Chapter: Medical Physiology: Aviation, High-Altitude, and Space Physiology
Effects of Low Oxygen Pressure on the Body
Effects of Low Oxygen Pressure on the Body
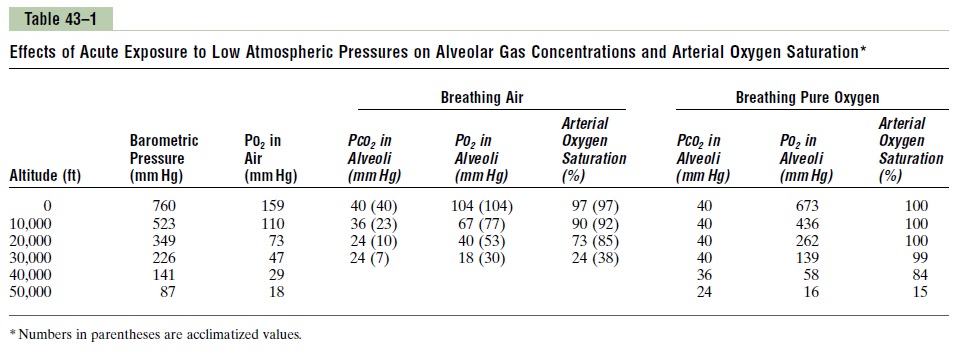
Barometric Pressures at Different Altitudes. Table 43–1 gives the approximatebaro-metric and oxygen pressures at different altitudes, showing that at sea level, thebarometric pressure is 760 mm Hg; at 10,000 feet, only 523 mm Hg; and at 50,000 feet, 87 mm Hg. This decrease in barometric pressure is the basic cause of all the hypoxia problems in high-altitude physiology because, as the baro-metric pressure decreases, the atmospheric oxygen partial pressure decreases proportionately, remaining at all times slightly less than 21 per cent of the total barometric pressure—PO2 at sea level about 159 mm Hg, but at 50,000 feet only 18 mm Hg.
Alveolar PO2 at Different Elevations
Carbon Dioxide and Water Vapor Decrease the Alveolar Oxygen. Even at high altitudes,carbon dioxide is continually excreted from the pulmonary blood into the alveoli. Also, water vaporizes into the inspired air from the respiratory surfaces. These two gases dilute the oxygen in the alveoli, thus reducing the oxygen con-centration. Water vapor pressure in the alveoli remains 47 mm Hg as long as the body temperature is normal, regardless of altitude.
In the case of carbon dioxide, during exposure to very high altitudes, the alveolar PCO2 falls from the sea-level value of 40 mm Hg to lower values. In the acclimatized person, who increases his or her ventilation about fivefold, the PCO2falls to about 7 mm Hg because of increased respiration.
Now let us see how the pressures of these two gases affect the alveolar oxygen. For instance, assume that the barometric pressure falls from the normal sea-level value of 760 mm Hg to 253 mm Hg, which is the usual measured value at the top of 29,028–foot Mount Everest. Forty-seven millimeters of mercury of this must be water vapor, leaving only 206 mm Hg for all the other gases. In the acclimatized person, 7 mm of the 206 mm Hg must be carbon dioxide, leavingonly 199 mm Hg. If there were no use of oxygen by the body, one fifth of this 199 mm Hg would be oxygen and four fifths would be nitrogen; that is, the PO2 in the alveoli would be 40 mm Hg. However, some of this remaining alveolar oxygen is continually being absorbed into the blood, leaving about 35 mm Hg oxygen pressure in the alveoli. At the summit of Mount Everest, only the best of acclimatized people can barely survive when breathing air. But the effect is very different when the person is breathing pure oxygen, as we see in the fol-lowing discussions.
Alveolar PO2 at Different Altitudes. The fifth column of Table 43–1 shows the approximate PO2s in the alveoli at different altitudes when one is breathing air for both the unacclimatized and the acclimatized person. At sea level, the alveolar PO2 is 104 mm Hg; at 20,000 feet alti-tude, it falls to about 40 mm Hg in the unacclimatized person but only to 53 mm Hg in the acclimatized. The difference between these two is that alveolar ventila-tion increases much more in the acclimatized person than in the unacclimatized person, as we discuss later.
