Chapter: Basic Radiology : Imaging of Joints
Exercise: Arthritides
EXERCISE 7-4.
ARTHRITIDES
7-12.The frontal pelvis view for Case 7-12 (Figure 7-34) shows all of
the following features except
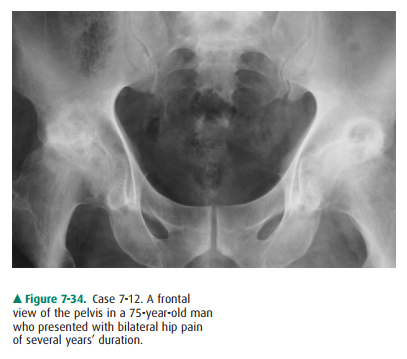
A.
A.loss of articular space.
B.
B.geode formation.
C.
C.juxtaarticular osteopenia.
D.
bony sclerosis.
7-13.The hands of the 45-year-old woman in Case 7-13 (Figure 7-35)
show soft-tissue calcifications that are most consistent with a diagnosis of

A.
A.osteoarthritis.
B.
B.scleroderma.
C.
C.systemic lupus erythematosus
(SLE).
D.
psoriasis.
7-14.The radiograph of the right hip in Case 7-14 (Figure7-36) is
most compatible with
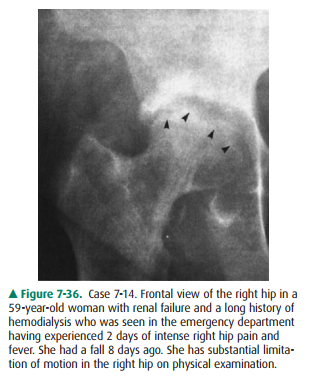
A.
A.osteoarthritis.
B.
B.gout.
C.
C.septic arthritis.
D.
scleroderma.
7-15. The imaging
findings for Case 7-15, at the first metatarsal phalangeal joint (Figure 7-37),
are most likely due to
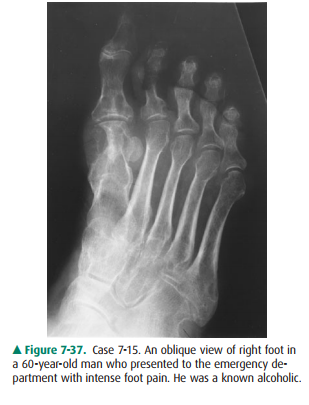
A.
scleroderma.
B.
ankylosing spondylitis.
C.
gout.
D.
osteoarthritis.
7-16. The linear
ossification connecting the cervical verte-bral bodies in Case 7-16 (Figure
7-38) are called
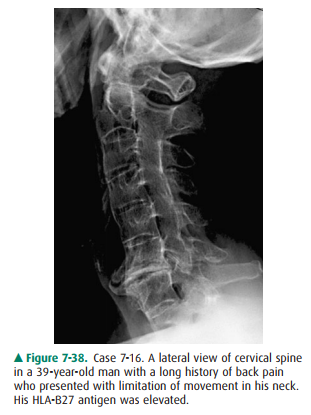
A.
osteophytes.
B.
erosions.
C.
soft-tissue swelling.
D.
syndesmophytes.
7-17. The “pencil-in-cup”
deformity of the interphalangeal joint of the thumb in Case 7-17 (Figure 7-39)
is most compatible with a diagnosis of
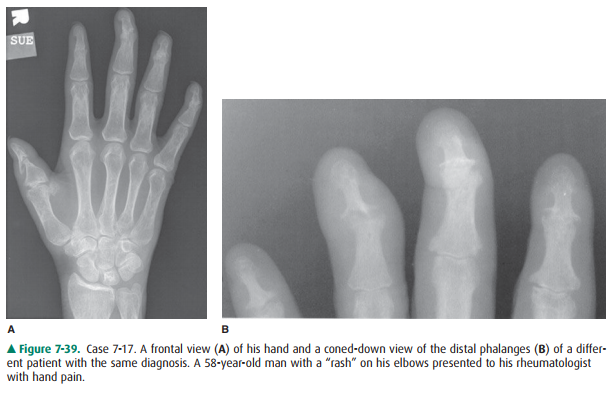
A.
psoriasis.
