Chapter: Medical Surgical Nursing: Assessment of Cardiovascular Function
Electrocardiography - Diagnostic Evaluation of Cardiovascular Function
ELECTROCARDIOGRAPHY
The
ECG is a diagnostic tool used in assessing the cardiovascular system. It is a
graphic recording of the electrical activity of the heart; an ECG can be
recorded with 12, 15, or 18 leads, showing the activity from those different
reference points. The ECG is obtained by placing disposable electrodes in
standard positions on the skin of the chest wall and extremities. The heart’s
electrical impulses are recorded as a tracing on special graph paper.
The
standard 12-lead ECG is the most commonly used tool to diagnose dysrhythmias,
conduction abnormalities, enlarged heart chambers, myocardial ischemia or
infarction, high or low calcium and potassium levels, and effects of some
medications. A 15-lead ECG adds 3 additional chest leads across the right
precordium and is a valuable tool for the early diagnosis of right ventricular
and pos-terior left ventricular infarction. The 18-lead ECG adds 3 poste-rior
leads to the 15-lead ECG and is very useful for early detection of myocardial
ischemia and injury (Wung & Drew, 1999). To en-hance interpretation of the
ECG, the patient’s age, gender, BP, height, weight, symptoms, and medications
(especially digitalis and antiarrhythmic agents) should be noted on the ECG
requisi-tion.
Continuous Electrocardiographic Monitoring
Continuous
ECG monitoring is standard for patients who are at high risk for dysrhythmias.
Two continuous ECG monitoring techniques are hardwire monitoring, found in
critical care units and specialty step-down units, and telemetry, found in
specialty step-down units and general nursing care units. Patients who are
receiving continuous ECG monitoring need to be informed of its purpose and
cautioned that this monitoring method will not de-tect symptoms such as dyspnea
or chest pain. Therefore, patients need to be advised to report symptoms to the
nurse whenever they occur.
HARDWIRE CARDIAC MONITORING
The
patient’s ECG can be continuously observed for dysrhyth-mias and conduction
disorders on an oscilloscope at the bedside or at a central monitoring station
by a hardwire monitoring sys-tem. This system is composed of three to five
electrodes posi-tioned on the patient’s chest, a lead cable, and a bedside
monitor. Hardwire monitoring systems vary in sophistication but in gen-eral can
do the following:
·
Monitor more than one lead
simultaneously
·
Monitor ST segments (ST-segment
depression is a marker of myocardial ischemia; ST-segment elevation provides
evidence of an evolving MI)
·
Provide graded visual and audible
alarms (based on prior-ity, asystole would be highest)
·
Computerize rhythm monitoring
(dysrhythmias are inter-preted and stored in memory)
·
Print a rhythm strip
·
Record a 12-lead ECG
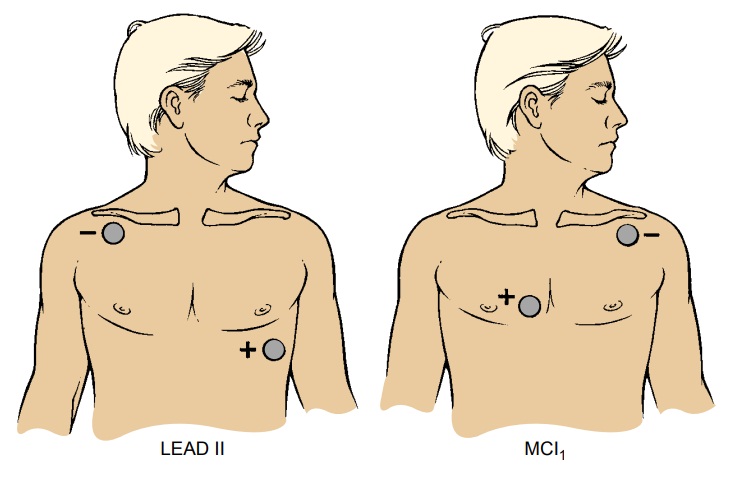
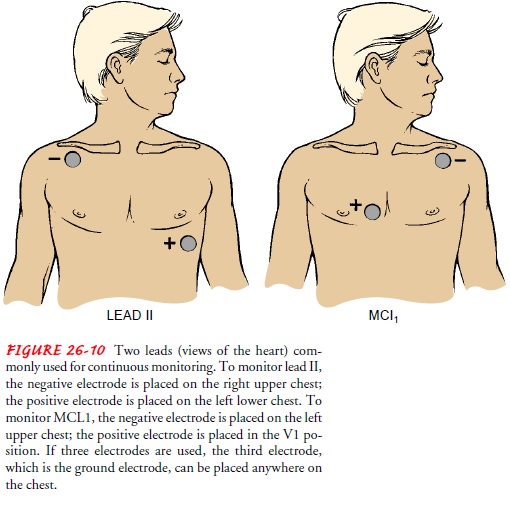
Two
leads commonly used for continuous monitoring are leads II and V1 or a
modification of V1 (MCL1) (Fig. 26-10). Lead II provides the best visualization
of atrial depolarization (represented by the P wave). Leads V1 and MCL1 best
visualize the ventricle responsible for ectopic or abnormal ventricular beats.