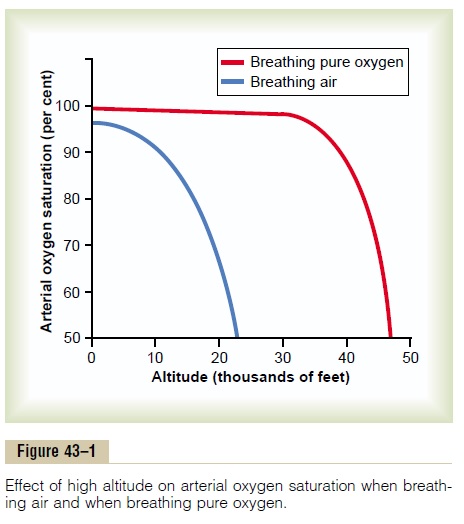
Saturation of Hemoglobin with Oxygen at Different Altitudes. Figure 43–1 shows arterial blood oxygen saturation at different altitudes while a person is breathing air and while breathing oxygen. Up to an altitude of about 10,000 feet, even when air is breathed, the arterial oxygen saturation remains at least as high as 90 per cent. Above 10,000 feet, the arterial oxygen saturation falls rapidly, as shown by the blue curve of the figure, until it is slightly less than 70 per cent at 20,000 feet and much less at still higher altitudes.
Effect of Breathing Pure Oxygen on Alveolar PO2 at Different Altitudes
When a person breathes pure oxygen instead of air, most of the space in the alveoli formerly occupied by nitrogen becomes occupied by oxygen. At 30,000 feet, an aviator could have an alveolar PO2 as high as 139 mm Hg instead of the 18 mm Hg when breathing air (see Table 43–1).
The red curve of Figure 43–1 shows arterial blood hemoglobin oxygen saturation at different altitudes when one is breathing pure oxygen. Note that the sat-uration remains above 90 per cent until the aviator ascends to about 39,000 feet; then it falls rapidly to about 50 per cent at about 47,000 feet.
The “Ceiling” When Breathing Air and When Breathing Oxygen in an Unpressurized Airplane
Comparing the two arterial blood oxygen satura-tion curves in Figure 43–1, one notes that an aviator breathing pure oxygen in an unpressurized airplane can ascend to far higher altitudes than one breathing air. For instance, the arterial saturation at 47,000 feet when one is breathing oxygen is about 50 per cent and is equivalent to the arterial oxygen saturation at 23,000 feet when one is breathing air. In addition, because an unacclimatized person usually can remain conscious until the arterial oxygen saturation falls to 50 per cent, for short exposure times the ceiling for an aviator in an unpressurized airplane when breathing air is about 23,000 feet and when breathing pure oxygen is about 47,000 feet, provided the oxygen-supplying equipment operates perfectly
Acute Effects of Hypoxia
Some of the important acute effects of hypoxia in the unacclimatized person breathing air, beginning at an altitude of about 12,000 feet, are drowsiness, lassitude, mental and muscle fatigue, sometimes headache, occa-sionally nausea, and sometimes euphoria.These effects progress to a stage of twitchings or seizures above 18,000 feet and end, above 23,000 feet in the unaccli-matized person, in coma, followed shortly thereafter by death.
One of the most important effects of hypoxia is decreased mental proficiency, which decreases judg-ment, memory, and performance of discrete motor movements. For instance, if an unacclimatized aviator stays at 15,000 feet for 1 hour, mental proficiency ordi-narily falls to about 50 per cent of normal, and after 18 hours at this level it falls to about 20 per cent of normal.
Acclimatization to Low PO2
A person remaining at high altitudes for days, weeks, or years becomes more and more acclimatized to the low PO2, so that it causes fewer deleterious effects on the body. And it becomes possible for the person to work harder without hypoxic effects or to ascend to still higher altitudes.
The principal means by which acclimatization comes about are (1) a great increase in pulmonary ventila-tion, (2) increased numbers of red blood cells, (3) increased diffusing capacity of the lungs, (4) increased vascularity of the peripheral tissues, and (5) increased ability of the tissue cells to use oxygen despite low PO2.
Increased Pulmonary Ventilation—Role of Arterial Chemore- ceptors. Immediate exposure to low PO2stimulates thearterial chemoreceptors, and this increases alveolar ventilation to a maximum of about 1.65 times normal. Therefore, compensation occurs within seconds for the high altitude, and it alone allows the person to rise several thousand feet higher than would be possible without the increased ventilation. Then, if the person remains at very high altitude for several days, the chemoreceptors increase ventilation still more, up to about five times normal.
The immediate increase in pulmonary ventilation on rising to a high altitude blows off large quantities of carbon dioxide, reducing the PCO2 and increasing the pH of the body fluids. These changes inhibit the brain stem respiratory center and thereby oppose the effectof low PO2 to stimulate respiration by way of the peripheral arterial chemoreceptors in the carotid and aortic bodies. But during the ensuing 2 to 5 days, thisinhibition fades away, allowing the respiratory center to respond with full force to the peripheral chemore-ceptor stimulus from hypoxia, and ventilation in-creases to about five times normal.