B.
gout.
C.
ankylosing spondylitis.
D.
SLE.
Radiologic Findings
7-12. The frontal
radiograph of both hips in this case (Fig-ure 7-34) shows articular space
narrowing, sclerosis, and subchondral cyst formation (also called geodes) bilaterally.
There is no significant juxtaarticular os-teopenia (C is the correct answer to
Question 7-12). The findings are most compatible with bilateral os-teoarthritis
(OA) of the hips.
7-13. In this case
(Figure 7-35), the most prominent fea-ture of this lady’s hand is soft-tissue
calcification and
7-16. The lateral view of
the cervical spine in Figure 7-38 shows prominent thin vertically oriented
connec-tions between the anterior aspects of the vertebral bodies and fusion of
the posterior elements of the spine. The thin vertically oriented ossifications
are lo-cated anatomically in the outer layers of the annulus fibrosis and
represent syndesmophytes that are asso-ciated with ankylosing spondylitis (D is
the correct answer to Question 7-16).
7-17. Figure 7-39 shows a
distinct “pencil-in-cup” erosion of the interphalangeal joint of the thumb and
severe joint space loss of the distal interphalangeal (DIP) joints with bony
ankylosis of the second, third, and fifth DIP joints. Fine periostitis is
evident around some of the erosions. Theses findings are most com-patible with
a diagnosis of psoriasis (A is the correct answer to Question 7-17).
Discussion
Osteoarthrosis (Osteoarthritis)
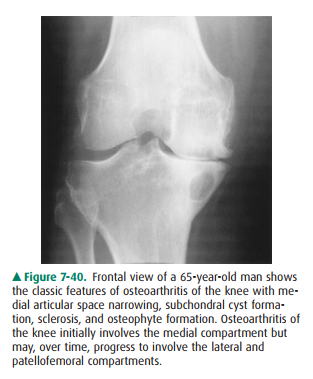
The frontal view of the pelvis of
Case 7-12 (Figure 7-34) shows the classic findings of osteoarthritis. These
include joint space narrowing resulting in cartilage loss, subchondral cysts,
and os-teophyte formation. The findings of osteoarthritis are similar inall
joints. In the knee, the articular space narrowing typically in-volves the
medial compartment initially (Figure 7-40) but may progress to involve the
lateral and patellofemoral compart-ments. In the hands, the articular space
narrowing typically in-volves the distal interphalangeal joints. Another
classic “target area” of osteoarthritis in the hand is the first CMC
(car-pometacarpal joint) and the STT (scaphotrapezo-trapezoidal) joint. There
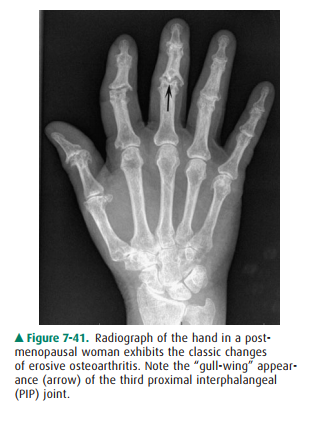
is a variant of osteoarthritis called erosive os-teoarthritis. Erosive
osteoarthritis usually affects post-menopausal women and can be confused with
rheumatoid arthritis. However, erosive arthritis usually affects the distal
in-terphalangeal joints and exhibits predominately subchondral or central
erosions as opposed to the marginal erosions seen in rheumatoid arthritis.
These central or subchondral erosions have the classic “gull wing” appearance
as shown at the proxi-mal interphalangeal joint of the third digit (Figure
7-41).