TELEMETRY
In
addition to hardwire monitoring systems, the ECG can be continuously observed
by telemetry, the transmission of
radio-waves from a battery-operated transmitter worn by the patient to a
central bank of monitors. Although telemetry systems have the same capabilities
as hardwire systems, they are wireless, al-lowing the patient to ambulate while
being monitored. Following the guidelines for electrode placement will ensure
good conduc-tion and a clear picture of the patient’s rhythm on the monitor:
·
Clean the skin surface with soap and
water and dry well (or as recommended by the manufacturer) before applying the
electrodes. If the patient has much hair where the electrodes need to be
placed, shave or clip the hair.
·
Apply a small amount of benzoin to
the skin if the patient is diaphoretic (sweaty) and the electrodes do not
adhere well.
·
Change the electrodes every 24 to 48
hours and examine the skin for irritation. Apply the electrodes to different
locations each time they are changed.
·
If the patient is sensitive to the
electrodes, use hypoaller-genic electrodes.
SIGNAL-AVERAGED ELECTROCARDIOGRAM
For
some patients who are considered to be at high risk for sudden cardiac death, a
signal-averaged ECG is performed. This high-resolution ECG assists in
identifying the risk for life-threatening dysrhythmias and helps to determine
the need for invasive diag-nostic procedures. Signal averaging works by
averaging about 150 to 300 QRS waveforms (QRS waveforms represent
depolarization of the ventricle). The resulting averaged QRS complex is analyzed
for certain characteristics that are likely to lead to lethal ventric-ular
dysrhythmias. The recording is performed at the bedside and requires about 15
minutes.
CONTINUOUS AMBULATORY MONITORING
In
ambulatory ECG monitoring, which may occur in the hos-pital but is more
commonly prescribed for outpatients, one lead of the patient’s ECG can be
monitored by a Holter monitor. This monitor is a small tape recorder that
continuously (for 10 to 24 hours) documents the heart’s electrical activity on
a mag-netic tape. The tape recorder weighs approximately 2 pounds and can be
carried over the shoulder or worn around the waist day and night to detect
dysrhythmias or evidence of myocardial ischemia during activities of daily
living. The patient keeps a diary of activity, noting the time of any symptoms,
experiences, or unusual activities performed. The tape recording is then
exam-ined with a special scanner, analyzed, and interpreted. Evidence obtained
in this way helps the physician diagnose dysrhythmias and myocardial ischemia
and evaluate therapy, such as anti-arrhythmic and antianginal medications or
pacemaker function.
TRANSTELEPHONIC MONITORING
Another
method of evaluating the ECG of a patient at home is by transtelephonic
monitoring. The patient attaches a specific lead system for transmitting the
signals and places a telephone mouthpiece over the transmitter box; the ECG is
recorded and evaluated at another location. This method is often used for
di-agnosing dysrhythmias and in follow-up evaluation of permanent cardiac
pacemakers.
Related Topics