Chapter: Clinical Dermatology: Drug eruptions
Drug eruptions Treatment
Treatment
The
first approach is to withdraw the suspected drug, accepting that several drugs
may need to be stopped at the same time. This is not always easy as sometimes a
drug is necessary and there is no alternative available. At other times the
patient may be taking many drugs and it is difficult to know which one to stop.
The decision to stop or continue a drug depends upon the nature of the drug,
the necessity of using the drug for treatment, the availability of chemically
unrelated alternatives, the severity of the reaction, its potential
reversibility, and the probability that the drug is actu-ally causing the
reaction.
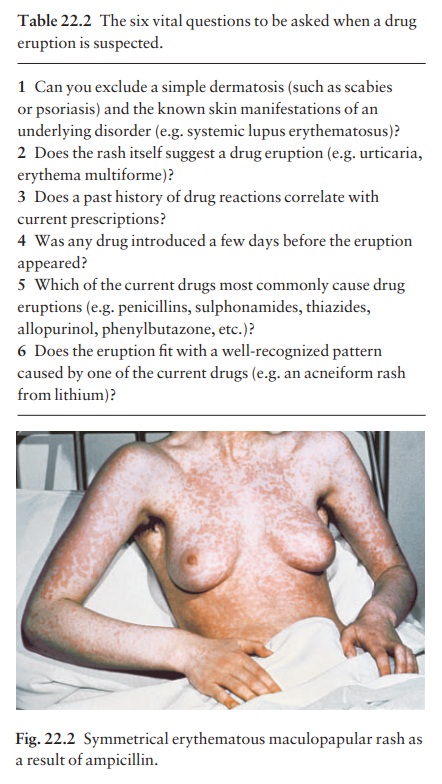
Assessment
depends upon clinical detective work (Table 22.2). Judgements must be based on
probabil-ities and common sense. Every effort must be made to correlate the
onset of the rash with prescription records. Often, but not always, the latest
drug to be introduced is the most likely culprit. Prick tests and invitro tests
for allergy are still too unreliable to be ofvalue. Re-administration, as a
diagnostic test, is usually unwise except when no suitable alternative drug
exists.
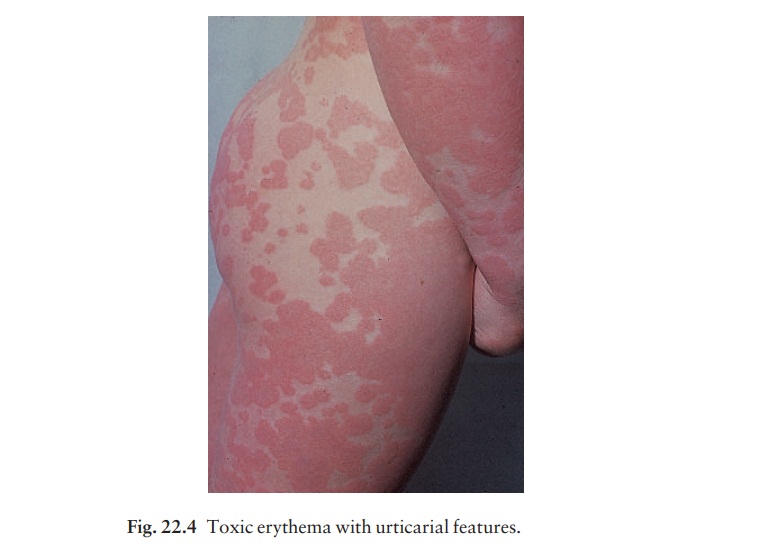
Non-specific
therapy depends upon the type of erup-tion. In urticaria, antihistamines are
helpful. In some reactions, topical or systemic corticosteroids can be used,
and applications of calamine lotion may be soothing.
Anaphylactic
reactions require special treatment (Fig. 22.4) to ensure that the airway is
not compromised (e.g. oxygen, assisted respiration or even emergency
tracheostomy). One or more injections of adrenaline (epinephrine) (1 : 1000)
0.3–0.5 mL should be given subcutaneously or intramuscularly in adults before
the slow (over 1 min) intravenous injection of chlor-phenamine maleate (10–20
mg diluted in syringe
with
5–10 mL of blood). Although the action of intra-venous hydrocortisone (100 mg)
is delayed for several hours it should be given to prevent further
deteriora-tion in severely affected patients. Patients should be observed for 6
h after their condition is stable, as late deterioration may occur. If an
anaphylactic reaction is anticipated, patients should be taught how to
self-inject adrenaline, and may be given a salbutamol inhaler to use at the
first sign of the reaction.
To
re-emphasize, the most important treatment is to stop the responsible drug.
Desensitization, seldom advisable or practical, may rarely be carried out when
therapy with the incriminated drug is essential and when there is no suitable
alternative (e.g. with some anticonvulsants, antituberculous and antileprotic
drugs). An expert, usually a physician with consider-able experience of the
drug concerned, should super-vise desensitization.
Related Topics