The cause of this fading inhibition is believed to be mainly a reduction of bicarbonate ion concentration in the cerebrospinal fluid as well as in the brain tissues. This in turn decreases the pH in the fluids surround-ing the chemosensitive neurons of the respiratory center, thus increasing the respiratory stimulatory activity of the center.
An important mechanism for the gradual decrease in bicarbonate concentration is compensation by the kidneys for the respiratory alkalosis. The kidneys respond to decreased PCO2 by reducing hydrogen ion secretion and increasing bicarbonate excretion. This metabolic compensation for the respiratory alkalosis gradually reduces plasma and cerebrospinal fluid bicarbonate concentration and pH toward normal and removes part of the inhibitory effect on respiration of low hydrogen ion concentra-tion. Thus, the respiratory centers are much more responsive to the peripheral chemoreceptor stimulus caused by the hypoxia after the kidneys compensate for the alkalosis.
Increase in Red Blood Cells and Hemoglobin Concentration During Acclimatization. As discussed, hypoxia is the principal stimulus for causing an increase in red blood cell production. Ordinarily, when a person remains exposed to low oxygen for weeks at a time, the hematocrit rises slowly from a normal value of 40 to 45 to an average of about 60, with an average increase in whole blood hemoglobin concentration from normal of 15 g/dl to about 20 g/dl.
In addition, the blood volume also increases, often by 20 to 30 per cent, and this increase times the increased blood hemoglobin concentration gives an increase in total body hemoglobin of 50 or more per cent.
Increased Diffusing Capacity After Acclimatization. It willbe recalled that the normal diffusing capacity for oxygen through the pulmonary membrane is about 21 ml/mm Hg/min, and this diffusing capacity can increase as much as threefold during exercise. A similar increase in diffusing capacity occurs at high altitude.
Part of the increase results from increased pul-monary capillary blood volume, which expands the capillaries and increases the surface area through which oxygen can diffuse into the blood. Another part results from an increase in lung air volume, which expands the surface area of the alveolar-capillary interface still more. A final part results from an increase in pulmonary arterial blood pressure; this forces blood into greater numbers of alveolar capil-laries than normally—especially in the upper parts of the lungs, which are poorly perfused under usual conditions.
Peripheral Circulatory System Changes During Acclimatiza-tion—Increased Tissue Capillarity. The cardiac outputoften increases as much as 30 per cent immediately after a person ascends to high altitude but then decreases back toward normal over a period of weeksas the blood hematocrit increases, so that the amountof oxygen transported to the peripheral body tissues remains about normal.
Another circulatory adaptation is growth ofincreased numbers of systemic circulatory capillaries in the nonpulmonary tissues, which is called in-creased tissue capillarity (or angiogenesis). This occurs especially in animals born and bred at high altitudes but less so in animals that later in life become exposed to high altitude.
In active tissues exposed to chronic hypoxia, the increase in capillarity is especially marked. For instance, capillary density in right ventricular muscle increases markedly because of the combined effects of hypoxia and excess workload on the right ventricle caused by pulmonary hypertension at high altitude.
Cellular Acclimatization. In animals native to altitudes of13,000 to 17,000 feet, cell mitochondria and cellular oxidative enzyme systems are slightly more plentiful than in sea-level inhabitants. Therefore, it is presumed that the tissue cells of high altitude–acclimatized human beings also can use oxygen more effectively than can their sea-level counterparts.
Natural Acclimatization of Native Human Beings Living at High Altitudes
Many native human beings in the Andes and in the Himalayas live at altitudes above 13,000 feet—one group in the Peruvian Andes lives at an altitude of 17,500 feet and works a mine at an altitude of 19,000 feet. Many of these natives are born at these altitudes and live there all their lives. In all aspects of acclima-tization, the natives are superior to even the best-acclimatized lowlanders, even though the lowlanders might also have lived at high altitudes for 10 or more years. Acclimatization of the natives begins in infancy. The chest size, especially, is greatly increased, whereas the body size is somewhat decreased, giving a high ratio of ventilatory capacity to body mass. In addition, their hearts, which from birth onward pump extra amounts of cardiac output, are considerably larger than the hearts of lowlanders.