Connective Tissue Diseases and Seronegative Spondyloarthropathies
Generally, in the clinical
setting of polyarticular stiffness and pain, conventional radiographs are used
as the initial survey of the affected joints. These images target the most
common regions of involvement and usually include films of the hands, wrists,
pelvis, knee, feet, and ankles. The findings on these studies, coupled with the
ESR value and other laboratory tests, should indicate whether a
connective-tissue disorder is the cause of the arthropathy. Often patients will
be tested for rheumatoid factor (discussed in the next paragraph). If this test
is negative and the patient has symptoms involving the peripheral joints and
spine, then a “seronegative spondy-loarthropathy” is considered.
Perhaps the most common and
characteristic connective tissue disease producing arthritis is rheumatoid
arthritis (RA). Females (especially middle-aged women) are more commonly
affected by this disease than men. RA is thought to be a mal-function of the
immune system, and patients with this disorder usually produce a measurable
immune complex called rheuma-toid factor (RF). They also characteristically
have an elevated ESR. The disease often progresses in a symmetrical fashion.
The major initial pathologic process in RA is a synovitis that pro-duces
periarticular osteopenia because of the associated hyper-emia. Later in the
disease, synovial proliferation with pannus formation may then cause erosions
in the juxtaarticular regions (the so-called bare areas). These erosions occur
at the margins of the joint where the bony cortex and synovium contact each
other without interposition of articular cartilage. The articular cartilage
provides some protection from erosion in the early stages of the disease.
Subsequently, the disease may progress to secondary degenerative changes and
eventually to fibrous or bony ankylosis of the joint. In the wrist, the carpal
bones will show osteopenia, carpal crowding, or subluxations. In fact, the
ulnar styloid is often one of the first sites of erosions and “pen-ciling.”
Juxtaarticular osteopenia is seen in the bones of the hands and wrists.
Symmetric swelling at the proximal interpha-langeal joints of the hand is
present, and the articular surfaces show erosions, especially at the
metacarpophalangeal and prox-imal interphalangeal joints (Figure 7-42).

Systemic lupus erythematosus
(SLE) is a connective-tis-sue disorder that can be seen in conjunction with
other con-nective tissue diseases (the “overlap syndrome”). Patients with SLE
may show profound osteopenia, including resorp-tion of the tufts, but it does
not characteristically result in erosions. The typical appearance is of joint
instability with multiple subluxations at the wrists and metacarpophalangeal
joints. In fact, SLE is the most common cause of a nonerosive subluxing
arthropathy (Figure 7-43). Subluxations also occur in RA, but the distinguishing
factor is that the subluxations in RA are associated with the “bare area”
erosions.

Scleroderma (also called
progressive systemic sclerosis or PSS) is a disorder characterized by fibrosis
and skin thicken-ing. Soft-tissue calcification is a prominent feature of this
disorder. The major effects of this disease are not on the joints per se, but
are secondary to the diffuse sclerosis with resultant joint stiffness for which
the patient may seek treat-ment initially. About 10% of patients with PSS have
synovi-tis that is indistinguishable from RA at presentation, and many of these
patients eventually develop Raynaud’s phe-nomenon. The typical imaging findings
are periarticular cal-cification and resorption of the terminal phalangeal
tufts (acroosteolysis). Scleroderma may also be associated with other
connective disorders such as rheumatoid arthritis and SLE in the same
individual.
Psoriasis, Reiter’s disease,
ankylosing spondylitis, and in-flammatory bowel disease comprise the major
seronegative spondyloarthropathies. Psoriasis is a connective tissue disor-der
that primarily affects the skin. However, about 15% of pa-tients with psoriasis
develop bone and joint changes, and these findings may be the initial
manifestations of the disease. Radiographic findings of psoriasis include
periosteal reaction(periostitis) and/or focal cortical thickening in the
digits. The earliest manifestation of the disease is juxtaarticular osteopenia
that is less profound than in RA. The disease may then progress to show erosions
at the articular sur-faces. The distribution of these findings in psoriasis is
mainly the distal interphalangeal joints, unlike the findings in patients with
RA, which are predominately in the proxi-mal interphalangeal joints,
metacarpophalangeal joints, and carpus. The “pencil-in-cup” erosion seen in
Figure 7-39 is typical of psoriasis. Patients with psoriasis and other
seronegative spondyloarthropathies also develop ab-normalities of the spine and
sacroiliac joints (hence, the term spondyloarthropathy).
