (Fig.
16.4), and close objects take on
sharp contours. As the ciliarymuscle
relaxes, the tension on the lens increases and the lens flattens.
Theresulting decrease in refractive power
shifts the focus of the eye into the distance (Fig. 16.4), and distant objects take on sharp contours.
The ciliary muscle is innervated by the short ciliary nerves, postganglionic parasympathetic fibers of the oculomotor nerve. Parasympatholytics such as atropine, scopolamine, and cyclopentolate inhibit the function of the ciliary muscle and therefore prevent accommodation. Referred to as cycloplegics, these medications also cause mydriasis by inhibiting the sphincter pupillae.
Parasympathomimetics such
as pilocarpine cause the ciliary muscle andsphincter pupillae to contract,
producing miosis.
When the ciliary muscle is at rest, the zonule fibers are under
tension and the eye focuses on distant objects.
Accommodation is regulated by a control loop. The control variable is
the sharpness of the retinal image. The system presumably uses the color
disper-sion of the retinal image to determine the direction in which
accommodation should be corrected.
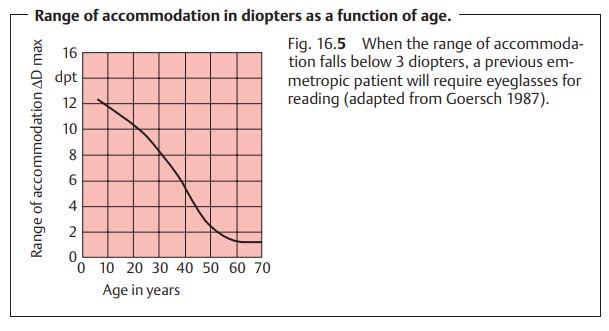
Range of accommodation:
This specifies themaximum
increase in refractivepower that is possible by accommodation in diopters
(Fig. 16.5). In mathemati-cal terms,
the range of accommodation is obtained by subtracting near-point refractive
power from far-point refractive power. The near
point is shortest distance that allows focused vision; the far point describes the farthest point
that is still discernible in focus. The near and far points define the range of
accommodation; its specific location in space is a function of the refractive
power of the eye.
Example: In one patient, the near point lies at 0.1 m and the far point
at 1 m.This patient’s range of accommodation is then 10 diopters –1 diopter = 9
diopters.
In an emmetropic eye, the far point is at
optical infinity. However, accom-modation can also bring near-field objects
into focus (Fig. 16.6b). The elastic-ity of the lens decreases with increasing age,
and the range of accommodation decreases accordingly (Fig. 16.5). Presbyopia (physiologic loss of accommo-dation in advancing age) begins
when the range of accommodation falls
below3 diopters. The gradual loss of accommodation causes the near point
torecede; that patient’s arms become “too short for reading”. Depending on age
and limitation of accommodation, presbyopia can be compensated for with
converging lenses of 0.5 – 3 diopters (see Fig. 16.6c and d).
Adaptation to Differences in Light Intensity
Like a camera, the eye’s aperture and lens
system also automatically adapts to differences in light intensity to avoid
“overexposure”. This adjustment is effected by two mechanisms.
1. The iris acts as an
aperture to control the amount of light entering the eye. This regulation takes about one second and
can change the light inten-sity on the retina over a range of about a power of
ten.
2. The sensitivity of the retina changes to adapt to differences in light inten-sity.
The sensitivity of the retina to light is a function of the concentration ofphotopigment in the
photoreceptors and of the neuronal
activity of the reti-nal cells. The change in neuronal activity is a rapid
process that takes only afew milliseconds and can alter the light sensitivity
of the retina over a range of three powers of ten. The change in the
concentration of photopig-ment takes several minutes but can cover a wide range
of retinal light sen-sitivity, as much as eight powers of ten.
Related Topics