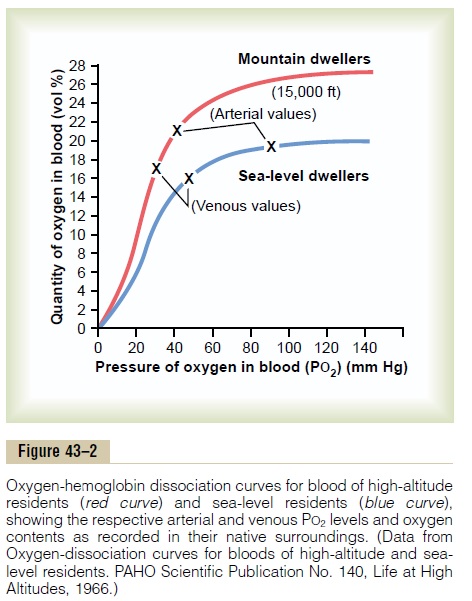
Delivery of oxygen by the blood to the tissues is also highly facilitated in these natives. For instance, Figure 43–2 shows oxygen-hemoglobin dissociation curves for natives who live at sea level and for their counterparts who live at 15,000 feet. Note that the arterial oxygen PO2 in the natives at high altitude is only 40 mm Hg, but because of the greater quantity of hemoglobin, the quantity of oxygen in their arterial blood is greater than that in the blood of the natives at the lower altitude. Note also that the venous PO2 in the high-altitude natives is only 15 mm Hg less than the venous PO2 for the lowlanders, despite the very low arterial PO2, indicating that oxygen transport to the tissues is exceedingly effective in the naturally acclimatized high-altitude natives.
Reduced Work Capacity at High Altitudes and Positive Effect of Acclimatization
In addition to the mental depression caused by hypoxia, as discussed earlier, the work capacity of all muscles is greatly decreased in hypoxia. This includes not only skeletal muscles but also cardiac muscles. In general, work capacity is reduced in direct proportion to the decrease in maximum rate of oxygen uptake that the body can achieve.
To give an idea of the importance of acclimatization in increasing work capacity, consider this: The work capacities as per cent of normal for unacclimatized and acclimatized people at an altitude of 17,000 feet are as follows:
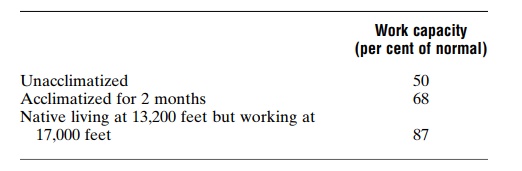
Thus, naturally acclimatized native persons can achieve a daily work output even at high altitude almost equal to that of a lowlander at sea level, but even well-acclimatized lowlanders can almost never achieve this result.
Acute Mountain Sickness and High-Altitude Pulmonary Edema
A small percentage of people who ascend rapidly to high altitudes become acutely sick and can die if not given oxygen or removed to a low altitude. The sick-ness begins from a few hours up to about 2 days after ascent. Two events frequently occur:
1.Acute cerebral edema. This is believed to resultfrom local vasodilation of the cerebral blood vessels, caused by the hypoxia. Dilation of the arterioles increases blood flow into the capillaries, thus increasing capillary pressure, which in turn causes fluid to leak into the cerebral tissues.
The cerebral edema can then lead to severe disorientation and other effects related to cerebral dysfunction.
2.Acute pulmonary edema. The cause of this is stillunknown, but a suggested answer is the following: The severe hypoxia causes the pulmonary arterioles to constrict potently, but the constriction is much greater in some parts of the lungs than in other parts, so that more and more of the pulmonary blood flow is forced through fewer and fewer still unconstricted pulmonary vessels. The postulated result is that the capillary pressure in these areas of the lungs becomes especially high and local edema occurs.
Extension of the process to progressively more areas of the lungs leads to spreading pulmonary edema and severe pulmonary dysfunction that can be lethal. Allowing the person to breathe oxygen usually reverses the process within hours.
Chronic Mountain Sickness
Occasionally, a person who remains at high altitude too long develops chronic mountain sickness, in which the following effects occur: (1) the red cell mass and hematocrit become exceptionally high, (2) the pul-monary arterial pressure becomes elevated even more than the normal elevation that occurs during acclima-tization, (3) the right side of the heart becomes greatly enlarged, (4) the peripheral arterial pressure begins to fall, (5) congestive heart failure ensues, and (6) death often follows unless the person is removed to a lower altitude.
The causes of this sequence of events are probably threefold: First, the red cell mass becomes so great that the blood viscosity increases severalfold; this increased viscosity tends to decrease tissue blood flow so that oxygen delivery also begins to decrease. Second, the pulmonary arterioles become vasoconstricted because of the lung hypoxia. This results from the hypoxic vascular constrictor effect that normally operates to divert blood flow from low-oxygen to high-oxygen alveoli. But because all the alveoli are now in the low-oxygen state, all the arteri-oles become constricted, the pulmonary arterial pres-sure rises excessively, and the right side of the heart fails. Third, the alveolar arteriolar spasm diverts much of the blood flow through nonalveolar pulmonary vessels, thus causing an excess of pulmonary shunt blood flow where the blood is poorly oxygenated; this further compounds the problem. Most of these people recover within days or weeks when they are moved to a lower altitude.
Related Topics