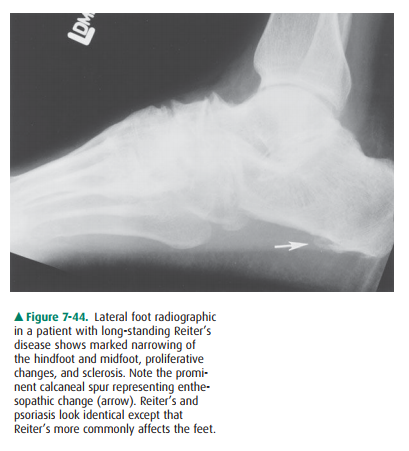
Reiter’s disease is a
postinfective disorder of the immune system that is characterized by the triad
of non-gonococcal urethritis, conjunctivitis/iritis, and arthritis. Seen most
fre-quently in male patients, Reiter’s disease was originally thought to be caused
by Chlamydia, but other organisms,
in-cluding Escherichia coli and Salmonella organisms, have also been
implicated. The imaging findings of Reiter’s disease are often
indistinguishable from those of psoriatic arthritis ex-cept that Reiter’s
disease most commonly affects the feet and psoriasis most commonly affects the
hands. Both diseases show periostitis, erosions, and enthesopathic changes. An en-thesis is an area of attachment of a
ligament or tendon to bone by the
perforating fibers of Sharpey. An enthesopathy is, therefore, an abnormality at
this site and is seen on the radi-ograph as bony excrescences in these areas. A
typical example of enthesopathy in Reiter’s disease is the bony excrescence on
the inferior aspect of the calcaneus, which develops at the site of attachment
of the plantar fascia and the short flexors in the foot (Figure 7-44).
Ankylosing spondylitis (AS) is a
rheumatic disease causing arthritis of the spine and sacroiliac joints and can
cause in-flammation of the eyes, lungs, and heart valve. The typical clin-ical
scenario is intermittent back pain that occurs throughout life. The pain may
progress to severe chronic disease attacking the spine, peripheral joints, and
other organs resulting in marked loss of motion and deformity over time. The
cause of AS is not known, but most of the spondyloarthritides share a common
genetic marker called the HLA-B27 antigen. The dis-ease usually presents in the
adolescent and young adults and is most common in Native Americans.
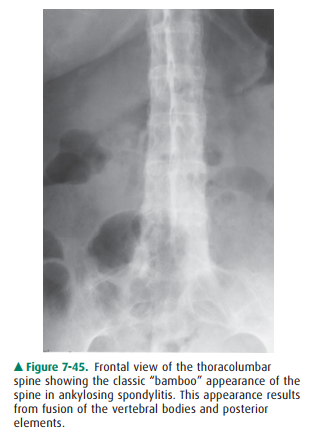
Figure 7-38 shows the typical
features of AS in the cervi-cal spine. The thin vertically oriented
ossifications connect-ing the vertebral bodies, syndesmophytes, are
anatomically located in the outer layers of the annulus fibrosis. Also typical
in this case is the fusion of the posterior elements. In fact, the classic
appearance of AS is the “bamboo spine” (Figure 7-45). This appearance is caused
by fusion of all the synovial joints of the spine and predisposes the patient
to the development of fractures (insufficiency type fractures). This
insufficiency fracture (which may lead to a “pseudoarthrosis”) is a
well-documented complication of ankylosing spondylitis.
The mainstay of treatment for AS is nonsteroidal anti-inflammatory medication to control pain. However, some patients with severe disease may be given methotrexate.
Septic Arthritis
Septic arthritis is usually
blood-borne (hematogenous) and is most commonly monoarticular (that is,
involving only one joint at any time). A common cause of septic arthritis in
the adult is Staphylococcus aureus,
although other infective agents including Streptococcus,
Gonococcus, and other gram-negative
organisms may also be encountered. Streptococcus
and gram-negative organisms are particularly important in the pediatric age
group. Also, tuberculosis has been recently encoun-tered with greater
frequency, especially in patients who are immunocompromised.
The radiographic examination of
the patient in Case 7-14 (Figure 7-36) provides general anatomic information,
helps to determine whether further imaging is necessary, and aids in deciding
whether further intervention is appropriate. Her physicians were very worried
about septic arthritis in this clinical setting of previous renal transplant
(ie, relatively im-munocompromised), and a hip aspiration was requested. Twenty
milliliters of bloodstained turbid fluid was aspirated and was sent to the
microbiology laboratory for Gram’s stain, culture, and sensitivity studies. The
cultures grew Staphylo-coccus aureus,
a common pathogen in septic arthritis.
Figure 7-36 shows the classic
radiographic findings of sep-tic arthritis and osteomyelitis. These include articular
space narrowing, erosion of bone on both sides of the joint, and sclerosis. An
effusion is typically present and can be identified by ultrasound or MR
imaging. In addition, MR imaging can be useful if abscesses are suspected in
the adjacent soft tissues. Septic joints will exhibit increased uptake on bone
scan be-cause of the marked hyperemia and bony proliferation.
Crystal Deposition Diseases
Gout, a disorder more common in
middle-aged men, is an inflammatory arthritis caused by abnormal deposition of
urates (called tophi) in the soft tissues and cartilage. These deposits cause
episodic joint inflammation and are associ-ated with pain and disability. In
the earlier stages of the dis-ease, radiographs of the bone and joints may be
normal except for soft-tissue swelling and in some instances soft-tissue
calcification. The initial classic clinical presentation of gout is podagra, an
acute inflammation of a joint, often the first metatarsal phalangeal joint
(Figure 7-37). At presenta-tion, the patient will have severe joint pain, and
the overlying soft tissues will be swollen and red. With repeated attacks over
years, bony erosions with “overhanging edges” (or over-hanging margins) may
develop adjacent to the joint but not within the joint. When the patient is
severely incapacitated by pain and not moving the joint, “disuse” osteopenia
can be seen at radiography. The typical areas to screen for gout are the first
metatarsophalangeal joint, the heel, the back of the elbow joint (olecranon
fossa), and the hands and wrists. Screening for elevated serum levels of uric
acid and joint as-piration are the best ways to confirm the clinical suspicion
of gout after obtaining conventional radiographs. The joint as-pirate will show
birefringent uric acid crystals in the synovial fluid on polarized light
microscopy.
Calcium pyrophosphate dehydrate
crystal deposition (CPPD) disease is another common crystal deposition joint
disorders. In CPPD disease, there is calcification in the fibrocartilage and
hyaline articular cartilage (so-called chon-drocalcinosis). The most common
association with chondro-calcinosis is aging, although it may also be seen in
pseudogout (CPPD disease), gout, ochronosis, hemochromatosis, and
hy-perparathyroidism. This finding is most commonly seen in the wrist,
symphysis pubis, or knee. So, if one suspects a patient of having CPPD,
radiographs of the pelvis, wrist, and knees would be a good start at screening
for it. The presence of calci-fication alone is not diagnostic of CPPD,
however. The clinical syndrome of pain from the presence of abnormal cartilage
cal-cification is referred to as the CPPD syndrome, and symptoms may be
provoked by various stresses (eg, surgical procedures). Confirmation of the
diagnosis may be obtained by identifica-tion of calcium pyrophosphate crystals
from synovial fluid ob-tained via percutaneous aspiration of the affected
joint.
Related Topics